- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.10
Introduction: Cervical cancer is the fourth most frequently found cancer among women worldwide. Numerous studies have underlined that persistent infection with human papilloma virus is the most important risk factor, two strains of the same virus – 16 and 18 being responsible for approximately 70% of the cases. Cervical cancer rarely metastasizes in the cervical lymph nodes and this indicates a poor prognosis. Literature data reports an incidence for left supraclavicular M1LYm of 0.1-1.5%. Material and Method: We bring attention to the case of a 44-year-old patient from the rural area who was diagnosed in January 2019 with stage IIIB cervical cancer, represented morphologically by a poorly differentiated squamous cell carcinoma. When admitted, the patient presented clinically with vaginal hemorrhage, intense abdominal and pelvic pain, fatigue, a dynamic, significant weight loss. The physiological personal history revealed nine pregnancies, the first one when she was 16. After pretherapeutic evaluation, the multidisciplinary committee decides performing simultaneous radio-chemotherapy with platinum salts. During the second week of treatment clinical examination revealed left cervical and supraclavicular adenopathy, both documented through imaging evaluation. Lymph node biopsy is done and its histopathological aspect, correlated with the immunohistochemistry profile supports the diagnosis of poorly differentiated squamous cell carcinoma lymph node metastasis. The initial treatment scheme is maintained, the patient being discharged with clinical remission of cervical and supraclavicular lymph node metastasis. Conclusions: The peculiarity of the case is determined by the distant metastases in the left cervical and supraclavicular lymph nodes, a rare finding during treatment, which was associated with a poor prognosis; in this case treatment was done for palliative purposes. Rapid diagnosis is the main factor that conditions the therapeutic results and chances for healing.
Keywords: Cervix, treatment, metastasis, supraclavicular lymph nodes.
According to estimations made by the World Health Organization (WHO) in 2018, cervical cancer is the fourth cause of malignancy among female patients worldwide. In the European Union, Romania occupies the first place in regard to cervical cancer death rates – 14,2 to 100.000 women (World Health Organization, 2012).
Many studies have revealed that certain strains of the human papilloma virus (HPV) are responsible for cervical cancer development. This virus is also frequently associated with other types of cancer: vulvar, vaginal, penile, oropharyngeal, anal. Approximately 120 HPV genotypes have been discovered until now, 15 of these being involved in cervical cancer development (Centers for Disease Control and Prevention, 2020; Penţa & Băban, 2014). Two strains – 16 and 18 are incriminated in the development of almost 70% of cancers (Castellsagué et al., 2009). Among the risk factors for HPV infection there are: early sexual intercourse initiation, multiple sexual partners, poor hygiene, multiparity. Clinically, cervical cancer is asymptomatic in early stages. When vaginal bleeding occurs (the most frequent symptom) it is possible that the malignant cells have already spread. Lymph node status is a prognostic factor of high value, the lymph node spread being associated with a poor prognosis (Creasman et al., 1987; DeVita et al., 2008).
We present the case of a 44-year-old patient from the rural area diagnosed in January 2019 with cervical cancer. The first admission is in the Gynecology Department. When admitted, the patient presented clinically vaginal hemorrhage, intense abdominal and pelvic pain, asthenia, adynamia, significant weight loss. From her physiological personal history, we notice 9 pregnancies, the first one when she was 16 years old, without significant pathological history. After the gynecological consultation a biopsy is taken from an ulcerated and vegetated exocervical mass. The pathology report diagnosed poorly differentiated squamous cell carcinoma. At gross inspection, the cervical squamous cell carcinoma reveals an exophytic, red, friable, ulcerated lesion. On the cut surface, the tumor is whitish grey, with areas of hemorrhage and/or necrosis.
Microscopic examination classifies squamous cell carcinoma in two categories: keratinizing or non-keratinizing. The patient presented the keratinizing variant, which is made up of sheets or nests of polygonal cells with intercellular bridges (desmosomes) and keratin pearl formation. The neoplastic squamous cell has large, hyperchromatic nuclei with coarse chromatin, the nuclear and cellular pleomorphism being variable. Concerning the degree of differentiation, the pleomorphism of the tumor with pseudo-glandular structures and <75% undifferentiated structures (Fig.1.) and <25% keratinization allowed for it to be classified as a poorly differentiated squamous cell carcinoma (G3).
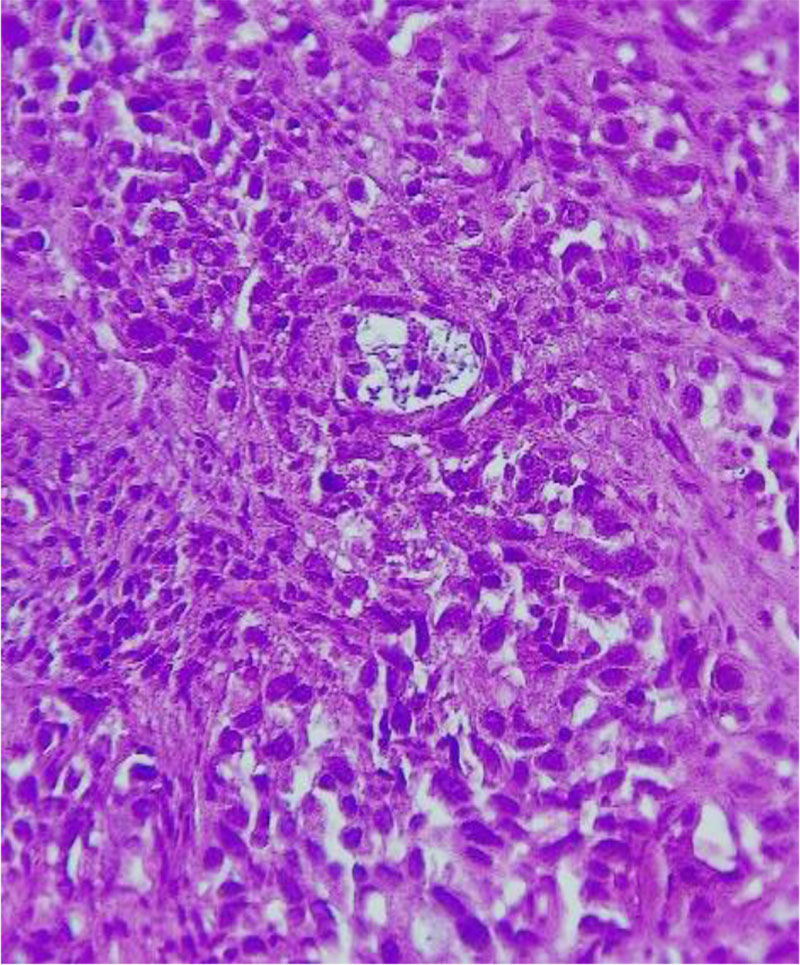
Fig.1. Poorly differentiated squamous cell carcinoma (G3).
Pseudo glandular area. H&Ex400
Source: Authors' own work
In February 2019 the patient is directed to the Radiotherapy Department for appropriate specialized treatment. When admitted, the local exam reveals a lower third smooth walled vagina cervix with an ulcerative-vegetated mass which measured 4/4 cm and hemorrhaged spontaneously and by valve examination, absent vaginal pouches, enlarged uterine corpus with low mobility and bilateral parameter infiltration that reached the pelvic excavation wall. Laboratory examination bring attention to the tumor markers, with values for cancer antigen (CA) 125 of 483 U/mL, CA-19.9 of 2710 U/mL, carcinoembryonic antigen (CEA) of 72,8 U/mL. We do not have available data for the squamous cell carcinoma antigen (SCCA). Thoracoabdominal and pelvic computed tomography (CT) did not reveal malignant pelvic adenopathy; the liver, pancreas and lungs did not have any discernable pathological alterations. The patient fell into the IIIB stage (T3bN0M0).
After pretherapy evaluation, the multidisciplinary committee decides on concomitant radio-chemotherapy treatment, along with brachytherapy. It is well tolerated by the patient, with no digestive or hematological toxicity. During the second week of treatment, clinical examination revealed left cervical and supraclavicular adenopathy. In this case the patient is evaluated through imaging studies which documented the presence of left cervical and supraclavicular lymph node enlargement, of a right renal, poorly iodophilic, heterogeneous image measuring a diameter of 16,5 mm (Fig.2), a globular cervix measuring 33 mm (Fig.2), with no retroperitoneal adenopathy and intense disk and bone structure alterations located at the level of the 4th and 5th cervical vertebrae.
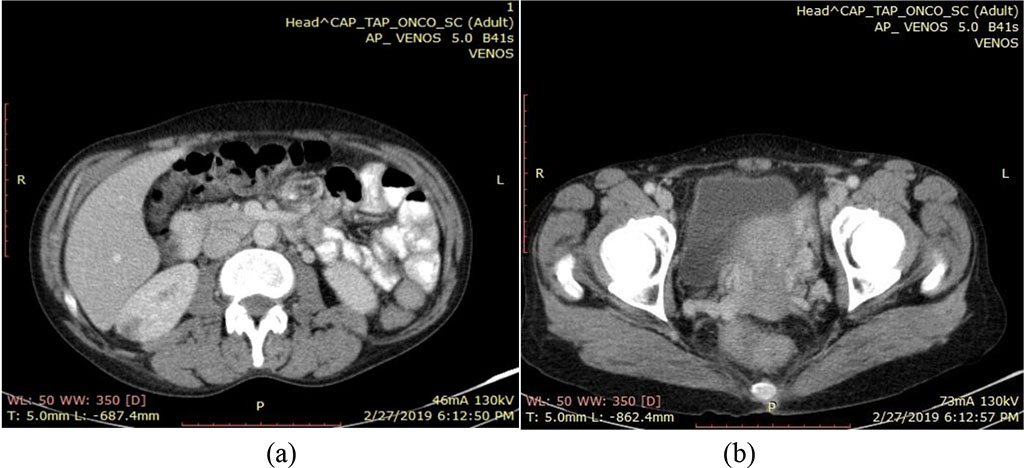
Fig.2. CT
scan February 2019 - (a) a right renal, poorly iodophilic,
heterogeneous image, and (b) globular cervix – 33mm.
Source:
Authors' own work
The patient is transferred to the otorhinolaryngology department (ENT) where the involved lymph nodes are biopsied. The pathology report reveals that the lymph nodes present a malignant, anaplastic cell proliferation. By immunohistochemistry examination CK7 and p63 are positive in the neoplastic cells, CK20 and ER are negative, and Ki-67 is present in 80% of cells. In conclusion, the histopathology aspect correlated with the immunohistochemistry profile reveals the diagnosis of poorly differentiated (G3) squamous cell carcinoma lymph node metastasis. Due to the similar histological aspect and degree of differentiation, we considered the left cervical and supraclavicular metastasis as having the cervix as onset.
The initial weekly treatment with platinum salts and cisplatin 40 mg/m2, respectively, along with external radiotherapy (RTE) is continued; the total dose (TD) is 46 Gy/23 fractions, with a dose/fr equal to 200 cGy. The patient is compliant and responds well to therapy, so that when discharged the cervical and supraclavicular adenopathy are in full clinical remission. She is redirected to another Radiotherapy center in order to complete her therapy dose with brachytherapy which she does not do due to personal reasons. We mention the lack of brachytherapy in our treatment center.
The patient continues cancer treatment with 2 series of carboplatin and topotecan. She develops moderate vomiting, first degree anemia and leucopenia which is corrected with granulocyte growth factors and cortisone formulas. During the treatment course, the patient benefited from psychological counseling.
In July 2019 she was admitted to the Radiotherapy Department for reevaluation. Clinically, the patient has no symptoms, with a performance index (PI) of 0. The hematology labs highlight the presence of a second-degree anemia with a hemoglobin value of 9,7 g/dL and a hematocrit of 28,80%, erythrocyte sedimentation rate of 40 mm/h and hypocalcaemia. The local gynecological examination reveals the cervix without a macroscopically evident neoplastic mass, vaginal telangiectasia, and supple parameters. A cytology exam is done and the Papanicolaou stained vaginal smear reveals post-radiotherapy alterations with large, atypical squamous cells, having a two-tone cytoplasm, finely granular chromatin, conspicuous nucleoli and irregular membrane, some with keratohyalin granules or with nuclear and/or cytoplasmic vacuoles. The presence of a predominantly neutrophilic granulocytic inflammatory infiltrate is associated with cytolysis and mature and immature squamous metaplasia (Fig.3). These aspects suggest a chronic postradiotherapy change, the data described needing clinical and laboratory correlations.
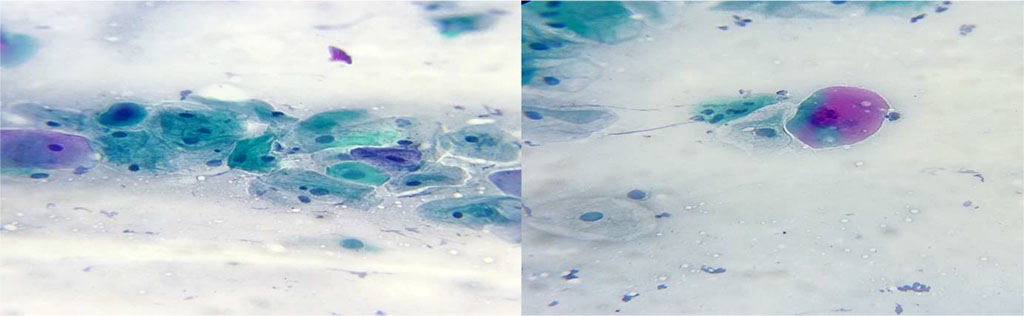
Fig.3. Atypical squamous cells of undetermined significance.
Changes suggestive for chronic postradiotherapy period. Papanicolau
stain x400
Source: Authors' own work
Contrast soft tissue cervical, thoraco-abdominal and pelvic computed tomography reveals 8 mm left cervical lymph nodes, normal-sized kidneys with physiological secretion and excretion, no retroperitoneal lymph node enlargement and no discernable lung and liver pathological changes. The cervix presents a homogenous, iodophil image that is smaller than what was previously found at CT examination (Fig.4).
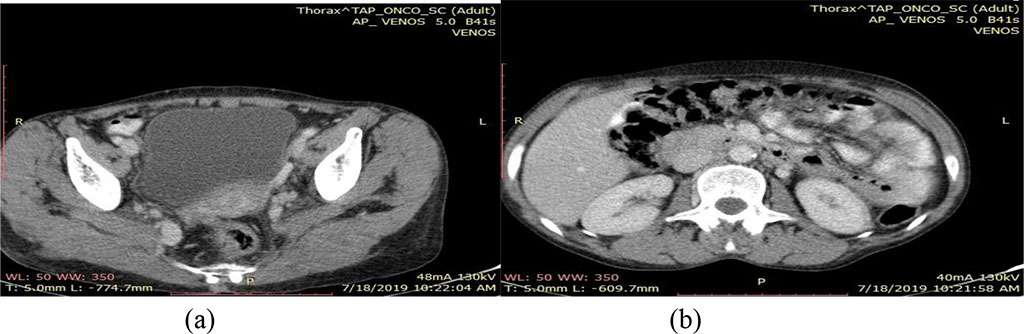
Fig.4. CT scan July 2019 - (a) Heterogeneous cervical image
and (b) normal sized kidney with physiological secretion and
excretion
Source: Authors' own work
The next post-therapy check-up is scheduled in three months. Post-therapeutic monitoring includes clinical examination and gynecological consultations once every 3 to 6 months in the first 2 years and 6 to 12 months in the third to the fifth-year post-treatment.
The International Federation of Gynecology and Obstetrics (FIGO) describes five stages of cervical cancer. Stage 0 and I are preclinical ones in which the diagnosis is made by cytology examination; stages II, III and IV are accompanied by clinical signs and are associated with malignant invasion (Bhatla et al., 2018; Denny et al., 2006; Peters III et al., 2000).
Concomitant radiotherapy and chemotherapy for patients with stage IB2 bulky – IV is the standard treatment recommended by the NCCN and ESMO guidelines. Clinical trials highlight the disease-free survival (DFS) and overall survival (OS) as being increased for concomitant radio-chemotherapy versus radiotherapy alone (Stryker & Mortel, 2000).
Results are contradictory concerning administering induction chemotherapy anterior to radiotherapy.
Life expectancy is correlated with the tumor stage at diagnosis, stage 0 having a 5-year survival rate of 100%, while stage IV reaching a ratio of only 7% (Bhatla et al., 2018).
Lymph node involvement is an important prognostic factor and has a huge impact in the subsequent therapeutic conduct (Creasman et al., 1987). In a report by Peters et al. 2020, enhanced survival is mentioned by the fact that patients with involved lymph nodes who underwent treatment with cisplatin concomitant with pelvic radiation, have had a far better response than those who benefitted only from RTE. For patients who were initially diagnosed with lymph node metastases, chemotherapy with platinum salts seems to have an effectively positive result (Stryker & Mortel, 2000), many studies continuing to report favorable results, contrary to the multiple severe acute hematological and gastrointestinal toxicities (Kazumoto et al., 2011; Kim et al., 2009; Kim et al., 2012; Small et al., 2007).
The most frequent lymph node groups involved in the metastatic process are obturator, hypogastric, iliac artery bifurcation and sacral lymph nodes. In 30% of cases the pelvic lymph nodes can be involved without the presence of parameter invasion, the survival rate being 71%.
In a study done by Shandong Cancer Hospital it was revealed that the most common site for pelvic lymph node metastasis are the obturators with a ratio of 17,6%, followed by external and internal iliac lymph nodes 13,4%, common iliac 3,6%, para-aortic 1,7% and presacral lymph nodes 0,6% (Li et al., 2015).
Cervical lymph nodes are the most frequent metastatic site for head and neck tumors. Cervical and supraclavicular lymph nodes are rarely found in current practice. Literature data report a ratio of secondary supraclavicular lymph node involvement of 0.1%–1.5%. Patients with involved supraclavicular lymph nodes treated with chemotherapy have a reported 3-year and 5-year survival rate of 16,5%.
However, occult supraclavicular lymph node metastases have been identified by FDG-PET in 8% of patients (14 of 186).
Supportive psychotherapy must focus on solutions, and in all medical cases, supportive groups may be efficient by sharing individual experiences, such as patient groups with the same diagnosis or patient groups with the same therapeutic sequence (Rebegea et al., 2019; Păduraru et al., 2019).
Although screening programs exist, cervical cancer is still diagnosed in advanced stages, although it benefits from double prevention, both through regular testing and through vaccination. The main aim of the treatment in the advanced stages of the disease is palliation and reaching a minimal toxicity and complication risk.
The peculiarity of the case resides in the distant metastasis to the cervical and supraclavicular lymph nodes, a rare finding during treatment that is associated with a poor prognosis.
In this case we notice the full remission of the secondary left cervical and supraclavicular lymph node involvement. Early diagnosis is the main factor which conditions the therapeutic results and chances for survival.
A big part of the current research is aimed at molecular detection of cervical cancer precursors; this should overcome many of the deficiencies associated with screening and cervical cytology programs.