- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
![]() cojocarumariaeva@yahoo.com, aliaplesea@yahoo.com
cojocarumariaeva@yahoo.com, aliaplesea@yahoo.com
Introduction: Parasomnias are disorders that may appear during sleep with and/or without dreams. To describe them we must take in account a subjective description by the patient and his relatives. Objective measurement of this phenomenology is made with Polysomnography, Electromyography and Holter EKG. Material and Methods: We searched the recent data about parasomnia in the Medline, Pubmed, Google academic databases as also in classic books and reviews. Results: The clinical picture is various from motor and neurological signs to autonomic signs as also sleep related hallucinations. There are more rare presentations with associated disorders due to excretion and involuntary urinary emission during sleep disorders. Parasomnias are often preceded by a traumatic event for the patient and his family members which can be a head trauma or an infection or an intoxication which can be accompanied by psycho vulnerable events. On the other part parasomnias can be themselves a preamble announcing neurodegenerative diseases like Parkinson disease, Lewy Body Dementia or some synucleopathies. Conclusions: The fluctuations of neurotransmitters (Dopamine, Serotonine or Acetylcholine) due to specific neurologic pathology can lead to particular parasomnias, their evolution corresponding to each impairment. The knowledge of accompanying parasomnias of neurologic disorders like those from Parkinson disease helps manage diseases of neurological patients already known with Parkinson's disease or other neurological diseases, leading to increased quality of life for these patients as a result of specialized intervention.
Keywords: parasomnias, neurotransmitters, neurodegenerative diseases, dream
The sleep state is physiological and has the characteristics of reversibility. The person is not conscious in this state and from motor point of view the reactions are reduced (Santamaria & Tolosai, 2016; Sandu et al., 2017). The sleep is composed from sleep cycles with more stages of four types which are NREM sleep called so with nonrapid eye movements, and a stage called REM (rapid eye movement) which are succeeding more times in a night these cycles varying in length and proportions between different tags of sleep, so they are not identical. After recording we obtain a hypnogram. During REM sleep the EEG expresses with low voltage and desynchronization. In this stage peoples are dreaming (Cheyne et al., 1999).
Sleep disorders vary at quantitative level so are insomnias-means few sleeps and hypersomnia’s meaning to much sleep as also in the qualitative way like in parasomnias or mixt where the circadian rhythm is disrupted (Grigoras & Ciubara, 2021). Parasomnias presented in table 1 have a variety of accompanying phenomena consisting of behaviours and emotional experiences before asleep, during the NREM sleep or during the sleep with dreams, the REM sleep (Santamaria & Tolosai, 2016).
Table 1 Types of parasomnias
| Types of parasomnia | Sleep stage | Characteristics | Observațions |
| Isolated sleep paralysis | Asleep Before complete awakening | Conscious but canot moove | Is
included as parasomnia linked to REM sleep. There can coexist
hypnagogic and-or hypnopompic phenomena There can be a hereditary component. A person can have a single episode during life, or they can repeat. |
| Restless leg syndrome | REM sleep disorder | Person
is not conscious Sensorimotor disorder The desire always to move the legs Paraesthesia of the limbs |
In putamen located iron deficiency as also in, thalamus, caudate nucleus and substantia nigra Decrease of D2 receptors in the putamen. |
| Rhythmic
movement disorder during sleep |
Ata awakening | The body baloances with /or without the head and/or without the limbs | |
| Somnilocvia | REM sleep | Repeat
words of complex expressions .complete amensia of episodes |
|
| Bruxismus | Light stages of NREM sleep as stages 1 and 2 | The activity of the masticatory muscles are watched | Destructions of the teeth, Teeth grinding appear in the REM sleep. Teeth are protected with special devices |
| REM sleep behaviour disorder RBD | During REM sleep | Rapid movements in sleep can affect the patients during sleep which can lead to trauma and fractures. At 60-97 years the prevalence is 6-7% | Can
coexist with major depressive disorder announcing a possible
degenerative disorder. Dopamine is lowered in the striatal
neurons. On the other hand, the reticular activates in this
disorder |
| Sleep Enuresis | Different stages of NREM sleep and during REM sleep | Involuntary
urine emission 97-98% din
enurezis e non-organic Dacă ambii părinţi au enuresis 70% că şi copilul va avea |
It is primary or secondary, it is continuous or discontinuous in both forms, more often due to diabetes, urinary infections but not due to sleep apnea |
| Nocturnal paroxistic dystonia | Non-REM sleep | Convulsions like episodes | |
| Somnambulism | REM sleep | Amnesia of the episode | Can steal objects of commit crime. Treatment can consist with substances used also in convulsions anticonvulsants and/or antidepressants |
| Nightmare | Stage 2 of NREM sleep , or REM sleep | The episodes are appearing generally after midnight | Can appear in posttraumatic stress disorder, or when the subject is looking before asleep to horror movies or games |
| Nocturnal pavor | REM sleep | The episodes are finding place before midnight generally Lasting for 15 minutes medium. Cannot communicate | |
| Dissociateive disorder ins leep | NREM and REM sleep | Following or concomitant with migraines | |
| Catatrenia | REM sleep | Groaning occurs during expiration in sleep | Using CPAP machines |
| Hypnagogic at asleep and hypnopmpic at awakening hallucinations | Stage I sleep and at awakening | Can appear also in Intoxications, tumours, physiologic | |
| Exploding head syndrome | Any stage of sleep or between the stages of sleep | Can appear more times in a month, anxiety is great | |
| Eating disorder during sleep | Stage 4 | Ingestions of food and/or drinks during sleep with or without amnesia of the episode | |
| Confuseive awakenings | REM sleep | Awakes harder | Also called sleep drunkenness |
Source: Authors' own conception
There is existing two neuronal subpopulations: sleep-on neurons-these neurons have cholinergic transmission, and a neuronal population sleep-off and their transmission is serotoninergic and noradrenergic which are located at pontine level. A theory explains how the dreams appear (Ciubara, 2019; Rizzo et al., 2012; Sandu et al., 2018). Profound respirations will generate a sensation of suffocation or push of the thorax. These sensations can lead in a next stage to fear but also to visual and auditive hallucinations. The limbic system is the turntable wich modulate the emotions and is activating during REM sleep (Dobrescu & Rad, 2010; Rădulescu et al., 2020). These events were demonstrated with functional studies, and it revealed that in the cingulated cortex which is part of the limbic system take place the changes which can explain the mood alterations when REM sleep disorder coexist with depression (Rahmani et al., 2018). In 1999 R. Melzack proposed a new model of interconnexion of neural networks and this is called by him the neuromatrix. In this model the cerebral hemispheric surface is connected to the limbic system, under genetic influences (Melzack, 2001). Each person has an unique electric signature through the sum of his electrical discharges of the neurons after the individual electrical model (Iapascurta, 2015). On the other hand the distruction of the anatomic pathways involved in the sleep mechnisms can lead to severe alterations of it. So for example the pontine infarct determines the reducing of REM sleep as also the NREM sleep. Other diseases and conditions generating sleep disorders are Arnold Chiari Malformation as also Syringomyelia and/or Syringobulbia (Ropper et al., 2014). After location stroke are producing different effects on the sleep, so at the crebral hemnispheres the stroke produces the inversation of day-night cycle of sleep and in the case of mesencephalic stroke appear peducnular hallucinations. The nervous system suffers an assymetric aging process and the dopaminergic structures from the mezostriatum are the first affected and this phenomen is more pregnant for the mens (Ciobotea et al., 2016; Ciubara et al., 2018, Paduraru et al, 2019; Szasz 2010). Becasue of degenrative processes the therapeutic response for specific agent groups is modified in time and the treatment measures will be adequate for each stage of the disease (Caras & Sandu, 2013; Panea, 2010).
The white matter can be decreased in volume in the Restless leg foot syndrome (Provini & Chiaro, 2015). The dopaminergic pathways at striatal level can be seen with SPECT and PET in the patients with REM sleep behavior disturbances disorder. The white matter was investigated with fractioned ansiotropic diffusion tensed images DTI, axial and also radial difusivity with applied statistics. Another method is the connectometry related to MRI with difusion (Rahmani et al., 2018). Other imagistic approaches are voxel based morphometry, diffuzion based imaging and relaxometry or transcranial sonography (Provini & Chiaro, 2015). In the case of a patient with hypnagogic hallucination 59 years aged, with abulia and anhedonia we foudna infiltrative tumour. She made computer tomography native and contrast. Figure 1 a is the native imagine with digitiform oedema and figure 1 b postcontrast copmputer tomography shows the infiltrative process.
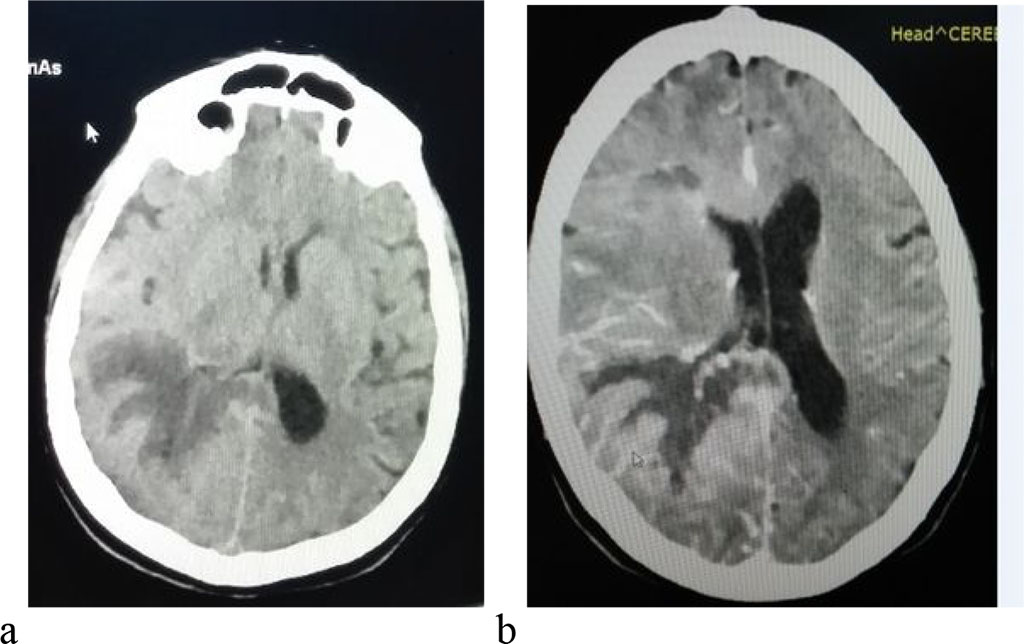
Figure 1 a native computer tomography with digitiform oedema 1b
Computer tomography with intravenous contrst substance
parietooccipital right infiltrativ process
Source: Authors' own
conception
The dimension of the parasomnia spectrum must be perceived in the correlation of an integration process of the neurologic and psychic and psychological functioning, so that the autonomy of the patient is more and more high, so they are self-defeating and perform in everyday life. In figure 4 the dimensions which must be reached by the therapeutic team are the following.
So, in Alzheimer patients 24% of their nights are with involved sleep disorders. The proportion between different stages of the sleep are different in these patients so, the stage 1 NREM is lasting far more, and the REM sleep is disappearing slowly. The processes of the construction of the entire neuronal network depens on gnetic factors but a role is played also by external influences, so a specific diversity is obtained which is unique for the indeividualisation of a single person. Adapting the mental health services to the needs of the patients is made by continous transformation and dinamisation.