- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.25
Introduction: Psychiatric disorders occurring during endocrine dysfunction and, conversely, endocrine dysfunctions associated with mental disorders were the emergence of a new discipline, psychoendocrinology. Psychiatric disorders correlated with endocrine diseases are defined as psychopathological manifestations of variable intensity and clinical symptomatology, determined by complex psycho-neuro-endocrinological interrelationships. Defining elements consist of the association between diagnosis of mental disorders and specific symptoms for endocrine dysfunction.
Methods: We conducted a prospective one-year study (January 2018 - December 2018 on 112 patients hospitalized in the Clinic of Psychiatry who also had an endocrinological comorbidity. We investigated the frequency and severity of psychoendocrinological associations by studying a number of demographic and clinical items.
Results: The results showed that the highest incidence belongs to thyroid disorder - 55.36%, followed by gonadal disorders - 24.11%, and, rarely, pituitary diseases and diabetes. Hyperthyroidism was associated most frequently with manic episodes, while unipolar depression prevailed in patients with hypothyroidism. In gonadal disorders, present in majority in female patients (secondary amenorrhea, menopause or erectile dysfunction in males), depression accompanied by anxiety, often severe in intensity, was the most frequent psychiatric diagnosis. Psychotic disorders were met in a smaller number of cases, especially in patients with long history of endocrine disorders and instability of biological constants.
Conclusions: We may state that affective disorders are the most frequent nosologically category in patients with endocrine dysfunctions. It requires a better collaboration between specialists in endocrinology and psychiatry, to highlight the determinants which contribute to the development of psychopathological manifestations in endocrine diseases and to individualize the treatment depending on cases’ particularities.
Keywords: endocrinology, psychiatry, association.
Patients with endocrine disorders are more likely to develop psychiatric symptoms of variable intensity and clinical aspect, especially affective symptoms (Fornaro et al., 2010; Hatzinger, 2000). For instance, major depression was frequently found in patients with Cushing Syndrome, Addison Disease, hyperprolactinemia, amenorrhea, hyper- or hypothyroidism, or any other thyroid disease (Lupu, et al., 2016; Marsh, 1997; Păduraru et al., 2019;). Uncontrolled diabetes, pheochromocytoma and hypoadrenalism are endocrine and metabolic dysfunctions frequently associated with anxious disorders, whereas ovarian diseases are often accompanied by mixed anxious and depressive symptoms (Benson et al., 2009; Chicos et al., 2019; Jefferson, 1988).
It is sometimes difficult to establish a classification of psychiatric disorders based on the degree of organic etiology present in patients with comorbidities, as mental disorders in patients with medical conditions are frequently found in practice (Ciubara et al., 2018, Rădulescu et al., 2020). Patients with endocrine dysfunctions experience psychiatric symptoms very often. This fact can be explained by a series of factors, such as: direct physio pathological effects of endocrinopathy, stress experienced by people with chronic diseases, side effects after a treatment or just a simple coincidence. Over the years, medical literature has presented few studies discussing the temporal relationship between the onset of endocrinopathy and the development of mental disorders (Ciubara et al., 2016; Sonino et al., 2004; Sandu & Damian, 2018; Sandu et al., 2019). In psychiatry, research focused exclusively on medical situations which challenge the physician by the way they develop, either by the complexity of these clinical processes, sometimes with high vital risk, or by their symptoms.
Risk factors for pathological diseases determining mental disorders are represented by hypo- or hyperfunction of the endocrine gland. This highly recommends the study of mental disorder issues that may arise, eventually at a normal pace during the onset, but if they aggravate, they may lead to severe impairments (Sandu et al., 2017; Valcea et al., 2016).
The endocrine system plays an important role in the ontogenetic development of our central nervous system. Thyroid and sexual hormones are also mandatory items which contribute to brain development and maturation. Hormones are essential for brain development, causing general or local changes in psychiatric functions, influencing the level of neurotransmitters and that of the cortical anatomic structures (Ciobotea et al., 2016). From an anatomopathological angle, the most severe endocrine dysfunctions trigger brain damage, such as general or local cortical atrophy in various endocrine diseases (Ciubară et al., 2015). On the other hand, endocrine dysfunctions sometimes affect electroencephalographic activity, showing a correlation between serious thyroid diseases, panhypopituitarism and functions of the thalamus and hypothalamus (Untu et al., 2015).
On the other hand, it should be outlined that affective states are some of the factors that have a substantial impact on the endocrine glands (Baroiu et al., 2021). The central nervous system plays a significant role in the endocrine system, leading to dysfunction.
A one-year analysis (January-December 2017) was completed on a study sample consisting of 112 patients with mental disorders, hospitalized in the Psychiatry Clinic of the Craiova who also had a documented endocrinologic comorbidity. Endocrine diagnosis included obesity, diabetes, hyper- and hypothyroidism, gonadopathies, hyperprolactinemia. Prior to the inclusion in the study, patients signed an informed consent. Exclusion criteria were presence of suicidal thoughts, severe psychotic symptoms, addiction to psychoactive substances, including alcohol, ongoing pregnancy. The aim of this study was to establish how frequent and severe were the psychiatric comorbidities of the subjects, socio-demographic risk factors and endocrine-psychiatric correlations.
During the study, patients with both mental illnesses and endocrine comorbidities represented 7.2% out of the total of admissions. Sample distribution by age pointed out a substantial prevalence of endocrine comorbidities in patients over 46 years old – 73.21%, out of which 56.25% were patients between 46-60 years (Figure 1). The extreme age groups showed a lower incidence of endocrine comorbidities symptoms.
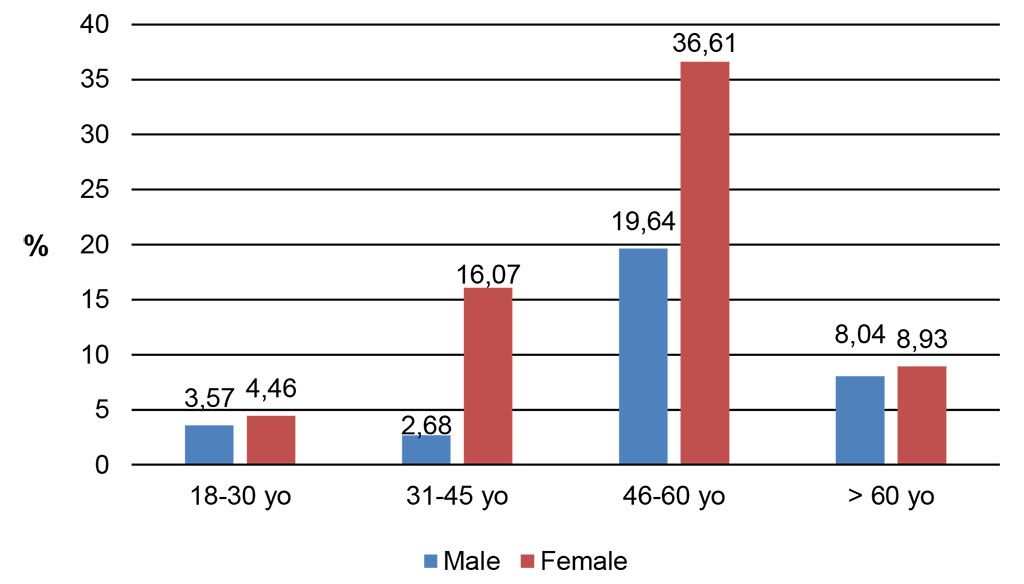
Figure 1. Sample distribution by gender and age group
Source: Authors' own conception
Similar distributions on gender can be found in young patients (under 30 years old) and elder ones (over 60), whereas in most of the cases between 31-60 years old, women were more likely to develop endocrine dysfunctions, especially around 45 years old, due to the premenopausal period.
The study of the sample revealed the prevalence of thyroid disorders – 55.36%, followed by gonadal disorders – 24.11% (Figure 2). Metabolic disorders (diabetes, obesity) and hyperprolactinemia had similar percentage – 9.82%, respectively 10.71%. Regarding the gender distribution of endocrine dysfunctions, visible differences were found only in the group of thyroid disorder. The values of the rest of the disorders are similar one to another.
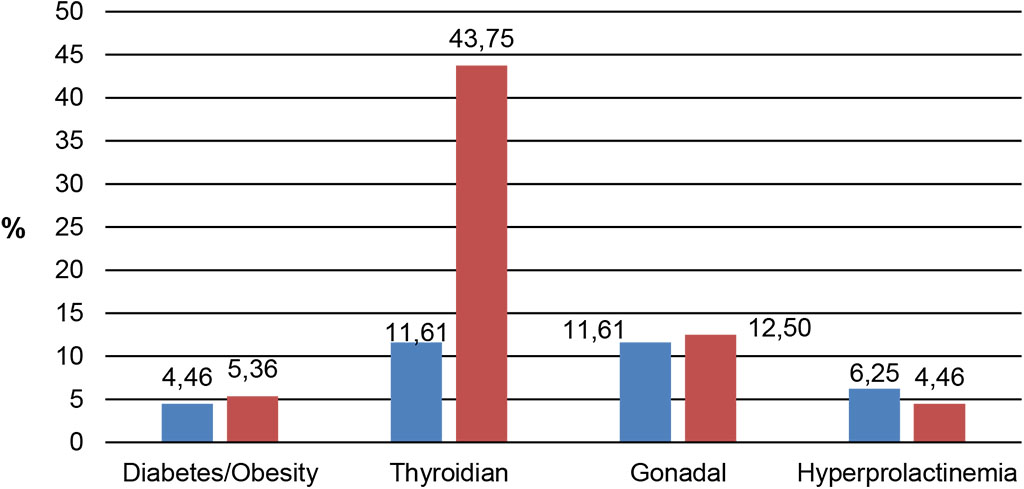
Figure 2. Sample distribution by gender and endocrine
pathology
Source: Authors' own conception
Mental disorders associated to endocrine dysfunctions were narrowed down and classified into the following categories: affective (including depression, with or without anxious symptoms and mania), psychotic (this group including schizophrenia, delirium, acute psychosis) and personality disorders. If we correlate mental disorders with endocrine dysfunctions, it turns out that depression seems to be the most frequent diagnosis associated with endocrine dysfunctions, except for the cases of hyperprolactinemia, where psychotic episodes were more frequent (Figure 3). Therefore, we are more likely dealing with a reverse cause, because high levels of hyperprolactinemia may mean side effects of the antipsychotic treatment administered.
Mania was also correlated with thyroid (hyperthyroidism); manic symptoms could also represent a side effect of the therapeutic use of thyroid hormones. A similar pathogeny can be found in the presence of manic symptoms from endocrine and metabolic disorders, as it is known that certain drugs used to control body weight may lead to mood and behavior disorders, especially if these substances are not administered under strict medical surveillance. Patients suffering from thyroid disorders showed psychotic symptoms or personality disorders, to a lesser extent, the latter being especially present in cases of gonadic (5.36%) and endocrine and metabolic conditions (3.57%).
As we found many cases of depression, we differentiated this disorder between the types of endocrinopathies by performing a dynamic evaluation. We assessed the intensity of depressive symptoms during the period of hospitalization and on a 3-month follow up, using the Hamilton depression rating scale (HAM-D 17) applied at admission, after a week of hospitalization, at discharge, after one and three months.
The results of the assessment were different, according to the type of endocrinopathy. Patients suffering from diabetes/obesity developed a lower level of depression at onset, from the very first week, so after a long period of linear decrease, they were rated as normal (non-depressive, HAM-D<7) at the endpoint. In patients with thyroid and gonadal disorders, the intensity of depressive symptoms, of moderate intensity at onset (close to severe in gonadopathies) had a slower pace of decrease, with a later improvement, as at endpoint, many patients, especially with hypothyroidism, still had mild symptoms of depression (Figure 4).
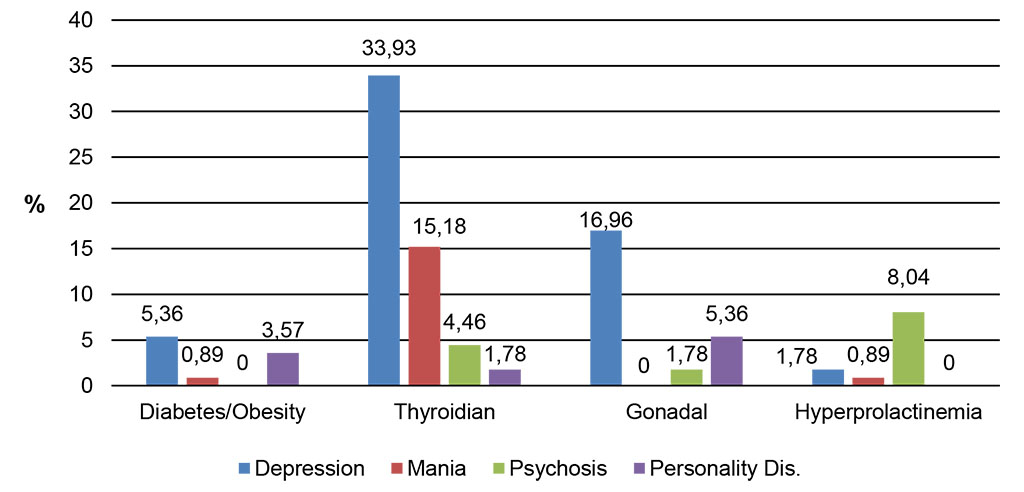
Figure 3. Sample distribution by endocrinological
comorbidities
Source: Authors' own conception
We performed a separate dynamic analysis of items 4, 5, 6 (for sleep disorders), as well as for items 9, 10, 11 (anxiety/agitations), according to the psychiatric symptoms experienced by most of the patients. Patients with diabetes/obesity were affected by medium insomnia, waking up frequently during the night, and most of them had nightmares. We also noticed that sleep disorders persisted and become acute in patients with diabetes and obesity during their first assessment week. Patients with thyroid dysfunctions, with initial severe insomnia, had difficulties staying asleep and were not able to return to sleep when waking up early in the morning (late insomnia). Patients with gonadal disorders had difficulties in falling asleep (early insomnia). Sleep disorders improved during the study period, as patients received a specific treatment after psychiatric assessment (Figure 5).
Patients with thyroid dysfunctions were more likely to experience symptoms of anxiety or agitation. The evolution of these symptoms was linear, in some cases with the persistence of moderate anxiety symptoms, observed in gestures and mimics. During the study, anxiety in gonadal disorders, first manifested by somatoform features, had a positive course; in endocrine-metabolic disorders, anxiety was highlighted by symptoms of irritability and respiratory somatic symptoms (Figure 6).
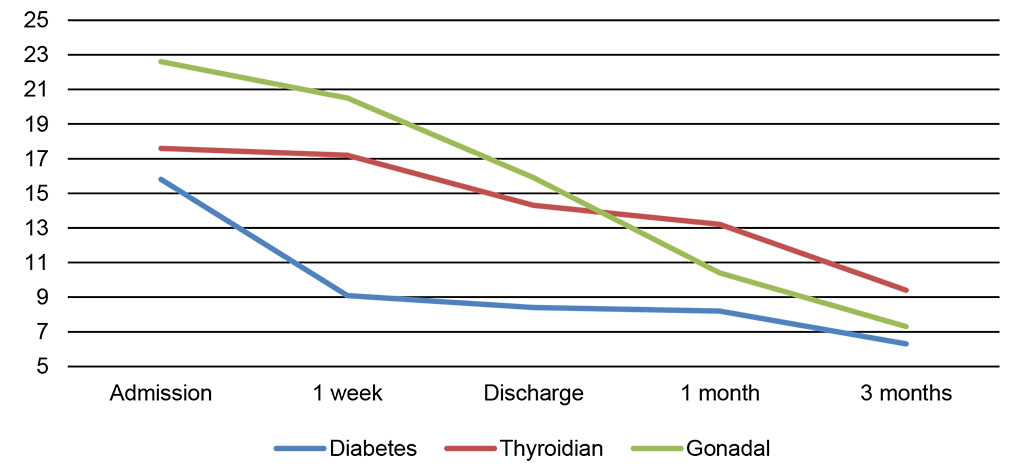
Figure 4. HAM-D scoreevolution
Source: Authors' own conception
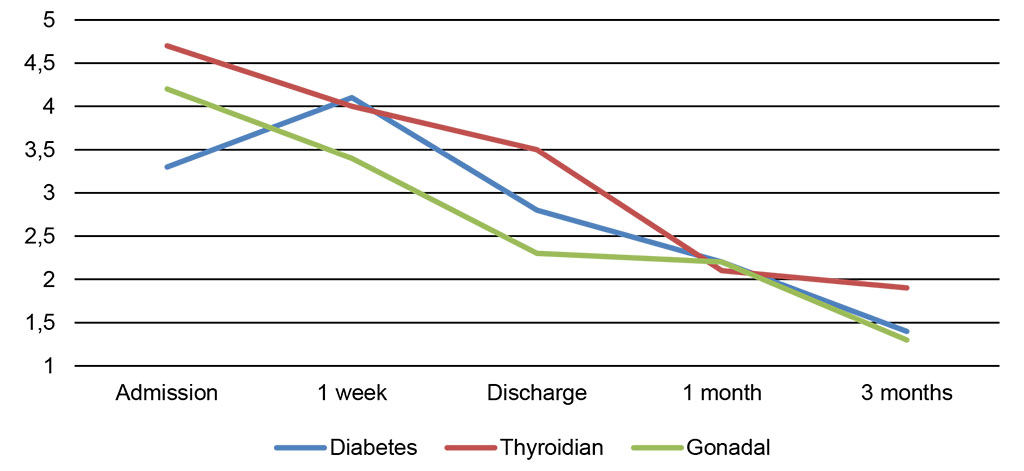
Figure 5. HAM-D subscores: insomnia outcome
Source: Authors' own conception
A global marker of evolution was represented by a high number of admissions in psychiatric wards during the study period. All in all, the study sample had a positive evolution, with a high prevalence of one single admission (Figure 7). The sub-group of patients with hyperprolactinemia proportionally registered a higher rate of hospitalizations for psychotic re-occurrences. It is worth mentioning the fact that medically induced hyperprolactinemia was totally remitted, in these patients, when switching to an antipsychotic drug with reduced side effects.
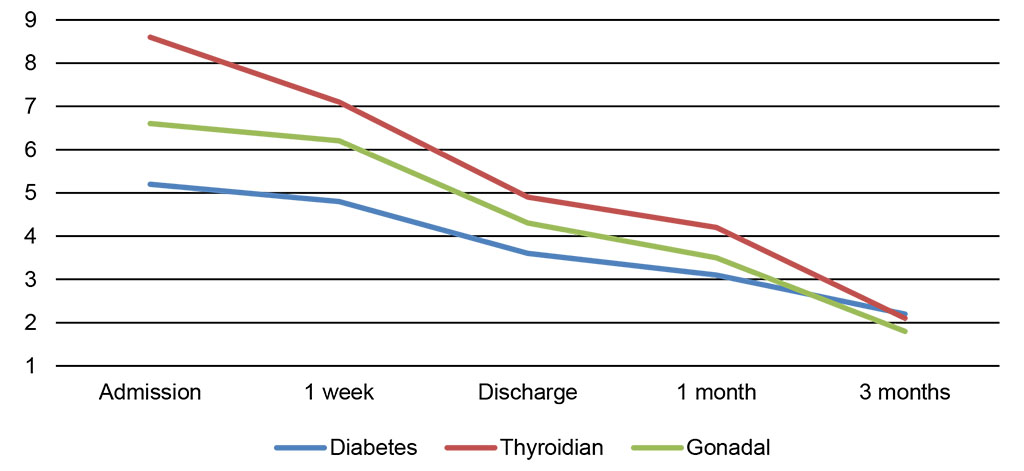
Figure 6. HAM-D subscores: anxiety/agitationoutcome
Source: Authors' own conception
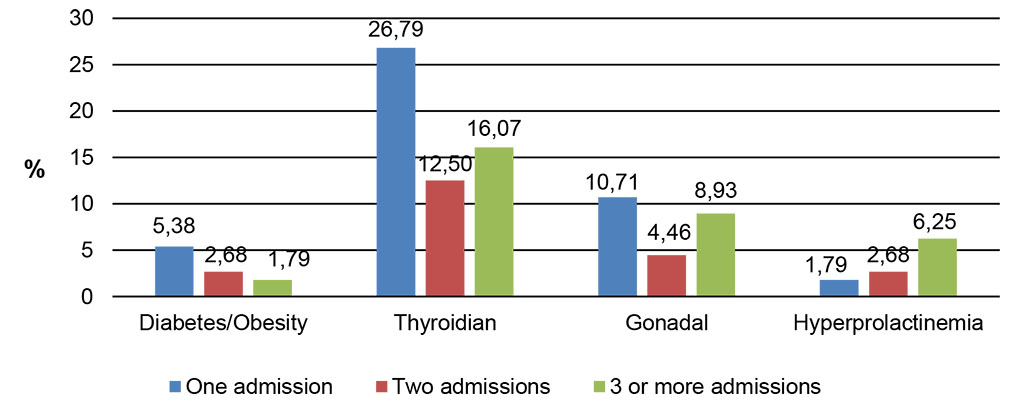
Figure 7. Sampledistributionbyadmissions in psychiatricwards
Source: Authors' own conception
Psychiatric symptoms in endocrine disease of various types and intensity distinguish themselves and develop according to the affected endocrine gland, its hypo- or hyperfunction and the specific drugs used to cure it. Under these circumstances, interdisciplinary collaboration becomes extremely useful, confirming the benefits of outlining psych neuroendocrinology as a transdisciplinary clinical field. This continuously improved collaboration stands for the dynamic relationship between the two disciplines, by stimulating addressability, by establishing theoretical foundation in the study area and last, but not least, by shaping an individualized therapeutic strategy.