- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.15
Introduction: Anniversary depressions are characterized by a dispositional change dominated by sadness, revolt against "destiny", regret and often self-accusations and suicidal concerns. They reflect a close correlation with a stressful event, especially localized during the family lifetime, such as the death of the child, the parent, partner or other loved ones. Anniversary depression occurs spontaneously with the approach of the trauma event or even at the anniversary of it. Symptoms of depression may occur a few days or weeks before and culminate at the anniversary when some of the depressed guilty feelings are shut down in their own painful intimacy (with high suicidal risk) and the others revolt against the destiny and "the guilty". Aim: The objective of this study is to evaluate young people's opinions about anniversary depression. Method: A questionnaire derived from HAM-D (Hamilton Depression Rating Scale) was applied to a group of 56 students during the year 2019. A quantitative and qualitative assessment of young people's perception of depressive symptomatology was evaluated. Applied questionnaires comply with the privacy rules of Law 46/2003 (A) and EU Regulation 2016/679. Conclusions: From the investigated group it results than 93% know someone who has experienced a traumatic episode. Of the 56 examines a significant proportion know or have experienced a traumatic event with an impact on mood (79%). Behavioural changes associated with the traumatic event or recall of such an event (in decreasing frequency) are sleeping disorders 79%, mood disorders 77%, appetite change 48%, somatoform accusations 36%, suicidal tendency 30%, decreasing useful yields 25 %, feelings of guilt 21%, decrease in alcohol consumption 14%, increase in alcohol consumption 7%.
Keywords: depression, anniversary, traumatic event, remembrance.
Depression is a commonly found disease worldwide, affecting more than 300 million people worldwide. Chronic depression of mean or increased intensity can have a major negative influence on the affected person, decreasing its functionality in the workplace, at school, or within the family and the quality of life (Ciubara et al., 2015; Ciubara et al., 2018; World Health Organization, 2018).
The prevalence of depression and other mental illnesses is on the rise worldwide. In this sense, in the resolution of the 66th WHO General Assembly, the Comprehensive Action Plan for the Promotion of Mental Health 2013-2020 (World Health Organization, 2013) was adopted, a plan which includes a series of measures that are encouraged by WHO Member States initiate them to limit the burden of mental illness and ensure an optimal mental health status among the populations.
Sadness, loss of interest or pleasure, feelings of guilt or low self-worth, interrupted sleep or food, fatigue, and difficulty concentrating are all traits of depressive illnesses. Long-lasting or recurrent depression can significantly affect a person's capacity to perform at work, at school, or in daily life. When depression is at its worst, it might result in suicide (World Health Organization, 2017).
By 2020, depression is anticipated to overtake diabetes as the second greatest cause of disability globally, according to the World Health Organization. Depression is currently the fourth major cause of disability globally (Murray & Lopez, 1996).
According to almost all studies, women have a major depressive illness at a rate that is two times higher than that of men, and the peak age at which depression first appears is between 20 and 50 (Sadock et al., 2015; Van de Velde et al., 2010).
The typical symptoms of a depressive episode include a low mood, a loss of interest and delight, and a decline in energy that results in greater weariness and decreased activity. It is usual to feel extremely exhausted after only a brief effort. Other typical symptoms include poor focus and attention, low self-esteem, guilt-inducing thoughts, a lack of value for oneself, a depressing and pessimistic outlook on the future, thoughts of harming oneself or suicide, disturbed sleep, and decreased appetite. It takes at least 2 weeks to diagnose a depressive episode, regardless of how severe it is, while shorter intervals may be acceptable if the symptoms start suddenly and are extremely severe (World Health Organization, 1993).
The major depressive disorder has to meet the following diagnostic criteria:
A. The same two weeks, at least five of the following symptoms have been present interval and signify a shift from prior functioning; at least one symptom either a low mood or a lack of interest or pleasure.
B. The symptoms affect social, occupational, or mental functioning clinically severe distress or impairment, any other crucial components of functioning C. The event cannot be linked to a substance's physiological side effects or another illness. D. Schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specific and unspecific schizophrenia spectrum disorders or other psychotic diseases do not provide a more compelling explanation for the occurrence of the major depressive episode. E. Neither a manic nor indeed a hypomanic episode has ever occurred (American Psychiatric Association, 2013).
Anniversary depressions are characterized by a dispositional change dominated by sadness, revolt against "destiny", regret, and often self-accusations and suicidal concerns. They reflect a close correlation with a stressful event, especially localized during the family lifetime, such as the death of the child, the parent, partner, or other loved ones.
Anniversary depression occurs spontaneously with the approach of the trauma event or even at the anniversary of it. Symptoms of depression may occur a few days or weeks before and culminate at the anniversary when some of the depressed guilty feelings are shut down in their painful intimacy (with high suicidal risk) and the others revolt against destiny and "the guilty".
Near the anniversary of the traumatic event or even on the anniversary date, individuals may experience depressive disorders, however, there is a degree of symptomatology that is dependent on exposure to actual or threatened death, serious injury, or sexual assault in one of the following ways: directly going through the traumatic event; seeing it happen to others in person; going through repeated or extreme exposure to the traumatic event's aversive details or learning that the traumatic event happened to a close friend or family member. When a family member or acquaintance is going to die or is in danger of dying, the incident had to be violent or unintentional.
Anniversary depression is influenced by several risk factors including:
A non-randomized observational prospective study was conducted in the "Elisabeta Doamna" Psychiatric Hospital of Galați. The database was made up of 56 students, with ages between 22 and 54 years, who was applied a questionnaire derived from HAM-D (Hamilton Depression Rating Scale) during the year 2019. A quantitative and qualitative assessment of young people's perception of depressive symptomatology was evaluated. Applied questionnaires comply with the privacy rules of Law 46/2003 (A) and EU Regulation 2016/679. For diagnosis to depressive disorder, we used criteria from the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders (DSM–5). The collected data was compiled and analyzed using JASP version 0.9.2.0, SOFA Statistics version 1.4.6. and Microsoft Excel version 2010.
For the categorical variables (gender, the environment of origin, age) were estimated the relative frequency (the reported number to the total number), the absolute frequency (number) and the central trend. Standard error mean (SEM) was calculated to determine a 95% confidence interval for the arithmetic mean (CI95%).
The mean age of the pacients was 31,41 (SEM: ±1,35) ) [CI95%: 30.51 to 32.95] years, mentioning that the distribution had an important negative skewness (-1.89), the median was 25.5 , standard deviation 10.1, minimum 22 and maximum 54.
The value mean of the feminin gender was 31.36 [CI95%: 28.63 to 34.09], standard deviation 9.74, p-value ˂ 0.001 (3.775e-6) was statistically significant and for masculin gender the mean was 31.71 [CI95%: 21.88 to 41.54], standard deviation 13.26.
Table 1 – Distribution by gender - ANOVA test indicate that there are statistical differences.
| Group | N | Mean | CI 95%3 | Standard Deviation4 | Min | Max | Kurtosis5 | Skew6 | p abnormal7 |
| F | 49 | 31.367 | 28.639 - 34.096 | 9.744 | 22.0 | 50.0 | -1.367 | 0.529 | < 0.001 (3.775e-6) |
| M | 7 | 31.714 | 21.889 - 41.540 | 13.263 | 22.0 | 54.0 | -0.942 | 0.905 | Unable to calculate overall p for normality test |
Source: Authors' own conception
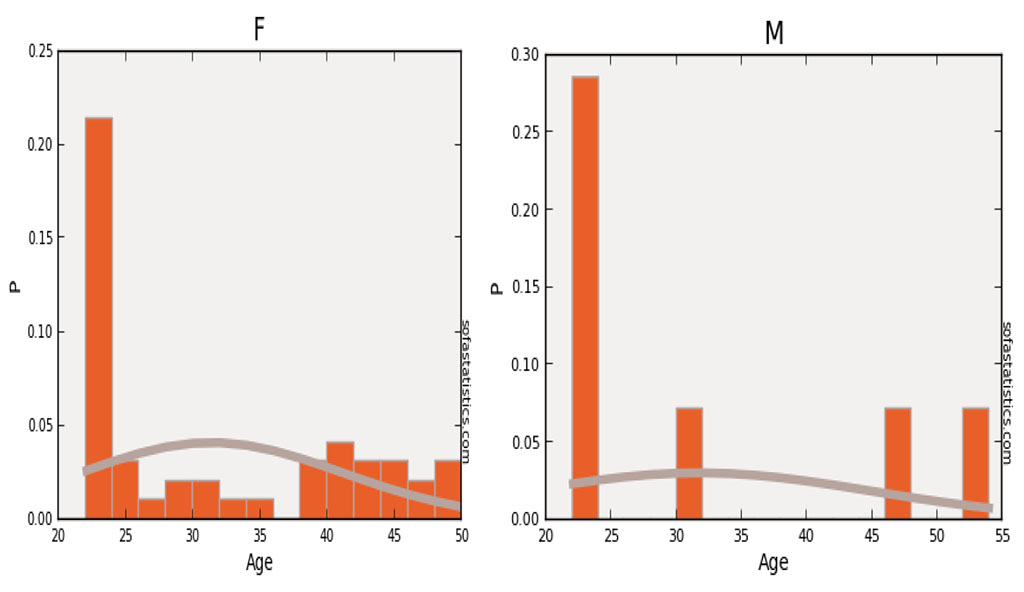
Figure 1. Distribution by age and gender
Source: Authors'
own conception
The average distribution of the phenomenon in the rural environment was 27.11 [CI95%: 22.15 to 32.07], standard deviation 7.59, p-value ˂ 0.001 (2.260e-4) was statistically significant and the mean in the urban environment was 32.23 [CI95%: 29.26 to 35.20], standard deviation 10.37, p-value ˂ 0.001 (1.813e-5) was statistically significant.
Table 2 – Distribution by environment of origin - ANOVA test indicate that there are statistical differences.
| Group | N | Mean | CI 95%3 | Standard Deviation4 | Min | Max | Kurtosis5 | Skew6 | p abnormal7 |
| R | 9 | 27.111 | 22.152 - 32.070 | 7.590 | 22.0 | 46.0 | 2.480 | 1.922 | < 0.001 (2.260e-4) |
| U | 47 | 32.234 | 29.267 - 35.201 | 10.378 | 22.0 | 54.0 | -1.356 | 0.460 | < 0.001 (1.813e-5) |
Source: Authors' own conception
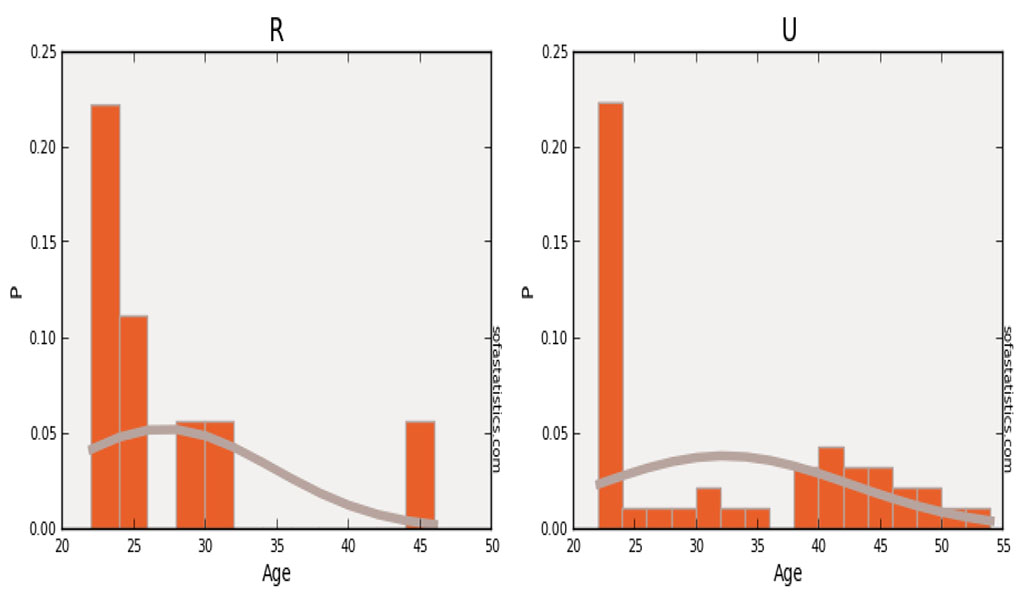
Figure 2. Distribution by age and the environment of
origin
Source: Authors' own conception
The applied questionnaire, derived from HAM-D, consists of 11 questions.
The first question has the mean value for yes 31.38 [CI95%: 28.64 to 34.12], standard deviation 10.09, p-value < 0.001 (8.693e-4) was statistically significant and the mean for no was 31.75 [CI95%: 20.22 to 43.27], standard deviation 11.75.
Table 3 – Distribution of answers to the first question - ANOVA test indicate that there are statistical differences.
| Group | N | Mean | CI 95%3 | Standard Deviation4 | Min | Max | Kurtosis5 | Skew6 | p abnormal7 |
| Da | 52 | 31.385 | 28.641 - 34.129 | 10.096 | 22.0 | 54.0 | -1.149 | 0.642 | < 0.001 (8.693e-4) |
| Nu | 4 | 31.75 | 20.227 - 43.273 | 11.758 | 22.0 | 47.0 | -1.393 | 0.470 | Unable to calculate overall p for normality test |
Source: Authors' own conception
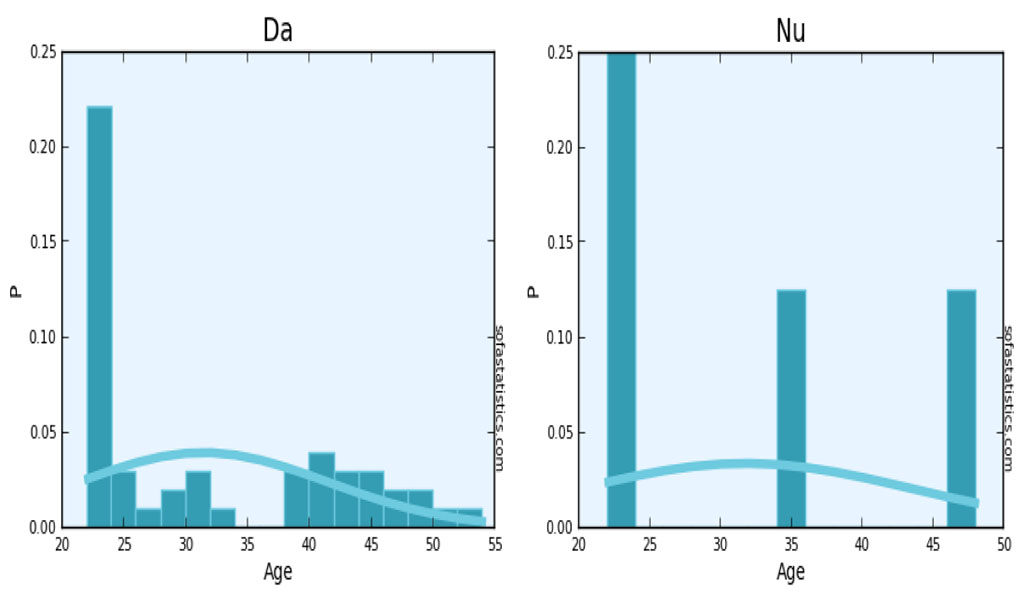
Figure 3. Distribution of answers by age
Source: Authors'
own conception
The second question has the mean value for yes 32.04 [CI95%: 29.00 to 35.08], standard deviation 10.28, p-value < 0.001 (7.817e-4) was statistically significant and the mean for no was 29.08 [CI95%: 23.72 to 34.44], standard deviation 9.47, p-value 0.2020.
Table 4 – Distribution of answers to the second question - ANOVA test indicate that there are statistical differences.
| Group | N | Mean | CI 95%3 | Standard Deviation4 | Min | Max | Kurtosis5 | Skew6 | p abnormal7 |
| Da | 44 | 32.045 | 29.008 - 35.083 | 10.280 | 22.0 | 54.0 | -1.252 | 0.538 | < 0.001 (7.817e-4) |
| Nu | 12 | 29.083 | 23.724 - 34.443 | 9.472 | 22.0 | 47.0 | -0.706 | 0.990 | 0.2020 |
Source: Authors' own conception
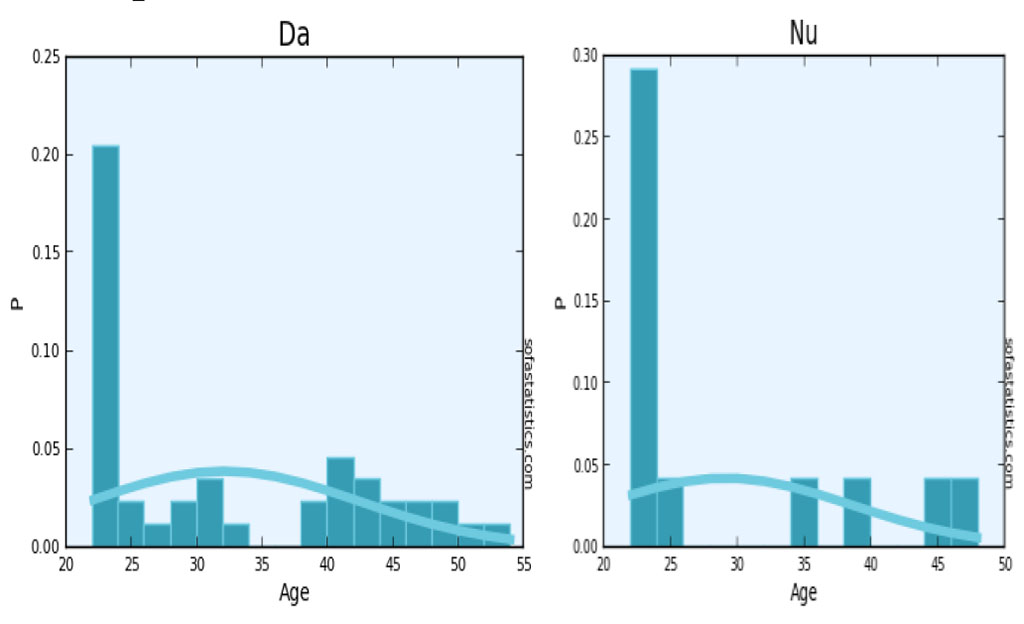
Figure 4. Distribution of answers by age for the second
question
Source: Authors' own conception
The third question has the mean value for yes 31.09 [CI95%: 28.00 to 34.18], standard deviation 10.34, p-value 0.01089 and the mean for no was 32.46 [CI95%: 27.25 to 37.66], standard deviation 9.57, p-value 0.04040. The four question has the mean value for yes 37.5 [CI95%: 28.61 to 46.38], standard deviation 12.81, p-value0.2607 and the mean for no was 30.39 [CI95%: 27.74 to 33.04], standard deviation 9.36, p-value 6.591e-3. The fifth question has the mean value for yes 31.23 [CI95%: 26.10 to 36.36], standard deviation 10.79, p-value 0.2037 and the mean for no was 31.48 [CI95%: 28.36 to 34.60], standard deviation 9.93, p-value < 0.001 (6.118e-5) was statistically significant. The sixth question has the mean value for yes 34.5 [CI95%: 27.96 to 41.03], standard deviation 12.48, p-value 0.04158 and the mean for no was 30.38 [CI95%: 27.62 to 33.13], standard deviation 9.12, p-value < 0.001 (6.384e-4) was statistically significant. The seventh question has the mean value for yes 32.52 [CI95%: 27.52 to 37.32], standard deviation 10.08, p-value 6.524e-3 and the mean for no was 30.92 [CI95%: 27.72 to 34.12], standard deviation 10.20, p-value 0.03281. The eighth question has the mean value for yes 40.75 [CI95%: 33.27 to 48.23], standard deviation 7.63 and the mean for no was 30.69 [CI95%: 27.98 to 33.40], standard deviation 9.96, p-value 7.905e-3. The nineth question has the mean value for yes 34.81 [CI95%: 30.69 to 38.93], standard deviation 10.91, p-value < 0.001 (5.217e-4) was statistically significant and the mean for no was 28.24 [CI95%: 25.23 to 31.25], standard deviation 8.26, p-value 0.02501. The tenth question has the mean value for yes 31.83 [CI95%: 26.00 to 37.65], standard deviation 10.29, p-value 0.2489 and the mean for no was 31.29 [CI95%: 28.29 to 34.30], standard deviation 10.16, p-value 4.493e-3. The eleventh question has the mean value for yes 31.55 [CI95%: 26.86 to 36.23], standard deviation 10.69, p-value 0.1690 and the mean for no was 31.33 [CI95%: 28.09 to 34.57], standard deviation 9.91, p-value 1.822e-3.
From the investigated group it results than 93% know someone who has experienced a traumatic episode. Of the 56 examines a significant proportion know or have experienced a traumatic event with an impact on mood (79%). Behavioral changes associated with the traumatic event or recall of such an event (in decreasing frequency) are sleeping disorders 79%, mood disorders 77%, appetite change 48%, somatoform accusations 36%, suicidal tendency 30%, decreasing useful yields 25 %, feelings of guilt 21%, decrease in alcohol consumption 14%, increase in alcohol consumption 7%.