- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.19
![]() baciu91@yahoo.com , carmengavrilaa@gmail.com
baciu91@yahoo.com , carmengavrilaa@gmail.com
Introduction: Human immunodeficiency virus (HIV) infection is often preceded or accompanied by neuropsychiatric symptoms, including depression. This fact has been evaluated in most of the clinical studies to date as associated with HIV infection already diagnosed.
Case report: We report a case of a 46-year-old woman patient with no prior diagnosed pathology, suffering from depressive disorder for roughly 6 months, with a progressive evolution under treatment. Blood tests showed a moderate normochromic normocytic anemic syndrome of unspecified origin. Given the fact that depressive syndrome has not improved under treatment, a cerebral computed tomography (CT) scan and a cerebral magnetic resonance imaging (MRI) are decided, revealing an expansive cerebral process which in turn recommends performing stereotactic biopsy, but the family of the patient refuses the procedure. The patient is neurologically evaluated and after considering the cerebral MRI pattern and the presence of anemia, an HIV and syphilis detection test is decided, revealing a positive result for HIV infection. An antiretroviral therapy has been initiated, resulting in favorable clinical and imaging outcomes.
Conclusions: Each patient and each case are individual and is to be approached as such. Depression in a progressive evolution under treatment requires imaging evaluation (cerebral CT scan, ideally cerebral MRI).
Keywords: Human immunodeficiency virus (HIV) infection, depression, expansive cerebral process, magnetic resonance imaging.
The major depression is the most frequent psychiatric manifestation associated with human immunodeficiency infection (HIV) (Arseniou et al., 2014; Dube et al., 2005; Bolos et al., 2012 2012) and it has a big influence over the quality of life on this patient. Even if a precocious diagnosis and the initiation of an antiviral therapy has led to a decrease in deaths caused by acquired immunodeficiency syndrome (AIDS), it is estimated that in 2030, HIV infection will be the main cause for disability followed by major depression disorder (Capuron et al., 2007; Carey et al., 2004; Mathers & Loncar, 2006; Nanni et al., 2015; Sandu, 2013; Sandu et al., 2017). And as the two conditions can coexist, the social impact will be even greater because depression in HIV-positive patients is a predictor of negative clinical outcomes (Păduraru et al., 2019; Mayston et al 2012; Nanni et al., 2015).
A review of the literature showed that only a few clinical studies assess depression as a risk factor for HIV infection (Nanni et al., 2015). These studies demonstrate that people with major depression disorder have an increased risk of infection, facilitating transmission of the human immunodeficiency virus (Carey et al., 2004; Grassi, 1996; Schenker et al., 2022). Rosenberg et al. highlighted a prevalence of HIV infection eight times higher among psychiatric patients compared to the general population (Rosenberg et al., 2001).
Meade and al. confirmed high prevalence of HIV infection among the patients with severe psychiatric disease (Meade & Sikkema, 2005). Most of these patients had behavioral disorders associated with increased transmission risk for HIV: unprotected sexual contact with multiple partners and administration of intravenous drug with the syringe (Meade & Sikkema, 2005; Nanni et al., 2015). Also, patients with severe depressive disorders have a probability of five times higher to have unprotected intercourse, especially with a paid female partner (Armstrong et al., 2013, Lupu et al., 2017).
With regard to the association of depression with HIV infection, more research has evaluated the incidence of major depression among the HIV positive population. Even if depression is described in all phases of infection with HIV (Nanni et al., 2015), studies have shown a higher prevalence of major depressive disorders in the advanced stages of the disease. The prevalence of the major depression disorders among people with HIV infection varies form 7,2% to 71,9%, this being explained by the size of the sample, different scales and evaluation questionnaires that have been used in the studies (Chaudhury et al., 2016).
We present a 46-year-old woman’s case, with no prior medical history, that had been diagnosed and treated for depression for 6 months, depression that apparently occurred in full health status.
The patient was admitted in the medical department with great fatigue and progressive depression despite the treatment. Blood tests showed a normochromic normocytic anemic syndrome. An superior and inferior digestive endoscopy was performed without any results that could explain the anemic syndrome.
At this point it is worth mentioning from her anamnestic history that she was a divorced woman that had sexual intercourse with two partners in the last five years.
Because the state of the patient is worsening, and depression syndrome is progressive a cerebral computed tomography (CT) scan was performed and revealed a left fronto-parietal expansive brain process. A cerebral magnetic resonance imaging (MRI) with gadolinium contrast followed and showed a heavy solid mass in deep cerebrum area, in which gadolinium is captured peripherally. That mass was located fronto-parietal with extension to left basal nuclei (Fig. 1). A similar but smaller mass was discovered in left occipital area also.
The patient was transferred in the neurology department to continue the investigation due to suspicions of cerebral metastases. A thoracic-abdominal-pelvic CT scan was performed with no other neoplastic process found and all tumor markers were negative.
Without a clear etiologic diagnostic, the imagistic aspects and the presence of the anemic syndrome require an HIV and syphilis detection test revealing a positive result for HIV infection. The viral load in the blood determination was 1019520 copies/ml, lymphocytes T-CD4 - 72 cell/mm3, cerebrospinal fluid analysis with protein concentration of 79 mg/dl, glucose concentration of 44 mg/dl, elements number 1 cell/mm3, HIV-RNA 133922 copies/ml and fungal culture was negative. The serology for toxoplasma Gondi (immunoglobulin G) was positive.
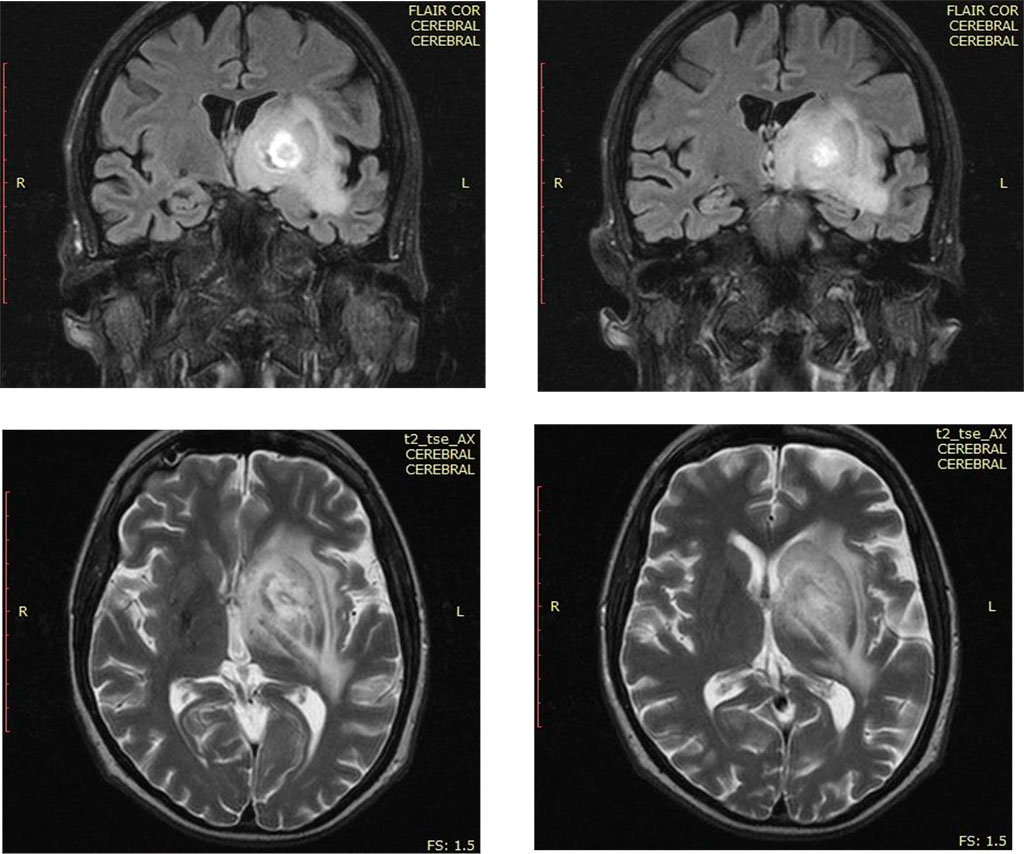
Fig.1. The
appearance of the cerebral MRI of the cerebrum tumor processe
Source: Authors' own conception
The therapy for human immunodeficiency and toxoplasmosis was initiated (the MRI imaging was extremely suggestive and the serology for toxoplasmosis was positive), with favorable evolution, improving overall state and depression and reducing the size of the intracerebral mass.
An association between depression and chronic illnesses is common, but it is often underdiagnosed and undertreated because symptoms like fatigue, insomnia, decreased appetite are commonly found both in depression and in chronic diseases (Rebegea et al 2019; Reis et al., 2017; Untu et al., 2015) or acute diseases (Baroiu et al., 2021). Additional there is a perception that depressive symptoms are just the negative consequences of the diseases (Reis et al., 2017; Teng et al., 2005).
Signs and symptoms of depression are similar in patients with HIV infection and in the ones without infection (Rădulescu et al., 2020; Nanni et al., 2015). The presence of apathy and anhedonia associated with diminished morning mood is more commonly caused by depressive illness (Nanni et al., 2015; Teng et al., 2005), while memory disorders and fatigue are more likely to be independent of major depression disorder, being caused by HIV infection by immune inflammatory neurogenic pathways (Alciati et al., 2007; Nanni et al., 2015).
Different studies and reviews have found a bidirectional association between HIV infection and depression, which implies a complex biological and psychosocial interaction (Nanni et al., 2015; Chaudhury et al., 2016).
Recent studies have confirmed a correlation between depression, low level of CD4 and large viral load in patients with HIV infection, announcing a faster progression to AIDS (Alciati et al., 2007; Leserman, 2003; 2008; Nanni et al., 2015). Patients with CD4 cells less than 200/mm3 had a 2,1 times higher risk of developing depression than patients with values of CD4 greater 500/mm3 (Reis et al., 2017).
The particularity of the case lies in the fact that a persistent depressive syndrome under treatment has led to the diagnosis of HIV infection, after imaging evaluation (cerebral MRI with contrast substance) and determining serology for HIV. Depression can be explained by the presence of cerebrum processes (cerebral toxoplasmosis) and may be secondary to the low number of T-CD4 lymphocytes (72 cell/mm3) and big viral load (1019520 copies/ml).
Managing depression among HIV-positive patients can lead to better prognosis, improves quality of life and increases adherence to medication (Ciobotea et al., 2016). The selective serotonin re-uptake inhibitors (SSRIs) are considered first-line medications for the treatment of depression in patients with HIV infection (Arseniou et al., 2014), sertraline and escitalopram being the first therapeutic option (Arseniou et al., 2014; Wolff et al., 2010). Treatment should be started with low doses and a slow titration to avoid complications especially in patients with advanced disease, or those with complex therapeutic regimens (Arseniou et al., 2014).
Patients with progressive depressive symptoms under treatment should be imagistic evaluated (cerebral CT or cerebral MRI).
Also, considering the increased incidence of HIV infection among psychiatric patients, HIV determination should be a routine test, especially in younger patients.
Physicians of HIV infected patients should be able to assess signs of depression and require psychiatric assessment whenever necessary. Identification and proper treatment of depression is an integral part of the care of HIV-positive patients.
The patient's informal approval has been obtained and recorded in the chart.
All the authors have equal contributions in this presentation.
This article does not contain any studies with human participants performed by any of the authors.
None
This article did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.