- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; sp: e1. DOI 10.35630/2022/12/sp.iss.2
In the case of gunshot wounds to the limbs, 7.1% of wounded servicemen are diagnosed with primary defects of bone tissue, which in 79.3% of victims exceed 3 square centimeters. In the treatment of this category of patients, the use of 3D modeling becomes especially relevant. Polyetheretherketone (PEEK) is a polyaromatic semi-crystalline thermoplastic polymer with mechanical properties favorable for biomedical applications. PEEK-based materials are becoming an important group of biomaterials used for bone and cartilage replacement, as well as in a large number of diverse fields of medicine. The possibility of using these materials in the 3D printing process increases scientific interest in them. The PEEK matrix is a 3D printed custom mesh that serves as a container for the plastic material. It is important to note that the chemical inertness of the PEEK surface does not guarantee good interfacial biocompatibility and requires surface modification before its use in vivo. The use of PEEK to replace bone defects, particularly after gunshot wounds to the extremities, requires further scientific research and clinical observations.
The analysis of clinical cases presented in the article aims to expand the understanding of orthopedic trauma surgeons about the possibilities of using 3D print PEEK matrix technology and help in making tactical clinical decisions in complex cases where there are significant bone defects.
Keywords: bone defect, spiral computed tomographic scanning (SCT), 3D print modeling, PEEK matrix, BMAC, humerus.
Regarding complex clinical cases, when there is a need to replace large bone defects after injuries, gunshot wounds, oncopathology and other pathological conditions, individual preoperative planning using additive technologies - 3D modeling and 3D printing - is becoming widespread throughout the world. These technologies are useful both for the manufacture of individual navigational aids and tools, and for the creation of individual metal and non-metal structures for replacing bone defects, creating a base or matrix for further formation of lost bone tissue.
Taking into account the fact that with gunshot wounds to the limbs, primary bone defects are diagnosed in 7.1% of wounded servicemen, which in 79.3% of victims exceed 3 cm [2], the use of additive technologies is gaining special relevance in this category of patients.
According to the data of modern literature, the vast majority of gunshot fractures of long bones have a multifragmentary or fragmented nature (76.4%), which determines the difficulty of staged reconstructive operations and requires long-term staged treatment and rehabilitation. [3].
An increase in the severity of soft tissue and bone injuries caused by the constant improvement of weapons, imperfection or lack of personal protective equipment, purposeful work of snipers, which is specifically aimed at disabling the wounded (46.3%) [1].
Gunshot wounds of the limbs, which are accompanied by the formation of both primary and secondary defects, are always primarily contaminated, are often combined with soft tissue defects, require multi-stage treatment using various bone-plastic surgical interventions, long-term multidisciplinary rehabilitation treatment, which causes a significant economic burden on the state.
Replacement of bone defects can be temporary with the help of hand made or manufactured spacer systems or permanent with the use of autobone, cortico-cancellous and structural allobone, calcium sulfate matrices (Stimulan), bioceramics, individual PEEK (polyether ether ketone) augments, titanium augments and grids for auto- and alloplastic materials based on the use of 3D printing in combination with orthobiological technologies (PRF - platelet-reach fibrin, BMAC - bone marrow aspirate concentrate, Lipogems, etc.).
Polyether ether ketone (PEEK - polyether ether ketone) is a polyaromatic semi-crystalline thermoplastic polymer with mechanical properties favorable for biomedical applications. Polyetheretherketone forms: PEEK-LT1, PEEK-LT2 and PEEK-LT3 have already found use in various surgical fields: spine surgery, orthopedic surgery, maxillofacial surgery, etc. [7]. The synthesis of new PEEK composites significantly expands the physicochemical and mechanical properties of PEEK materials. Various types of PEEK surface functionalization and PEEK structural modification have been proposed to improve their osteoinductive and antimicrobial abilities. PEEK-based materials are becoming an important group of biomaterials used for bone and cartilage replacement, as well as in a large number of diverse fields of medicine. The possibility of using these materials in the 3D printing process can increase scientific interest and their future development [8]. PEEK matrix is a 3D-printed individual grid that corresponds to the anatomical area of the destroyed bone and serves as a container for plastic material.
According to scientific works, the chemical inertness of the PEEK surface does not guarantee good interfacial biocompatibility and requires surface modification before its use in vivo. In order to improve biocompatibility, such chemically inert materials as PEEK can be specially modified using plasma technology methods [4]. In particular, the use of SPEEK (PEEK, which is sulfonated) compatible with orthobiological technologies, in particular exosomes derived from BMAC, improves biocompatibility and osteoimmunomodulatory effect to promote osteogenesis [5].
Thus, the use of this material to replace bone defects, in particular after gunshot and other limb injuries, requires further scientific research and clinical observations.
Goal of the work. The analysis of clinical cases presented in the article aims to expand the understanding of orthopedic trauma surgeons about the possibilities of using 3D print PEEK matrix technology and help in making tactical clinical decisions in complex cases where there are significant bone defects.
The materials of the work are presented by two clinical cases of surgical treatment of humerus defects using PEEK matrix. Case 1: a patient after a gunshot wound with a multifragmentary fracture of the humerus along the middle and upper third of the diaphysis with the formation of a bone tissue defect. Case 2: a patient with a secondary humerus defect along the entire diaphysis after a series of unsuccessful ORIFs (open reduction internal fixation) using LCP (Locking Compression Plate).
Computed tomography (CT) of the damaged and healthy contralateral shoulder was performed to obtain and further process the data. CT scan was performed on a TOSHIBA Activion 16 spiral computer tomograph with a tube voltage of 120 kV, a current of 150 mA, a spiral pitch of 0.5 mm, tube rotation in 0.75 sec., a hard reconstruction core FC03 or FC 30 (Kernel) , with a field of view of about 180 mm. The analysis of the produced materials was carried out on the Vitrea 6.1 workstation.
After performing a CT scan in telemedicine mode (free google-, free zoom-conference), pre-operative planning was carried out using the SOFTWARE MATERIALIZE MIMICS INNOVATION SUITE software in cooperation with "Materialize Ukraine" specialists. The main stages of the surgical intervention, the size and shape of the future PEEK matrix, the fixation method, as well as the volume of the future plastic material depending on the means of metallo-osteosynthesis (the shape of the plate, the diameter of the intramedullary rod, etc.) were discussed. After agreement on the main issues, 3D printing of individual PEEK matrix was carried out. PEEK matrix is a bioplastic grid printed using 3D printing taking into account the CT data of the damaged and healthy contralateral segment. In the future, operative interventions were carried out using autocyst alone and in combination with cortico-spongy autocyst and PEEK.
Wounded man, 38 years old. He was wounded during military operations on the territory of Ukraine. He was admitted for treatment with a diagnosis: blind gunshot wound (April 25, 2022) of the upper third of the right shoulder with a gunshot fracture along the upper and middle third of the right humerus with displacement of fragments, the formation of a bone defect along 6 cm of the diaphysis of the right humerus and the presence of extraneous bodies (metal fragments) in the fracture projection (photo 1). Primary surgical treatment of the gunshot wound, external fixation of the fragments of the right humerus with a rod apparatus of external fixation was performed as a priority (photo 2).
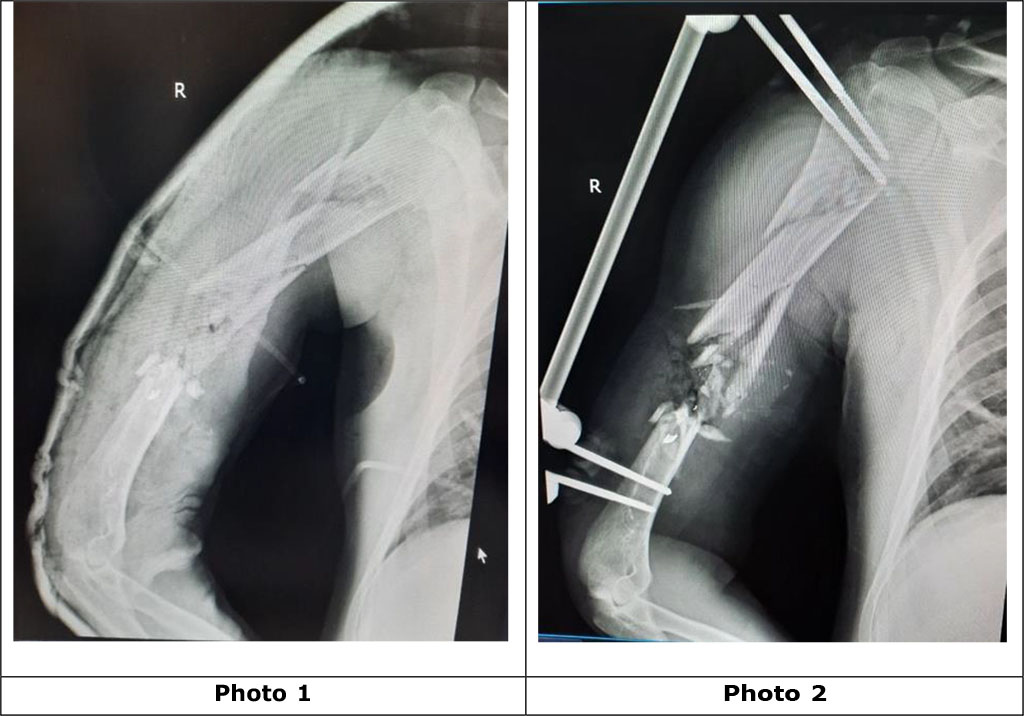
Photo
1. Radiographs of the right shoulder with a gunshot multifragmentary
fracture along the middle and upper third of the diaphysis of the
humerus with displacement of the fragments, a defect in the bone
structure, and foreign bodies (metal fragments) before the operation
Photo
2. Photo-radiogram after the operation of the primary surgical
treatment of the gunshot wound, external fixation of the fragments of
the right humerus with a rod apparatus of external fixation.
Considering the defect of the humerus, after wound healing and removal of the external fixation rod device, a decision was made to carry out surgical intervention in the scope: replacement of the defect with an individual 3D Print PEEK matrix with fixation of the fragments of the humerus with a blocked intramedullary rod.
Conversion, that is, the transition of one method of surgical treatment, in particular the fixation of fragments of the humerus with a rod apparatus of external fixation, to another, namely, internal metallo-osteosynthesis using a blocked rod, was carried out after healing of the wounds from the rods, after dismantling the rod apparatus of external fixation, reduction of local edema, normalization of the patient's body temperature , blood laboratory indicators, in particular: the level of leukocytes is less than 8x109, the level of C-reactive protein is less than 10 mg/l, the level of ESR is less than 15 mm/h, the normalization of total protein is not lower than 66 g/l and the albumin-globulin ratio is up to 2, level blood procalcitonin to 0.046 ng/ml.
Pre-operative planning was carried out in cooperation with "Materialize Ukraine" specialists using the SOFTWARE MATERIALIZE MIMICS INNOVATION SUITE.
With the help of the software, a virtual reposition of bone fragments was performed after a gunshot fracture of the humerus (photos 3 and 4).
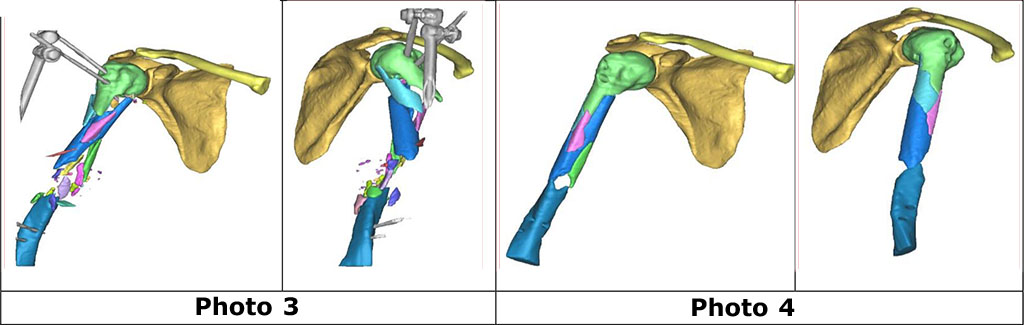
Photos 3 and 4. Digital model of the right shoulder before (3) and after (4) virtual repositioning of bone fragments of the right humerus.
According to the diameter and shape of the proximal and distal fragments of the humerus, a grid of a cylindrical shape - PEEK Matrix - was designed, which will serve as a container for plastic material and perform an additional stabilizing function of the fragments (photo 5).
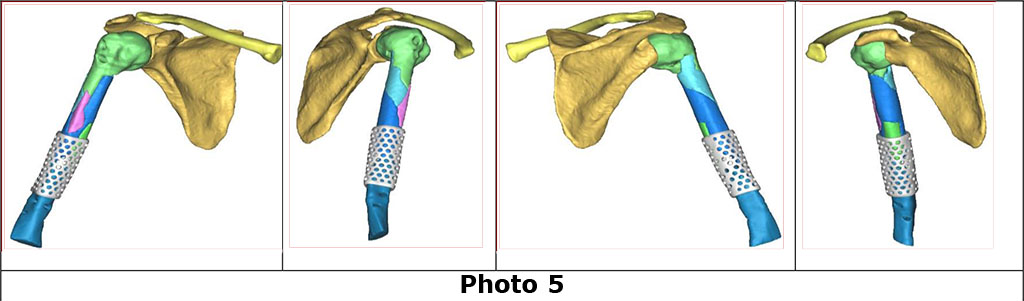
Photo 5. Virtual image of a PEEK grid following 3D modeling using SOFTWARE MATERIALIZE MIMICS INNOVATION SUITE as a stage of preoperative planning.Using the software, the diameter of the humeral canal was determined to select the appropriate size of the intramedullary rod, which was 10.1 mm (photo 6).
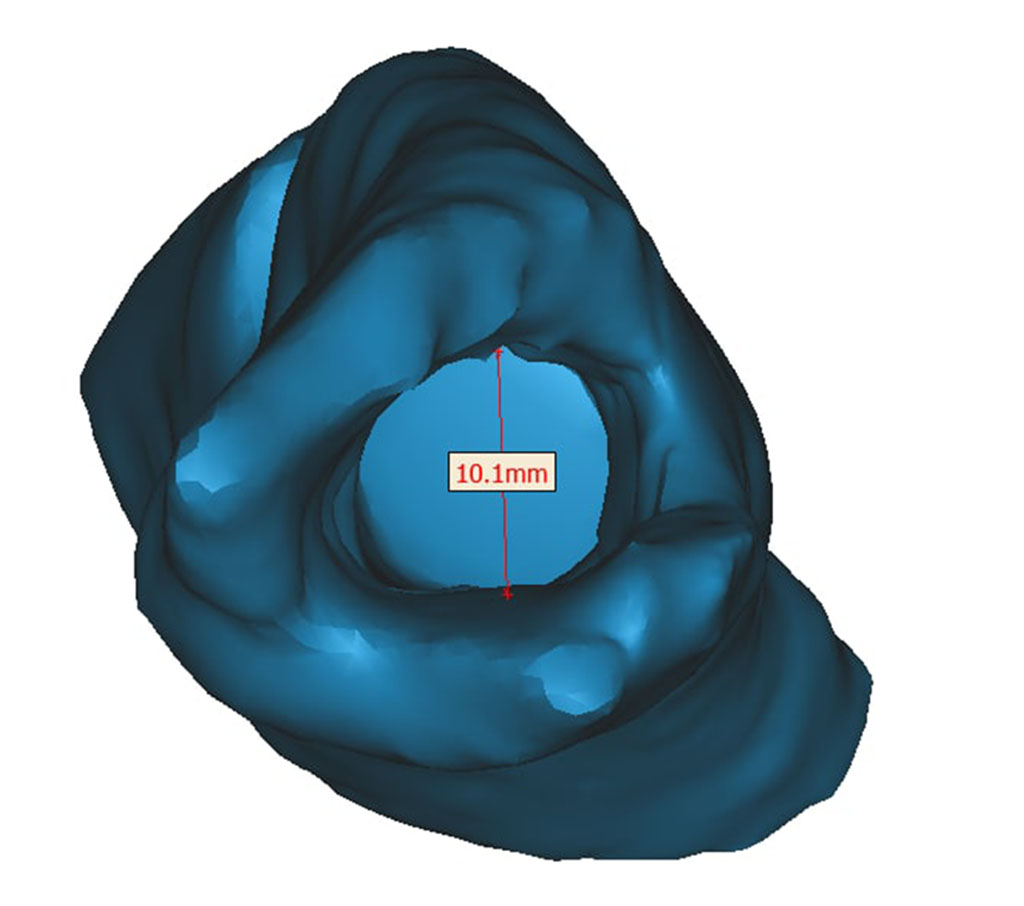
Photo 6. Virtual axial section of the medullary canal of the humerus using the MATERIALIZE MIMICS INNOVATION SUITE SOFTWARE.
After detailed preoperative planning, taking into account 3D planning data, 3D printing of PEEK Matrix and surgical intervention was performed in the scope of: lateral access with opening of the fracture zone of the right humerus, removal of foreign bodies (metal fragments) and small non-viable bone fragments. Recanalization of the proximal and distal bone fragments of the right humerus was performed. PEEK Matrix is filled with small fragments of autobone. After that, PEEK Matrix was adapted to the proximal and distal fragments of the humerus with fixation of the main fragments with a blocked intramedullary rod (photos 7, 8, 9).
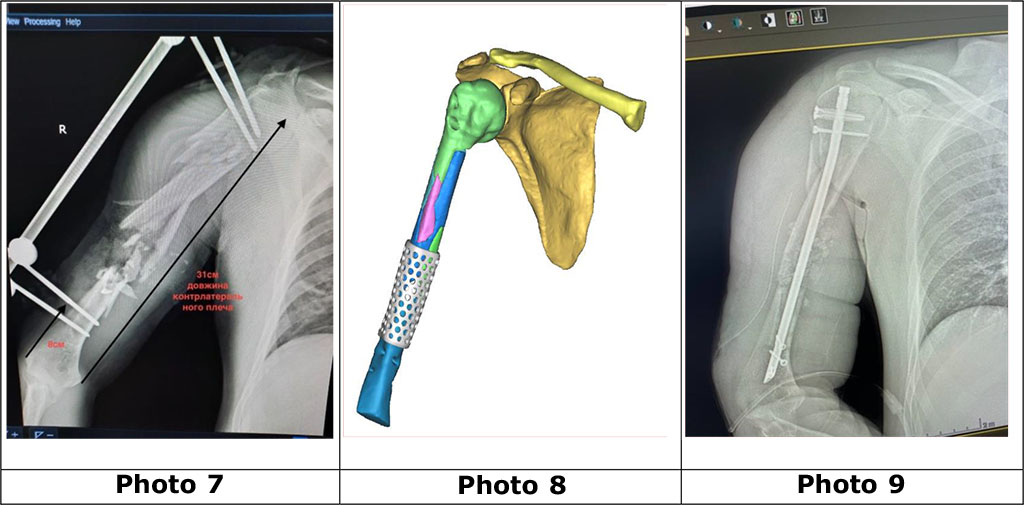
Photo
7. X-ray of the right shoulder with a multifragmentary fracture and a
defect of the humerus in the middle third of the diaphysis, which is
fixed with a rod device of external fixation.
Photo
8. Photo of a digital model of the right humerus with bone fragment
adaptation and 3D PEEK Matrix mounting on the humerus defect site.
Photo
9. Photo of the radiograph of the right shoulder: the defect of the
humerus is filled with auto bone, the fragments are fixed with a
blocked intramedullary rod. PEEK Matrix is X-ray transparent and
therefore not detectable.
In the postoperative period, immobilization of the right upper limb was carried out using an orthosis, as well as physical therapy to restore movements in the joints of the limb and restore muscle function according to the protocol after BIOS of the humerus. On the 10th day, seroma formation took place. Repeated surgical treatments using VAC therapy were performed. The wound healed in 21 days.
Patient S., a 51-year-old man, sought treatment for non-union after a fracture in the middle third of the humerus after a series of unsuccessful surgical interventions (MOS plate of the right humerus) with the development of significant deformation, sclerosis and osteolytic defects along the proximal and distal fragments of the right humerus bones (photos 10, 11, 12).
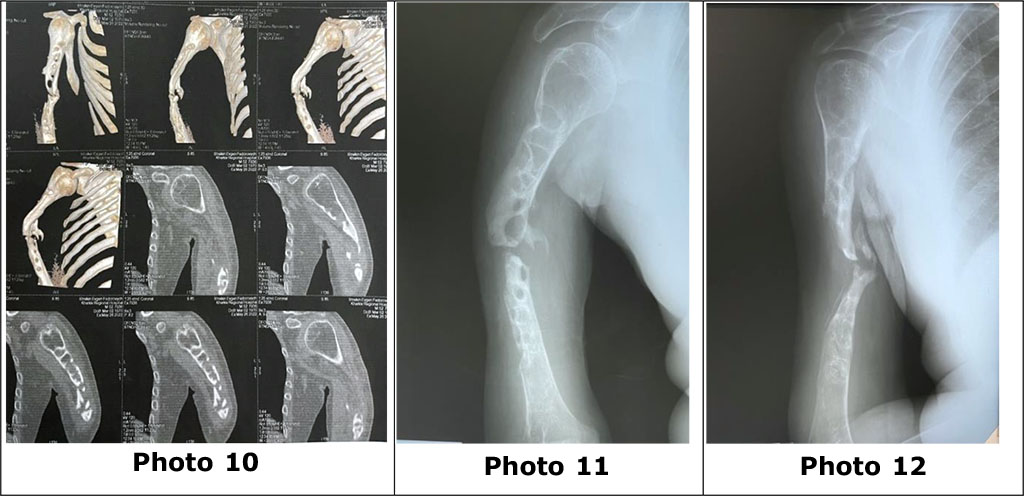
Photo 10 - computer tomography, photos 11, 12 - radiographs of the right humerus with signs of the formation of a false joint in the middle third of the humerus, pronounced sclerosis and pathological osteolytic cavities of the proximal and distal parts of the right humerus.
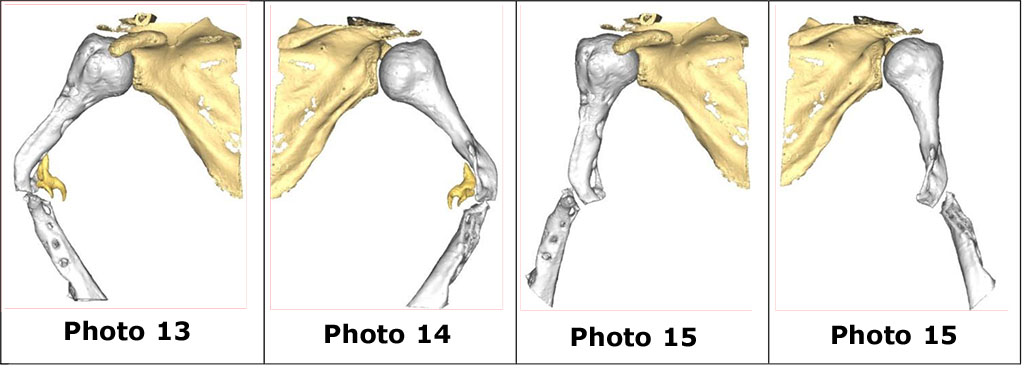
A clinical examination reveals a postoperative scar on the lateral surface of the right shoulder, compacted, hardened, without signs of inflammation. As in the first case, pre-operative planning was carried out in a Zoom conference in cooperation with the specialists of "Materialize Ukraine" using the SOFTWARE MATERIALIZE MIMICS INNOVATION SUITE. With the help of the software, a virtual image of the pathological segment (photos 13, 14) and digital repositioning of bone fragments of the humerus (photos 15 and 16) were performed.
Based on CT analysis and a 3D model of the pathologically changed right humerus, the level of resection of the proximal and distal main fragments of the humerus, their length from the level of resection to the end of the fragment, and the length, shape and diameter of the PEEK grid were determined (photos 17, 18, 19 ). For the stability of the grid, its length was calculated with an overlap of 2.5 cm on the proximal and distal fragments of the humerus. Thus, the length of the lattice was 169.6 mm.
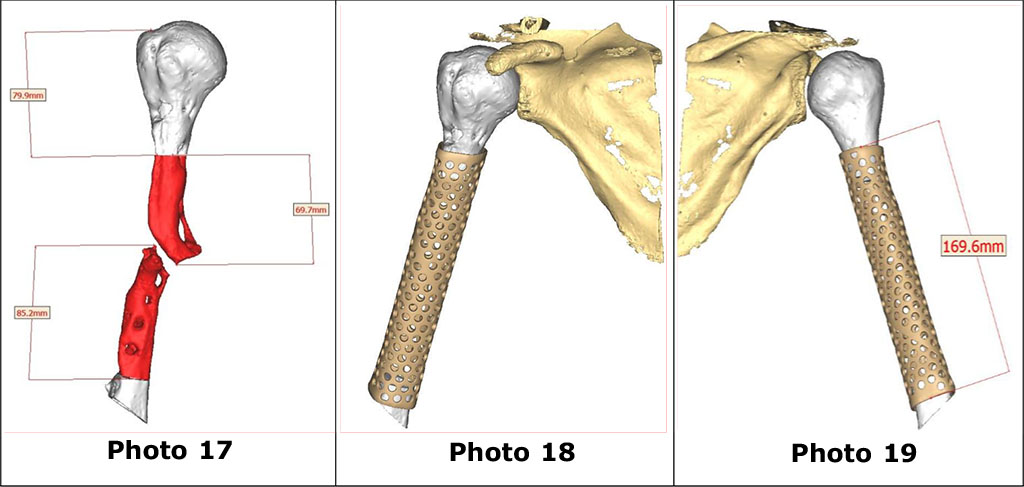
In addition, the diameter of the recommended blocked rod and the volume of auto- and alloplastic material to fill the grid were determined. The length of the blocked rod, which was calculated, was 240 mm.
According to the calculation, the minimum volume to fill the space between the cage and the rod of different diameters is:
Additionally, depending on the situation, but not depending on the diameter of the rod:
That is, the calculated maximum plastic material for the PEEK lattice with the most dense filling and a rod with a diameter of 8 mm, which was 84.3 cm3. The total volume of the cut bone fragments that can be used as autoplastic material was 34 cm3. It was planned to use 24 cm3 of cortico-spongy granulate "OMS-A-KGG" and 26.3 cm3 of cortico-spongy automaterial from the wing of the left iliac bone.
Surgical access and operation. Taking into account the need to open the humerus throughout, an anterolateral approach was chosen, starting along the deltoid-thoracic groove and continuing down along the lateral groove of the shoulder with a transition distally to the anterolateral surface of the shoulder for revision of the radial nerve. Mobilization and neurolysis of the right radial nerve, removal of interfragmentary scar tissue were carried out first. The proximal and distal bone fragments of the humerus are arthroscopically altered with numerous zones of osteolysis (photos 20, 21).
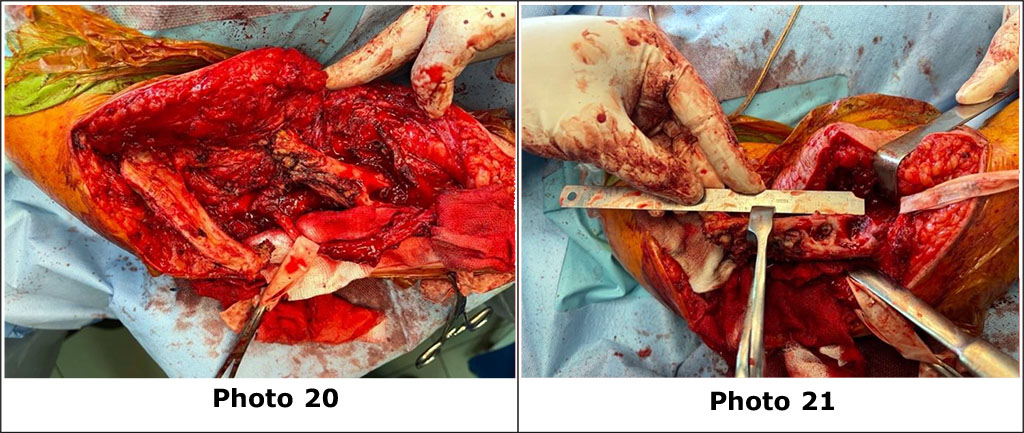
Photo
20. Bone fragments of the right humerus mobilized from scar tissue.
Neurolysis of the right radial nerve was also performed.
Photo
21. Pronounced osteolysis of the fragments of the right humerus, the
level of resection of the proximal fragment of the humerus is
measured.
Bone fragments were isolated from the scar tissue and resected with an oscillating saw. At the same time, cortico-spongy automaterial was collected from the wing of the left iliac bone. The plastic material for filling the PEEK matrix is represented by three sources: 1- cortico-spongy automaterial from the wing of the left iliac bone with a volume of about 30 cm3; 2 - cortico-spongy material from the proximal and distal fragments of the humerus after resection; 3- cortico-spongy granulate "OMS-A-KGG" - 2 packages of 8 grams, 12 cm3 each, i.e. 24 cm3 in total. (photo 23).

Photo
22. General view of the combined auto-alloplastic material and PEEK
lattice.
Photo
23, 24. The combined auto-alloplastic material is placed in the grid
and filled with BMAC from the wing of the iliac bone.
To biostimulate regenerative processes, BMAC from the wing of the iliac bone was added to the combined auto-alloplastic material.
After filling the PEEK grid with a combined auto- and alloplastic material (photos 23, 24), the latter was mounted and adapted to the proximal and distal ends of the humerus. A reamer up to 8 mm was reamed along the guide wire and the fragments were fixed with a blocked intramedullary rod 240 mm long and 8 mm in diameter with 4 blocked screws. The lattice is additionally blocked in the distal part with a cortical screw (photos 25, 26, 27).
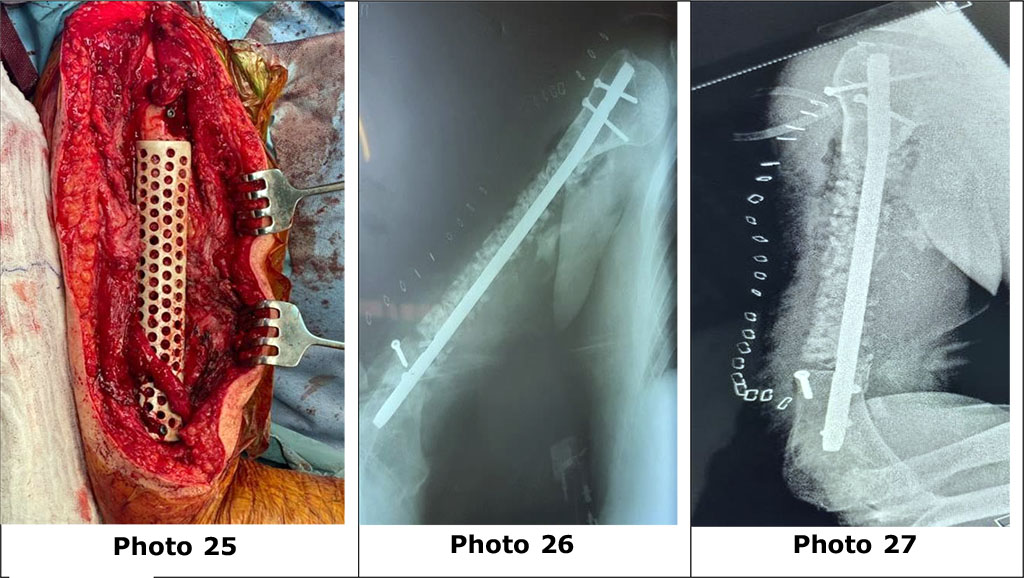
Photo
25. General appearance of the surgical wound after BIOS and the use
of a PEEK grid.
Photos
26, 27. X-rays of the right shoulder after surgery.
After the operation, the wound is drained with active PCV drainage. Immobilization of the right upper extremity using an orthosis with abduction up to 15 degrees. In the postoperative period, neuropathy of the right radial nerve was not observed (photo 28).
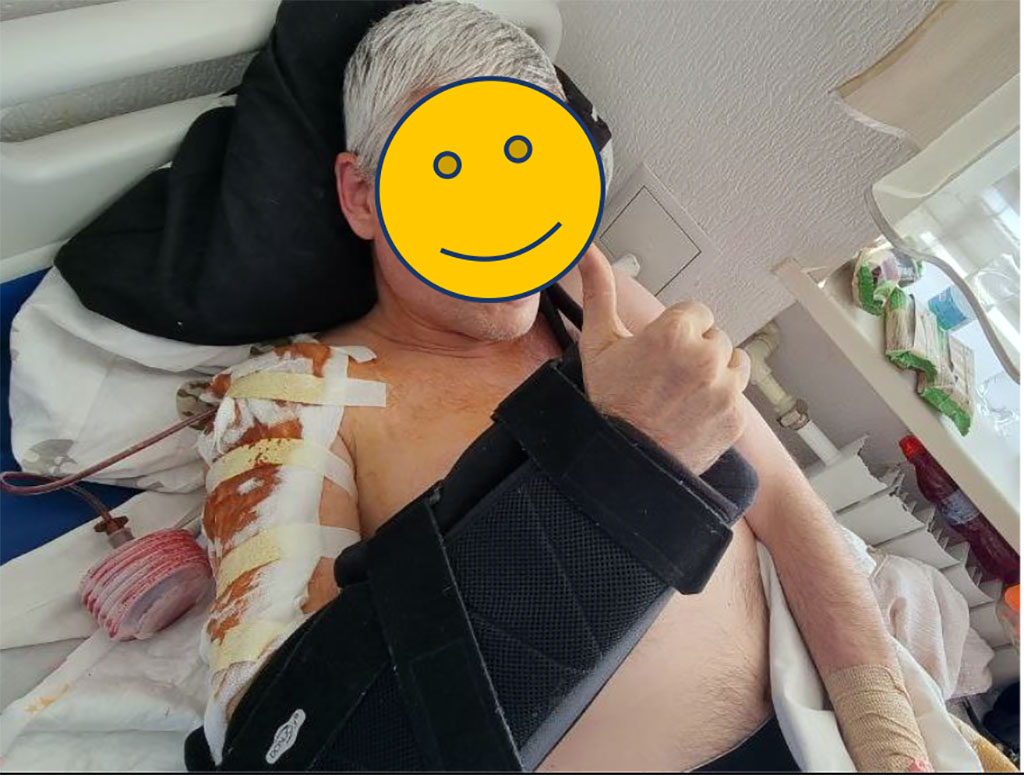
Photo 28. General view of the patient and his right hand, indicating the absence of neuropathy of the right radial nerve.
The patient received antibacterial, anti-inflammatory therapy, as well as Pascorbin 7.5 g per 200 ml of physiological solution intravenously by drip 2 times a day for 10 days. After 12 days, the postoperative period was complicated by the development of seroma in the surgical site. Opening and toileting of the wound, washing with a decamethoxine solution with the installation of an inflow-washing VAC was carried out. Replacement of VAC was carried out after 7 days with reduction of the wound and VAC twice (photos 29, 30). In parallel, the development of movements in the shoulder and elbow joints of the right upper limb was carried out in accordance with the rehabilitation protocol after BIOS of the humerus.
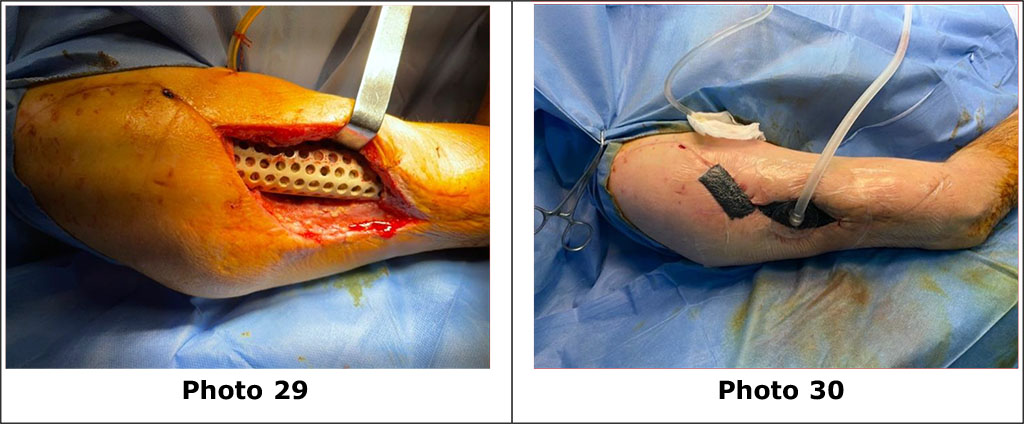
Photos 29, 30 view of the wound after the opening of the seroma of the surgical site, toileting of the wound with dekasan with the installation of inflow VAC to remove remnants of seroma and stimulation of reparative processes in the area of the PEEK grid.
A large proportion of gunshot wounds to the limbs, which are accompanied by the formation of primary bone defects, necessitates the search for new methods of replacing bone defects. This is especially relevant in cases where there is a significant volume of the defect and its anatomical features.
Replacement of bone defects with the use of PEEK mesh is a new direction in the treatment of gunshot wounds of the extremities. Due to the use of an individual implant, which is characterized by almost 100% similarity with the native bone, it is possible to reproduce the anatomy of the damaged bone fragment as accurately as possible.
Although PEEK is chemically stable, biocompatible, radiolucent, and has an elastic modulus similar to that of natural bone, it is characterized by poor integration with the surrounding bone tissue after implantation. In order to improve the bioactivity of PEEK, numerous strategies are proposed to increase the functionality of the PEEK surface and change the PEEK structure, which will increase the biocompatibility of PEEK implants and determine the direction of manufacturing multifunctional implants in the future [6].
Important criteria for the success of surgical intervention in gunshot wounds of the extremities with the formation of bone defects are compliance with the rules of conversion, namely: the absence of local inflammation and complete wound healing after dismantling the AZF rods, normalization of the patient’s body temperature and blood laboratory parameters, in particular: the level of leukocytes, SRP, ESR , total protein, albumin-globulin ratio and blood procalcitonin level. In every case of surgery for gunshot bone defects, tissue biopsies are recommended to rule out infection. Cultures taken during revision surgery are often positive, even when patients are thought to be uninfected.
When using individual PEEK grids in patients with bone defects, in our observations, the formation of aseptic seromas and hematomas is noted in the early postoperative period. In our opinion, this is a sign of a violation of the adaptation of this material, which indicates the expediency of using orthobiological technologies in the postoperative period, in particular PRFM and BMAC, as well as the search for special coatings or spraying on PEEK grids.
Since this method of treating bone defects is relatively new, it is necessary to further accumulate the experience of its solidification with the analysis of the possibilities of improving the integrative properties of the material, errors and complications, and methods of their prevention and treatment.
The authors declared that this study has received no financial support.
The authors have no conflicts of interest to declare.