- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.22
Introduction: Dementia is an important public health problem, the only cause of death that can not be treated or cured. The number of people who are diagnosed with dementia is increasing, over 55 million patients in 2021(about 5% of the world population), more than that a new case is diagnosed every 3 seconds, according World Health Organization. Prevalence of dementia is increasing, both before and after stroke.
Aim: The purpose of this paper is to emphasize the importance of early identification of the risk factors associated with cognitive decline and the role of the complex health care approach.
Method: The retroactive study involved analyzing the medical record of 60 subjects with stroke and cognitive impairments, hospitalized between july -december 2021. Furthermore we searched the latest PubMed database and Cochrane Library regarding the risk factors common for this two pathologies.
The outcome showed that more women are affected by this debilitating disease, of which 72% were over 80 years old. The following modifiable risk factors were identified: 63% of patients had hypertension, 42% had recurrent stroke, 37% atrial fibrillation, 26% type II diabetes, 22% dyslipidemia, and 10% obesity.
It is believed that one third of cases can be prevented by early identification of risk factors, especially cardiovascular, and by increasing the efficiency recovery after stroke. This can be done before the onset of the disease, growing the mental and emotional health, specificaly the cognitive abilitiy, including the executive function and the memory of people prone to neurodegeneration or cerebrovascular lesions.
In elderly subjects, healthy diet, moderate physical activity, chronic stress reduction, social interaction along with improvement in cardiovascular risk factors, could be considered the first line of defense against the development and progression of dementia.
Conclusions: The pathological process begins long before it manifests itself clinically, thus providing the opportunity to identify or combat the prodromal stages of the disease forward. We recommend multifactorial intervention to prevent cognitive impairment and dementia.
Keywords: dementia, stroke, prevalence, risk factors, prevention, cognitive decline.
According to the latest statistics: following a stroke, two thirds of patients had a cognitive impairment and after 3 months 10% are focused on dementia (Pendlebury, 2012). The states of cognitive dysfunction prior to cerebral infarction are described under the umbrella of a progressive care dementia involving insidious neurodegenerative processes and vascular changes (Kalaria et al., 2016).
The population has become worried about the effects of memory loss as much as it is worried about cardiovascular disease or diabetes. Dementia is overwhelming not only for people who have it, but also for their families and caregivers. There is a lack of awareness and understanding of dementia in most countries, leading to stigmatization, barriers to diagnosis, and physical, psychological and economic impact on the whole of society (World Health Organization, 2022).
The World Health Assembly recognizes that dementia is a priority issue, endorsing in 2017 a global action plan aimed at preventing this disadvantaged disease and providing support to the sick (Patterson, 2018).
The cognitive impairment once established cannot be cured, which is a serious aspect because it is estimated that the deterioration process begins at an earlier age than thought however there are a multitude of risk factors and modifiable protection that can be approached to avert or temporize the onset of dementia (Mangialasche et al, 2012).
We conducted a seven months retroactive study, during July - December 2021, in the Department of Neurology and included 60 subjects. Inclusion criteria: stroke and dementia diagnosis. Exclusion criteria: Alzheimer disease. We identified the modifiable and non-modifiable risk factors that predispose or aggravate dementia in patients who have had a cerebral infarction.
The number of subjects with cognitive impairment is increasing, considering that medicine advances rapidly and the average level of life expectancy in Romania increased to 76,5 years until 2019, with a slight decrease during the pandemic years (World Health Organization, 2020). The dementia incidence correlates with age, with a major leap after 60 years.
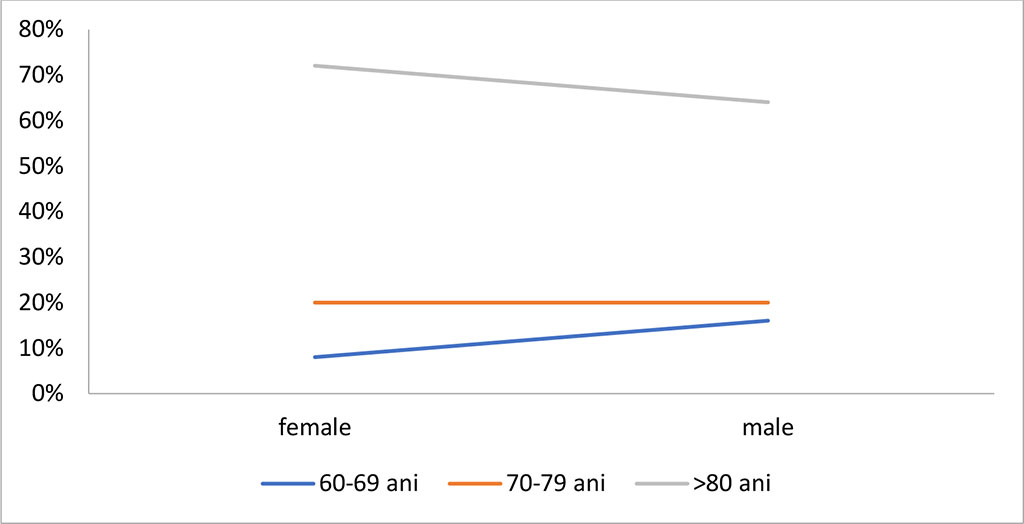
Figure 1. Incidence of dementia by gender and age in stroke
Source: Authors' own conception
In Figure 1 the results show that female sex was the most affected by this disabling disease, of which 72% were over 80 years old. Although it occurs on the sixth decade of life, dementia is not an unavoidable physiological process occurs caused by aging on the brain, there are also noticed in young subjects, over 30 years (World Health Organization, 2022).
The Rotterdam study showed that the seven different risk factors involved in developing dementia include: smoking, metabolic syndrome - overweight, hypertension and hyperglycemia, sedentariness - lack of cardio and resistance exercise training, low levels of education and mental disorder. The cumulative data from this study suggested that when the modifiable factors were addressed properly, the evolution towards dementia can be avert in third of the cases (De Bruijn et al., 2013).
In Figure 2 we underline the modifiable risk factors of the patients included in the study: 63% of patients suffer from arterial hypertension (AH), 42% had stroke recurrence, 37% atrial fibrillation (AF), 26% type II diabetes mellitus, 22% dyslipidemia and 10% obesity.
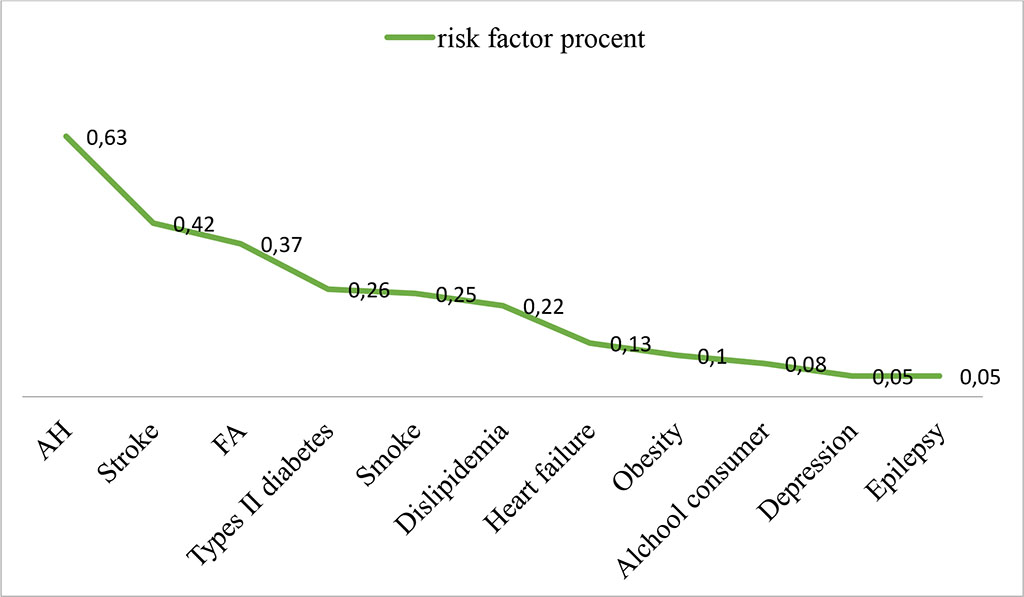
Figure 2. Modified risk factors for dementia associated with
stroke
Source: Authors' own conception
More studies investigate the impact of reducing the modifying risk factor on the health risk of brain, cognition and dementia (Rakesh et al., 2017).
FINGER is the first randomized controlled trial in 1,200 patients for 2 years that point out it is attainable to delay cognitive decline through a multifactorial intervention among the retired people. The results highlighted the value of the modified risk factors approach as a strategy to protect the health of the brain (Rakesh et al., 2017).
The Mediterranean diet based on the consumption of unsaturated fats in fish, cereals, fruits and vegetables associated with salt, sugar and alcohol reduction has beneficial effects on memory, language, executive function and is also in line with the recommendations on reducing cardiovascular risk disease. DASH Diet Association, for hypertension, can have a major impact on cognitive decline in older people (Grigoras & Ciubara, 2021; Morris et al., 2015).
According to the Finnish study the aerobic exercise (walking, running, gymnastics), postural and muscle growth for the 8 main muscle groups, performed three or four times a week, half hour, better one hour per training, slows progression to dementia (Kivipelto et al., 2013; Untu et al., 2015). Elderly with a normal cognitive function that performed regular exercises with moderate intensity exhibited a lower risk of cognitive decline over 8 years (Chu et al., 2015). In people with cognitive impairment exercise can improve spatial and verbal memory (Nagamatsu et al., 2013).
The negative impact of chronic psychosocial stress and charged on cognition can be countered that interventions, such as regular meditation or yoga, aimed at controlling the level of stress (Baroiu et al., 2021). Cognitive recovery is a complex therapeutic intervention that plays an essential role in the multidisciplinary rehabilitation of dementia, consisting of behavioral control strategies served by the personal rehabilitation psychologist to the entire team including here the family, strategies that emphasize the improvement of daily life and social interaction (Stern, 2012).
Anxiety and depression are frequently encountered problematic disorders, that influence attention, psychomotor speed, visual spatial skills and executive function (Fatu et al., 2020). All of this, with aging will have repercussions on cognitive function. (Butters et al., 2000). Depression should be recognized and treated properly, both by pharmacological means: selective serotonin reuptake inhibitors, tricyclic antidepressants (with low efficacy in the elderly and increased risk of ischemic or hemorrhagic stroke), but notably by non-pharmacological therapies.
When three or more components of the metabolic syndrome (blood pressure, cholesterol and triglycerides, blood sugar- conditions predisposing to vascular lessions) are addressed and brought under control, it is optimized to delay the onset of cognitive decline and reduce the risk of mortality. It is known that the treatment for increased tension could only drop the risk of vascular dementia however subjects without cerebrovascular lesion, like neurodegenerative disease (in Alzheimer disease or senile dementia), will have no benefits, even more can be affected by this cure (Chang-Quan et al., 2011).
Patients with diabetes mellitus type II have up to three times the risk of developing dementia, even after adjusting for other vascular risk factors (Ott et al., 1996). Diabetes accelerates microvascular pathology in the brain, also causing cognitive impairment through fluctuations in glucose and insulin levels in the blood that may affect beta amyloid clearance (Bruce et al., 2001).
Atrial fibrillation and the derived factors such as high levels of lipoprotein (a) and homocysteine, prothrombotic conditions, the high sensitive C reactive protein (hs CRP) , can produce coronary artery and cerebrovascular diseases, the latter have an increased risk of progressive cognitive impairment culminating in dementia (Bunch et al., 2019). Considering that ischemic lesions in the cerebral arteries caused by tachyarrhythmia predispose to the association of AF with dementia, it is crucial to control the heart rate, with the return to sinus rhythm and the early initiation of anticoagulation (Thacker et al., 2013). Patients treated with anticoagulants at the time of FA diagnosis have a thirth lower risk than subjects without cure, according to the latest studies (Friberg & Rosenqvist, 2018).
There is currently limited evidence to support the role of drugs used for dyslipidemia, namely statins, in preventing cognitive decline or dementia. Instead, statins reduce the concentration of low-density lipoprotein cholesterol and of hs CRP. This will have favorable repercussion on endothelial activity and inflammation used to prevent stroke (Collins et al., 2004).
A recent meta-analysis showed that repetitive transcranial magnetic stimulation and direct transcranial current stimulation can remarkably enhace cognitive function on healthy older people and dementia subjects. A sustained cure, with repeated sessions, is necessary to optimize the preserved functions and improve the degree of damage (Hsu et al., 2015; Paduraru et al., 2019).
The pathological process begins long before it manifests itself clinically, thus providing the opportunity to identify or combat the prodromal stages of the disease forward. We can act to reduce the modifiable risk factors which, most of time, are common in stroke and dementia. In order to delay neuronal degradation, in addition to specific prophylactic strategies for cognitive rehabilitation, it is necessary to limit cardiovascular risk, psychosocial stress and anxiety episodes. This can be done with healthy lifestyle, progressive aerobic training and educational nutrition program.
However, we need randomized trials on larger groups of people to demonstrate certain preventive interventions benefit of people at risk.