- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.27
![]() terpan.mihai@yahoo.com,baciu91@yahoo.com,
terpan.mihai@yahoo.com,baciu91@yahoo.com,
carmengavrilaa@gmail.com
Introduction: Eating disorders are mental illnesses characterised by abnormal eating habits that have a negative impact on a person's physical or mental health. In the last decade hospitalizations which included eating disorders increased among all age groups. The assessment of eating disorders associated with affective disorders has important clinical implications, but the standard psychiatric classification DSM-5 (American Psychiatry Association, 2013) and ICD-10 (World Health Organization, 1993) are limited.
Objectives: The current study aims to broaden the evaluation of this association and better understand its clinical implications. In addition, the study's goal is to comprehend the implications of eating disorders in Galaţi County.
Method: We conducted a retrospective study on 147 patients with eating disorders and mood [affective] disorders who were admitted to the Psychiatry Hospital "Elisabeta Doamna" Galati between January 1 and February 1, 2019.We used ICD-10 (Classification of Mental and Behavioral Disorders) and DSM-5 criteria for diagnosis (Diagnostic and Statistical Manual of Mental Disorders).
Results: In the period from 1 January 2019 - 1 February 2019 a total of 1131 patients was admitted in the Psychiatry Hospital, Of these, 147 were diagnosed with mood (affective) disorders, of whom 17 patients (12%) associated disorder and food as well as the independent disorder. Among these patients, the percentage of women with eating disorders associated with the affective disorder was 82 % and the percentage of men was 18 %.
Conclusions: According to the findings, women are more likely to associate eating disorders with mood [affective] disorders. We also found a poor relationship between eating disorders and affective disorders, with eating disorders being associated with a high percentage of other psychiatric disorders, which is represented by alcohol and substance use, but also by high-impact diseases like Alzheimer's disease and schizophrenia.
Keywords: eating disorders, affective disorder, hospitalizations, clinical implications.
Eating disorders are mental illnesses characterised by abnormal eating habits that have a negative impact on a person's physical or mental health (American Psychiatry Association, 2013, pp. 329-354). In the last decade hospitalizations which included eating disorders increased among all age groups. Eating disorders are potentially fatal illnesses that can cause significant disruptions in a person's eating behaviour. “Common eating disorders include binge eating disorder, bulimia nervosa, and anorexia nervosa, which is less common but very serious” (National Institutes of Mental Health, 2018). The DSM-V includes „diagnostic criteria for pica, rumination disorder, avoidant/restrictive food intake disorder, anorexia nervosa, bulimia nervosa, and binge-eating disorder” (American Psychiatry Association, 2013).
The current ICD-10 classification of eating disorders fails to classify the majority of „clinical presentations and ignores continuities between child, adolescent, and adult manifestations; this necessitates frequent changes in diagnosis to accommodate the natural course of these disorders” (Uher & Rutter, 2012).
Despite extensive research into the potential „risk factors associated with eating disorders, researchers have yet to discover the exact etiology of eating disorders, and they have also failed to comprehend the interaction between various possible causes of eating disorders” (Rikani et al., 2013).
The main disturbance in mood[affective] disorders is represented by a „change in mood or affect, usually to depression (with or without associated anxiety) or to elation” (Bolos et al., 2012; World Health Organization,1993).
Mood disorders include: Maniac „episode, bipolar affective disorder, depressive episode, recurrent depressive disorder, persistent mood [affective] disorders, other mood [affective] disorders, unspecified mood [affective] disorder” (World Health Organization,1993).
For eating disorders, medication is used in combination with nutritional and psychotherapeutic treatments.Antidepressants are frequently used to treat „bulimia nervosa, and binge eating disorder can be treated” with antidepressants, or appetite suppressants. Although for anorexia nervosa pharmacological studies have not foud any medication that have definitive improvement of the main symptoms (Ebert, 2009).
Psychotherapy and medication are often combined in the curent practice. Specific treatments are now available for both manic and depressive episodes (Winokur et al., 1980).
A number of studies have found an increase in „affective disorders in the families of patients with anorexia nervosa and bulimia nervosa” (Gershon et al., 1984; Hudson et al., 1983).
Serotonin dysregulation, a powerful „neurohormone involved in both mood and appetite, may be an etiological link, along with potential disturbances in other neurotransmitter systems” (Hudson et al., 1983).
Anorexia nervosa primarily affects young women, whereas bulimia nervosa also „affects women, though the age of onset is later in adolescence” (Valcea et al., 2016).
Males account for 10 to 15% of all cases, and it appears that they are more frequently affected by bulimia nervosa than anorexia nervosa.
Comorbid psychiatric symptomatology is common in patients with eating disorders, with affective symptoms being the most common (Baroiu et al., 2021).
The importance of depressive symptoms appearing in the majority of patients with eating disorders was evident in the earlier conceptualization of these disorders as affective subtypes (Ciubara et al., 2016; Untu et al., 2015).
Currently, depressive symptoms are frequently viewed as secondary to the eating disorder, and they often become less severe or disappear with treatment and resolution of the bulimic behaviour.
A non-randomized observational retrospective study was conducted in the "Elisabeta Doamna"Psychiatric Hospital with a database of 1131 patients out of which 147 patients with eating disorders and mood [affective] disorders, admitted in the Psychiatry Hospital "Elisabeta Doamna"Galati during the period from 1 January 2019 - 1 February 2019. For diagnosis, we used criteria from ICD-10( Classification of Mental and Behavioural Disorders), DSM-5(Diagnostic and Statistical Manual of Mental Disorders). The data was compiled and analyzed using JASP, EXCEL and PSPP.
In the period from 1 January 2019 - 1 February 2019 a total of 1131 patients was admitted to the Psychiatry Hospital. 147 of whom were diagnosed with mood disorders (F30, F31, F32, F33, F34, F38), of these, 17 patients (12%) associated disorder and food as well as the independent disorder (F50).
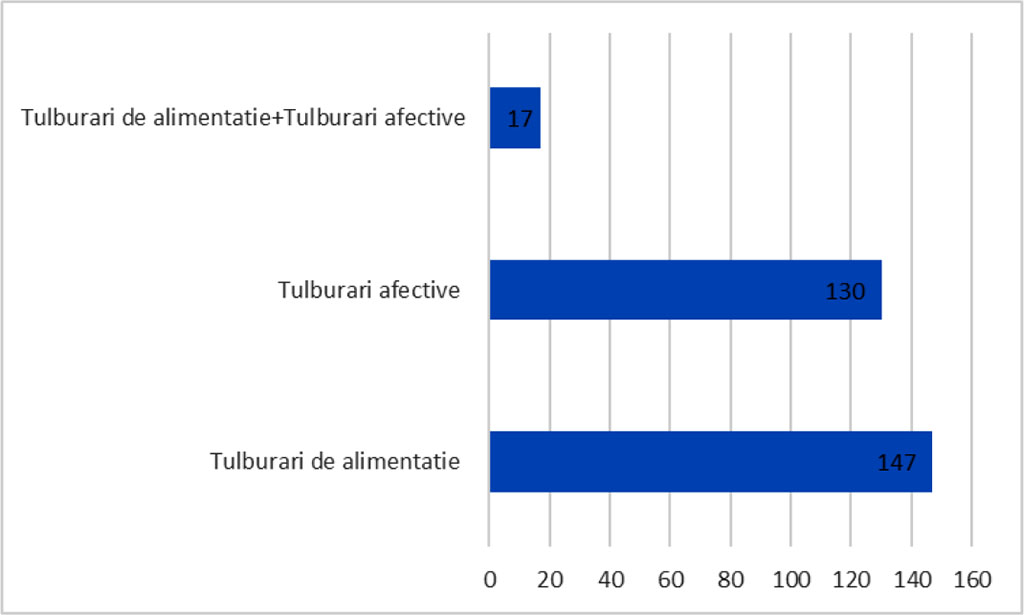
Fig. I – This figure shows us the number of patients
presenting eating disorders associated with affective disorders as
well as the total number of patients and those with only affective
disorders associated with other diagnoses.
Source: Authors' own conception
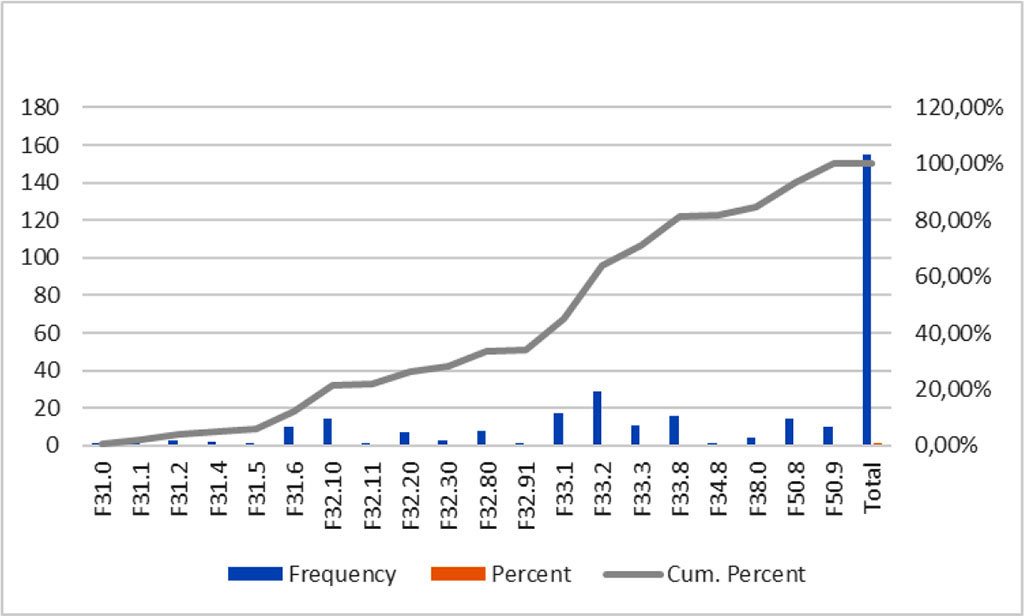
Fig. II - This figure shows us the frequency of the main
diagnostics
Source: Authors' own conception
Among these patients, the percentage of women with eating disorders associated with the affective disorder was 82 % and the percentage of men was 18 %.
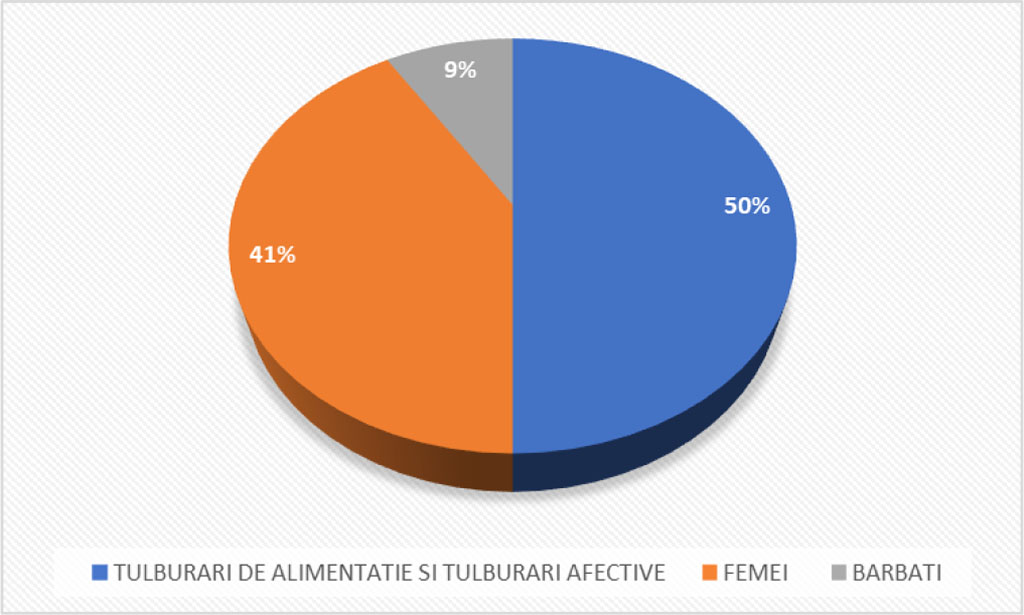
Fig III - This figure shows us the percentage of women and
men that associate eating disorders with affective disorders.
Source: Authors' own conception
Out of all the discharges over a period of one month 59% of patients had been diagnosed with mood [affective] disorders, 8% had been diagnosed with eating disorders associated with mood [affective] disorders and and 34% with eating disorders associated with diagnoses such as schizophrenia or mental and behavioural disorders caused by alcohol use.
The study period is relatively small, so the findings should be evaluated in a longer study for a better understanding of the association between eating disorders and mood[affective]disorders.
Clearly, more studies are needed to clarify the association link between eating disorders and mood [affective] disorders. By exploring this link, we could better understand the implication of this association and provide for our patients with better care and prevent the advanced stages of these diseases and socio-economic implications.
What is more, we could, through both pharmacologic and nonpharmacologic means start prevention strategy for these diseases.
From the results obtained, it can be concluded that women associate more often eating disorders with mood [affective] disorders. We also observed the poor association between eating disorders and affective disorders, eating disorders being associated with a high percentage of other psychiatric disorders, this high percentage is represented by alcohol and substance use, but also by high-impact diseases such as Alzheimer's disease and schizophrenia.
The authors report no conflict of interest in the development of this research.