- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.13
Introduction: The issue of sexuality is seldom investigated by psychiatrists in psychotic psychiatric patients, partly due to the frontline distressing psychiatric and behavioural symptoms but also due to hesitancy, haste, reluctance. Even though, the aspects of intimacy, sexual functioning are important and bothering, especially for young patients. These sexual impairments might be attributed to the disease itself but also to the medication.
Material and Methods: Two separate studies aim to investigate sexual disorders in female inpatient patients diagnosed with schizophrenia and in different phases of bipolar disorder (depression, manic) in comparison to controls. Therefore, treatment emergent sexual side effects (UKU scale), their relation to psychopathology (PANSS, GAF), quality of life (WHO-QOL Bref), misbelieves (Sexual Dysfunctional beliefs Questionnaire) were explored in chronic female schizophrenic patients and compared to matched controls. For the bipolar group, the depressed, manic women and controls were assessed regarding frequency of sexual intercourse, fantasies, desire, and lubrication orgasm by the Sexual Disorders Interview, Female Sexual Index and psychopathology by BDI, respectively YMRS. Both studies were cross-sectional and collected various demographical and therapeutical data.
Results: Schizophrenic patients rendered long histories of the disease and treatments, cumulating also disturbing side effects such as weight gain, amenorrhea, less marital and sexual partners. Low sexual interest, modest initiative, involvement, absent orgasm and sexual conservatorism were common and constant during exacerbations but also in chronicity being in connection rather to negative symptoms and modest functioning. Regarding bipolar women, sexual problems were detected in over 75% of the cases, with less implication and satisfaction during depression, pain, often blaming antidepressants as probable source of dissatisfaction. On the other hand, manic patients display more vivid sexual fantasies and interest, with higher arousal and lubrication, attending sexual satisfaction but being disturbed subjectively by some of these aspects. Although a wide range of sexual disorders might arise after treatment with antipsychotics, antidepressants, mood stabilizers, there could not be clearly ascertained a specific disorder.
Discussions: Hyposexuality seems to be a hallmark of schizophrenics even in treatment naïve patients, being more obvious after treatment, in chronicity. The issue of sexuality in bipolar women is rather difficult to assess and compare partly to the heterogeneity of the disorder.
Conclusions: Sexual disorders are a special and frequent issue in schizophrenia and bipolar women, displaying a wide range from low frequency, interest, dissatisfaction or even pain and a temporary phase limited exacerbation of sexuality during manic episodes.
Keywords: sexual disorders, schizophrenia, bipolar, women
Sexual disorders (SD) refer to a broad umbrella for various disorders, regarding sexual response cycle e.g., desire, arousal, erectile response, orgasm, ejaculation, genital and pelvic pain, which occur in more than 75% of sexual experiences, are enduring (more than three months), and produce distress and low quality of life (McMillan et al., 2017). Sexual functioning involves more than the above mentioned physiological sexual phases but also the relational engagement, marital satisfaction. Sexual disorders might be recorded in 30-80% (Baggaley 2008) of schizophrenia patients, the majority being attributed to treatment (Souaiby et al 2019). The situation of bipolar patients in this regard is more complicated, appreciating that almost one third complain of various sexual drive problems (Downey 2011), raising up to 80% in inpatients (Marzani-Nissen & Clayton 2004). It is usually ascertained that various drugs such as antipsychotics, antidepressants, mood stabilizers could trigger or aggravate SD, being the major source of noncompliance, especially in young and sexually active patients, with recent data of theratogenic effects of valproat acid (Ketter, 2010; Marzani-Nissen & Clayton 2004; Smith, 2007). These SD could be a hallmark of schizophrenia even before any treatment approach has been initiated, partly due to autism, negative symptoms, isolation, affective blunting, and abstract thinking problems (Marques et al., 2012; Radulescu et al., 2020). These SD are prominent during relapses but also in remission (Elkhiat et al., 2018). Among antipsychotics, prolactin raising ones (Olanzapine, Risperidone, Haloperidol, Clozapine) might be responsible of 40-60 % of SD but also those prolactine sparing could produce 16-27% of SD (Souaiby et al., 2019). Even though, the switch from first generation to second generation antipsychotics improved sexual functioning, still medication is seen as a major barrier against plenary expression of sexuality (Schenker et al., 2022; Souaiby et al., 2019). The studies regarding SD are sparse due to hesitancy, reluctance, in spite the disponibility of subjects and their interest to improve quality of life (Sandu, 2013a; 2013b), and self-fulfilment.
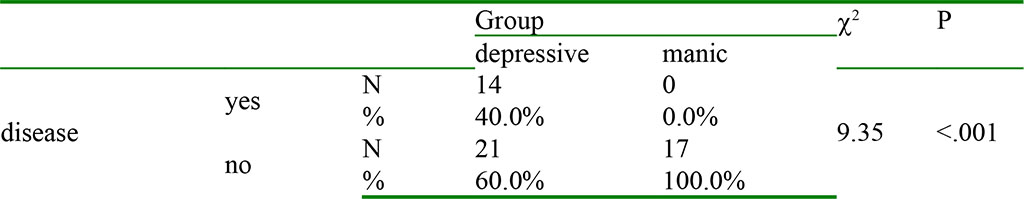
Two separate cross-sectional studies, with similar design, aimed to investigate the presence of sexual disorders in chronic schizophrenic and bipolar (depressive and manic) inpatient female patients and to relate these to severity of the disease, misbelieves. The design, partial results were previously published (Micluţia et al., 2008; Damian & Micluția 2013; 2015; Damian, 2016). The first study compared 50 female chronic schizophrenic inpatients, to matched controls and were explored by the following psychopatometric tools: PANSS, GAF-severity of the disease, treatment emergent sexual side effects (UKU Side-Effects Rating Scale), WHO-QOL Bref –quality of life, Sexual Dysfunctional Beliefs Questionnaire SDBQ. The second study, a broader PhD thesis (Damian, 2016), assessed severity of depression (BDI), mania (YMRS), frequency of sexual intercourse, fantasies, desire, lubrication, orgasm, dyspareunia (Sexual Dysfunction index-SDI, the Index of Female sexual Function-FSFI), SDBQ in 81 depressed, 31 manic and 61 matched controls. The inclusion criteria imposed the fulfilment of the diagnostic criteria according to ICD-10, the absence of organic disease that might induce sexual disorders (e.g., diabetes, neurological, endocrinological, urological, gynaecological, systemic diseases), comorbidities (alcohol, psycho-active substances misuse, dependence), contraceptive medication (Damian, 2016). All patients, admitted to the Second Psychiatric Clinic Cluj-Napoca, signed an informed consent and the evaluations were in accordance with the Helsinki requirements, receiving the approval of the local Ethics committee. A snapshot of some of the results will be presented.
There was stated from the very beginning that the focus was on chronic patients, e.g., at least three prior episodes had to be recorded since the disorder elapsed. The two samples were different not only from the diagnostic, therapeutical approach but also from the studied age, supposing the potential sexually active period: 18-55 years in the schizophrenia sample, respectively 10-62 years in bipolar patients (Damian, 2016; Micluţia et al., 2008). Among the demographical data, the two studies revealed similar age means e.g., 35.45 (SD=6.85) schizophrenia, versus depressed 40.19 (SD=11.4), and manic 42.19 (SD=11.4), ANOVA of the latter group (F=2.67, p>0.05) being nonsignificant (Damian, 2016; Micluţia et al., 2008). More interesting seems the onset age, the duration of the disease (over 8 years), exposure to treatment over 8 years (Table 1); a gap of over one year since the diagnosis and the treatment could be recorded in schizophrenia, depressed patients, while manic patients beneficiated sooner of therapy. There were used FGAs, SGAs, anticholinergics, anxiolytics, various types of antidepressants, mood stabilizers.
Table 1. Demographic data of the samples
| Diagnosis | schizophrenia | controls | depressive | manic | controls |
| N | 50 | 50 | 81 | 31 | 61 |
| Age (Mean, SD) | 35.45 (6.85) | 35.48 (8.24) | 40.39 (8.9) | 42.19 (11.4) | 37.62 (9.66) |
| Onset age | 26 (7.67) | 28 | 29 | ||
| Duration dg | 10.32 (6.55) | 9.3 | 8.1 | ||
| Duration tr | 9.31(6.06) | 8 | 8.1 |
Source: Authors' own conception
Similar level of education was recorded in all patients, but the employment status was generally below the educational level, with a special mention of the tremendous early and extended level of sick leave (64%) in the schizophrenia group (Micluţia et al., 2008). The marital status rendered evidence another situation that might be put in relation with the disease but also with sexual functioning: in spite the fact that the majority of patients were married or were engaged in a relationship, only half of the schizophrenia sample could keep their relation (Micluţia et al., 2008). Similar situation was noted in the bipolar sample, demonstrating a homogenous group sampling (F=2.67, p>.05) and education (F=5.25, p>.05) (Damian & Micluția 2013; Damian, 2016). 64% of schizophrenia inpatient women were sexually active (Micluţia, Popescu, & Macrea 2008). 54.4% (N=17) of manic, 43.3% (N=31) of depressive female inpatients were sexually active, being significantly inferior to controls 86.9% (N=53), chi-square-28.35, p<.001 (Damian & Micluția 2015; Damian, 2016). FSFI detected among the bipolar subjects, 75% sexual dysfunction, irrespective to depressive or manic pole (Damian & Micluția 2015; Damian, 2016) (Table 2).
Table 2 The prevalence of sexual dysfunctions in sexually active bipolar patients according to FSFI
| diagnosis | sexual dysfunction N, % | without sexual dysfunction N, % | Statically mean |
| depressive | 27 (77.1) | 8 (22.9) | c2 0.262 p>0.05 |
| manic | 12 (70.6) | 5 (29.4) |
Source: Authors' own conception
As with regard of the frequency of sexual intercourse, schizophrenic females reported in majority 78% less than one intercourse/month, out of these 36% having no intercourse (p<0.001) (Micluţia et al., 2008). Even though, 28% of schizophrenic patients were satisfied with their sexual life, in comparison to controls, with clinical statistical meaning (Micluţia et al., 2008). The bipolar sample reported 4.23 (SD=5.32) coitus/month in depressive women, and 4.24 in manic (SD=2.72) at t=0.005, p>0.05, but doubled as ideal frequency in manic patients (9.18, at t=2.89, p<0.05 (Damian, 2016).
An important issue is the level of psychopathology and sexual functioning. This has been investigated by PANSS scores and GAF scores in schizophrenia. Briefly, there could be noticed that the schizophrenia patients were moderate to severe ill, but stable during the admittance and evaluation. PANSS scores did not correlate with the frequency of sexual intercourse, with false beliefs about sexuality but positive correlate to the florid component of the positive subscale and number of partners (Micluţia et al., 2008). But more important, sexual satisfaction could be guaranteed by adequate adjustment, obvious by the GAF scale, and WHO-Qol Bref (Micluţia et al., 2008).
The psychopathology in bipolar sample, assessed by BDI in depressed patients and YMRS in manic patients did not show any significant correlation weather active/inactive sexually (Damian, 2016).
Table 3 Comparison between depressive and manic patients regarding the change of sexual interest due to the disease (Damian, 2016)
These results show the fact that depressive patients observed a reduction of their sexual interest attributable to illness. The query on SDI, FSFI indicated modest levels of desire, excitation, lubrication, sexual satisfaction in depressed patients (Damian, 2016). Depressive patients complained about pain during penetration (14). The major differences of SD within the bipolar group are outlined by Fig. 1.
| depression | mania |
| less sexual interest | intense sexual fantasies |
| rare sexual intercourse | high sexual arousal |
| discomfort | good lubrication |
| pain | sexual satisfaction |
Fig. 1. Patterns of sexual disorders in depression/mania (Damian, 2016)
The SDBQ has been validated on Romanian population (Damian, 2016). A ranking of the total scores of this scale in the psychiatric population emphasised higher scores than controls in all groups with comparable scores in schizophrenia and manic patients (Table 4). The merit of this tool is the highlight of misbelieves regarding sexuality. Schizophrenia patients showed total higher scores, more conservatism, sinful perception of sexuality and low body self-esteem (Micluţia et al., 2008). Within the domains of the scale, depressive and manic patients scored higher on all in comparison to controls (Table 4).
Table 4 Analysis of the mean, SD, total scores of the SDBQ items in schizophrenia, depressive, manic, controls (Micluţia et al., 2008; Damian & Micluția 2015; Damian, 2016)
| Items SDBQ | schizophrenia | controls | depressive | manic | controls |
| Sexual conserve | 30.96(5.31) | 19.9(7.97) | 25.96(8) | 31.44(6.98) | 22.18(4.33) |
| Sexual wish-sin | 17.72(3.73) | 11.68(4.59) | 12.6(4.33) | 18.16(5.78) | 11.58(4.38) |
| Age rel. beliefs | 16.6(3.14) | 11.2(3.61) | 13.3(3.48) | 16.96(3.6) | 11.95(2.74) |
| Body im. beliefs | 11.04(2.84) | 8.04(3.41) | 8.15(2.75) | 10.33 (3.5) | 7.5(2.65) |
| Denial affection | 22(3.51) | 19.3(1.9) | 19.23(3.35) | 21.23(2.36) | 18.01(2.54) |
| Motherhood primacy | 12.44(2.19) | 9.42(2.4) | 10.4(2,24) | 11,36(2.34) | 9.85(2.5) |
| Total | 110.7(14.4) | 79.54(20.48) | 89.14 | 109.48 | 81.07 |
Both samples of patients emphasised a special situation, that of hospitalised ones, isolated from their potential partners, on active medication, explaining partially the extend of the sexual impairments. If sexual interest and involvement of schizophrenia patients are modest even before the onset of the disorder due to the personality traits, they become more obvious during disease onset (van Bruggen et al., 2009) but are extensive in chronicity and long duration of treatment, unhealthy lifestyle, social drift, but also during remission. One major barrier is to dissociate disease driven SD from those triggered by medication. Negative symptoms, especially hinder initiation and joy of sexual relations, deterioration of intimate relations; frequent relapses, depression, and obesity might be as well important in this regard Certain features seem to be typical for female schizophrenia patients: the first sexual experiences, marriage, child bear might have occurred before disease onset and even when such SD are present, they are less obvious, accentuated during hospitalisations (McMillan et al., 2017). To the topic of sexuality in bipolar disorder: there is general agreement of hypersexuality, promiscuity, disruptive couple relations during manic, hypomanic episodes, less sexual interest, satisfaction in depression (Kopeykina et al., 2016). The hallmark is this great variability across polarities. Hyposexuality in manic bipolar I female patients has been observed by other authors as pain in depressive women (Elkhiat et al., 2018).
SD investigated in schizophrenic, bipolar female inpatients were detected and ranged from diminished sexual interest, involvement, low frequency of sexual intercourse, various dysfunctions of the sexual response cycle, conservatorism, sinful perception of sexuality. There could be established some patterns of sexuality in schizophrenia patients (anhedonic, with low sexual desire, moderate arousal, rare complete coitus) in depression (diminished sexual intererest, rare intercourse, dissatisfaction, dyspareunia) and in mania (intense sexual fantasies, high arousal, good lubrication, sexual satisfaction). These SD were modest associated with severity of psychopathology, improving with better adjustment.