- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2023. 13; 6: e1. DOI 10.35630/2023/13/6.609
Ocular manifestations in autoimmune diseases are mainly related to the formation of a chronic inflammatory process in the body. This is caused by an error in the body's histocompatibility system, which results in the lymphocyte attacking its own cells, which the lymphocyte considers foreign. Various autoimmune diseases with ocular symptoms may have different inflammation-related pathophysiology, ranging from increased vascular permeability in diabetic retinopathy to lymphocytic pressure in the exocrine glands in Sjögren's syndrome. The inflammatory process in the eye tissues leads to symptoms such as pain, redness, photosensitivity, tearing and reduced visual acuity. One of the most common autoimmune diseases associated with ocular symptoms is systemic lupus erythematosus, in which 50% of patients experience ocular symptoms. Ocular manifestations may worsen or improve depending on disease activity. Ophthalmological examination is extremely important for patients with autoimmune diseases because it allows for the early detection and treatment of eye-related diseases, monitoring the side effects of medications taken, and identifying other related health problems.
The aim of our work was to raise awareness of how many diseases can cause symptoms only in one organ, the eye. This shows how important examinations by an ophthalmologist and vigilance are.
Methods: We analyzed articles on Pubmed and specialized medical literature and selected the most common autoimmune diseases causing symptoms in the eye. Then we divided them into systems and described them in detail.
Conclusions: Autoimmune diseases are becoming more and more common in society. As the number of sick people increases, our awareness of the potential symptoms they may cause should increase. In our work, we show numerous diseases and their symptoms manifesting themselves in the eye. We focus especially on the most common autoimmune diseases and their impact on our eyesight. The symptoms are diverse and often very bothersome for sick people, which is why it is so important to be aware of their occurrence and diversity.
Keywords: autoimmune diseases, eye diseases, ocular symptoms, diabetic retinopathy, capillary permeability, lupus erythematosus, inflammation, pain, exocrine glands, visual acuity, people
Autoimmune diseases are a group of diseases in which the body's immune system attacks its own tissues and organs, leading to their destruction. This process is caused by excessive reactivity of the immune system and improper functioning of regulatory mechanisms. In autoimmune diseases, inflammation is the main factor leading to ocular symptoms. The inflammatory process in the eye tissues leads to symptoms such as pain, redness, photosensitivity, tearing and reduced visual acuity. A specific autoimmune disease affects various structures of the eye, such as the cornea, retina, iris or blood vessels, which results in specific symptoms for a given disease entity. It is important to understand that ocular symptoms in autoimmune diseases can vary and even vary from patient to patient. If any eye symptoms occur, it is always recommended to consult a doctor in order to initiate optimal therapy and prevent complications. Ocular manifestations are often among the first symptoms of an autoimmune disease. Unfortunately, despite the common occurrence of autoimmune diseases, common ophthalmological symptoms may be misdiagnosed. That is why a multi-level approach to the patient is so important. We should use interprofessional care of the patient. It is also worth bearing in mind that these diseases may occur in people with chronic underlying medical conditions, which may cause our vigilance to be obscured by other symptoms.
After carefully analyzing articles on Pubmed and specialized medical books, we selected the most common autoimmune diseases that cause ophthalmological symptoms. Then we divided them into systems and carefully described the eye ailments that occur in these diseases. Our goal was to present the issue and draw attention to how many serious autoimmune diseases can cause symptoms only in one organ, the eye.
Eye symptoms often become a component of systemic diseases. They may precede the manifestation of a full-blown disease and constitute its first symptom, occur during an exacerbation, or be a consequence of a long-term disease.
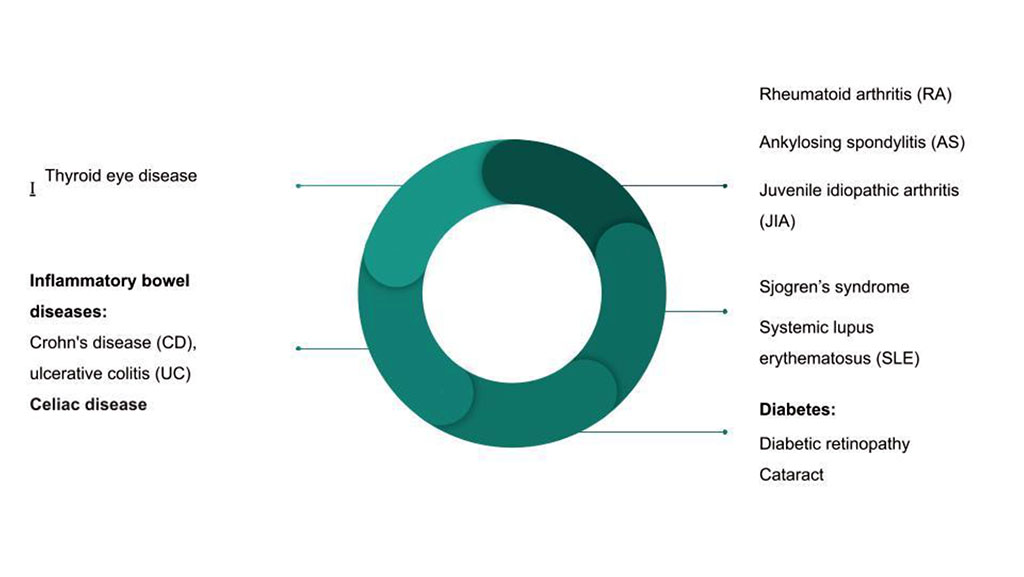
Figure 1. Autoimmune diseases causing eye symptoms
Type 1 diabetes:
It is an autoimmune disease in which anti-islet antibodies occur that destroy pancreatic beta cells and lead to a sharp drop in insulin levels, which requires lifelong insulin treatment. Ocular complications may occur in the course of this disease.
This complication may occur in both type 1 and type 2 diabetes. It can be diagnosed in almost all people with type 1 diabetes after 10 years of the disease. [7] This is a common cause of vision loss in these patients.
The pathophysiology of this disease involves increased capillary permeability and the formation of microaneurysms, which results in the development of intravascular thrombosis. This causes ischemia and stimulates the development of new vessels. They are susceptible to damage, which may cause bleeding. [30]
The most advanced stage of retinopathy is proliferative retinopathy, which is characterized by the growth of new vessels in the retina and vitreous body. These vessels can lead to traction on the retina and its detachment, which may result in irreversible vision loss. [7]
The risk factor for its occurrence is the duration of diabetes, unstable glycemia, and the development of improperly controlled arterial hypertension. [27]
The United Kingdom Prospective Diabetes Study conducted a study in which it was shown that proper glycemic control reduces the risk of retinopathy, but also other diabetes complications such as nephropathy or neuropathy, and the number of these microvascular complications was reduced by 25%. This study also showed that reducing the level of glycated hemoglobin by 1 percentage point results in a reduction in the risk of developing microvascular complications by up to 35%. [7]
Patients with type 1 diabetes have greater ischemic changes than those with type 2 diabetes, which is why the disease may progress more quickly. [27]
We treat this condition by performing photocoagulation of the vessels. This method allows you to delay the progression of this disease and limit vision loss, but this treatment will not restore the lost ability to see. That is why it is so important to regularly examine the fundus of the eye in patients with diabetes in order to start treatment as soon as possible. [7] Intravitreal anti-VEGF injections are also used. [9]
Regular examinations are also important because most patients do not experience symptoms when the process of vascular proliferation begins.
Retinopathy may also become more severe during pregnancy, so pregnant women must undergo check-ups at the beginning of pregnancy and in the 28th week. [21]
Cataracts will be more common in diabetic patients. This is due to the fact that metabolic disorders cause the lens to cloud more quickly. Research shows that the more severe the diabetes, the greater the risk of developing cataracts. [6] As in the case of retinopathy, proper glycemic control is most important.
Another name for this disease is dryness syndrome. It is a systemic connective tissue disease characterized by the formation of lymphocytic infiltrates in the exocrine glands, which impairs their function.
In this work, we will focus on ophthalmological problems, but it is worth remembering that this disease's spectrum of symptoms includes salivary secretion disorder, dry mouth syndrome and many systemic symptoms.
Eye complaints result from impaired tear secretion, which causes a feeling of sand under the eyes, photophobia, conjunctival hyperemia, and hypersensitivity to wind and tobacco smoke. [12]
We diagnose this using the Schrimer test, which is used to assess tear secretion.
The basis of treatment is artificial tears, soft lenses and the use of viscosity-increasing ointments at night. [1,2]
Systemic lupus erythematosus (SLE) belongs to the group of autoimmune diseases resulting from disorders of the immune system leading to autoimmunity. This results in the development of a chronic inflammatory process in many tissues and organs in the body. In 50% of cases, there is an ocular manifestation with symptoms of inflammation of the optic nerve, retina, cornea or dry eye syndrome. Pathological changes are most often the result of the deposition of immune complexes in the vessels of the eyeball, leading to vasculitis and embolism due to the cytotoxicity of autoantibodies characteristic of SLE, such as APLA and ANA. [31] SLE patients most often visit an ophthalmologist due to sudden deterioration of vision, eye pain or a feeling of sand under the eyelid. It often happens that an ophthalmologist discovers the first disturbing symptoms that may suggest SLE during a routine visit.[13]
The most common ophthalmological symptom in SLE is dry conjunctivitis and keratitis, known in medical nomenclature as dry eye syndrome. More than 25% of patients show abnormalities on the Schirmer test, and 12% qualify for a diagnosis of secondary Sjogren's syndrome.[16] Retinal symptoms that can be observed during fundus examination include cotton wool foci resulting from microcirculation disorders. Inflammation of retinal arterioles, which leads to ischemia and, consequently, retinal neovascularization, may cause vitreous hemorrhage. Other retinal manifestations include microaneurysms, retinal edema, retinal exudates, and multifocal serous retinal detachment or pigment epithelial detachment.[31] SLE involves hypertension and nephritis, which can also cause retinal changes such as arteriolar narrowing, retinal hemorrhages, and optic disc edema.[13] Retinal vasculitis and neovascularization should suggest a risk of central nervous system involvement and occult cerebral vasculitis. SLE-related retinal microangiopathy results from immune complex-mediated vascular damage. [16]
Retinopathy in SLE occurs in approximately 10% of patients. Antiphospholipid antibodies and anti-beta-2 glycoprotein-I are considered crucial in the pathogenesis of this disease. Mild retinopathy may be asymptomatic and transient, but severe form is characterized by deterioration of vision, image distortions or visual field limitations.[16,4] Optic neuritis in SLE is caused by chronic ischemia, which may lead to subsequent demyelination and progressive loss of vision. Optic nerve involvement occurs in approximately 1% of SLE patients. The corneal symptoms most frequently reported by patients in SLE include eye pain, redness, tearing, photophobia, or a foreign body sensation under the eyelids. Corneal physiology disorders are a sensitive marker of inflammation throughout the body. The diagnosis of peripheral ulcerative keratitis correlates with active vascular inflammation. The cause of the disease is the activation of the complement system by immune complexes, causing chemotaxis of inflammatory cells and the release of collagenases. This mechanism leads to the destruction of the corneal stroma. The symptom of peripheral ulcerative keratitis is a characteristic crescent-shaped lesion visible in the corneal stroma, which may lead to perforation.[16]
A common ocular manifestation of SLE is corneal edema. Cytokine release in the corneal basement membrane induces peripheral inflammation on the corneal surface.[4] SLE can also lead to involvement of the cranial nerves and cause diplopia. Eye movement abnormalities are common in SLE and have been observed in up to one fifth of patients as a result of ischemic brainstem microvascular disease. Paralysis of the third and sixth cranial nerves is the most common disorder in SLE patients.[13,16]
Rheumatoid arthritis (RA) is a systemic autoimmune disease that typically affects the joints of the hands, knees, wrists, and feet. Extra-articular manifestations of RA are described in various organs, including the lungs, kidneys, circulatory system, and eyes.
Ocular symptoms in rheumatoid arthritis appear in approximately 18% of patients, mainly involving the anterior segment of the eye. Anterior segment eye diseases in RA include dry eye syndrome, peripheral ulcerative keratitis, episcleritis, and anterior uveitis. The most commonly described ocular manifestation of rheumatoid arthritis is dry eye syndrome. [20]
Dry eye syndrome occurs in RA with a frequency of up to 25%. [10] This condition affects the eye's surface and tear production, leading to discomfort, visual disturbances, instability of the tear film with potential eye surface damage, increased tear osmolality, and ocular surface inflammation. Symptoms include itching, burning, foreign body sensation, light sensitivity, and redness.[20]
Peripheral ulcerative keratitis is characterized by peripheral corneal thinning due to autoimmune disturbances. Patients present to the doctor with gradual vision loss secondary to corneal melting. As the disease progresses, it leads to corneal distortion and, less commonly, perforation.[20]
Episcleritis is characterized by a sudden onset, discomfort with minimal impact on visual acuity. The attack lasts from 1 to 2 weeks and resolves spontaneously, but it may recur over the years. Approximately 5.6% of patients with episcleritis have RA. [20]
Symptoms of scleritis include deep eye pain, photophobia, tearing, and eye redness. The pain is localized in the extraocular area and may radiate to the forehead and temple. RA-associated scleritis is associated with a worse prognosis compared to episcleritis. In inactive disease, the sclera shows a blue tint, indicating scleral thinning. About 50% of patients with nodular scleritis have signs of scleral thinning. [10,20]
Ankylosing spondylitis is the most common form of seronegative spondyloarthritis, primarily affecting the sacroiliac joint, spine, and tendon attachments. [5]
The most common extra-articular symptom in patients with ankylosing spondylitis is acute anterior uveitis. The prevalence of this condition in patients with ankylosing spondylitis is 40%, and it occurs more frequently in men.[20] HLA-B27-positive patients experience it more frequently and have a worse prognosis. [5]
Acute anterior uveitis has a sudden or insidious onset, with an acute, recurrent, or chronic course. Compared to posterior uveitis, anterior uveitis less commonly leads to blindness. Symptoms include redness, pain, photophobia, and blurred vision. Usually, only one eye is involved at a given time. It is often confused with conjunctivitis. In patients with ankylosing spondylitis, relapses are frequent. [19]
Recurrent episodes of anterior uveitis can lead to cataract development. Typically, it is a posterior subcapsular cataract. [20]
Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in children, occurring before the age of 16 and lasting at least 6 weeks. The most common extra-articular manifestation of this disease is uveitis, with chronic anterior uveitis being the most common form, often asymptomatic. [26]
Uveitis can precede the onset of joint symptoms in juvenile idiopathic arthritis. Risk factors for chronic anterior uveitis include young age, female gender, degenerative disease, and the presence of ANA.[25] Research suggests a two-phase course of the disease, with a second peak occurring during adolescence.[11]
The risk of developing cataracts in patients with chronic anterior uveitis associated with juvenile idiopathic arthritis has been studied by Thorne and colleagues. Risk factors assessed include the presence of posterior synechiae, active uveitis, and local corticosteroid use.[28]
Ocular manifestations of thyroid disease cover a wide range of symptoms from ocular discomfort and irritation, lid retraction, chemosis, proptosis and restriction of ocular motility, to corneal exposure, eyeball protrusion and optic nerve compression leading to blindness. [22]
However, the most common diagnosis is thyroid eye disease (TED), which is an autoimmune inflammatory disease of the eyeball and its surroundings. Another name is ophthalmopathy or Graves' orbitopathy or thyroid orbitopathy. It is the most common cause of manifestations of eye diseases of the thyroid gland and proptosis in both sexes, with a higher incidence among women. [15] Exophthalmos is the most common symptom of TED - it occurs in 20–30% of patients treated for Graves' disease and in 40–70% of patients with ophthalmopathy related to thyroid damage. [24]
Typically, TED is observed in association with hyperthyroidism and pretibial myxedema, but recent studies report that ocular symptoms also appear in patients with Hashimoto's thyroiditis, as well as in the absence of confirmed dysfunction of this organ.
Clinically, orbital and periorbital edema, eyelid retraction, eyelid lag in downgaze, restrictive
strabismus, compressive optic neuropathy, and exposure keratopathy with common symptoms of ocular irritation and dryness are observed.
Symptoms may occur both unilaterally and bilaterally. It has been shown that low selenium levels, high exposure to stress and smoking increase the frequency of disease exacerbations and worsen its course. [15]
Inflammatory bowel diseases (IBD) are a group of chronic gastrointestinal diseases characterized by periods of exacerbations and remissions. Crohn's disease (CD) and ulcerative colitis (UC) are the 2 main disease entities of IBD. The incidence of CD and UC in Europe is estimated at 505/10,000 and 322/100,000, respectively. The pathogenesis of IBD is complex and multifactorial. Currently, it is believed that genetic factors, especially the NOD2 gene on chromosome 16, environmental and immunological factors influence the manifestation of the disease. The latter are responsible for the dysregulation of the normal immune response, as well as the increase in the production of tumor necrosis factor TNF and gamma interferon. The clinical picture of CD and UC differs due to the pathophysiology of both diseases. [14]
The main symptoms are gastrointestinal, but extraintestinal symptoms are common and occur in 9% to 40% of patients. Ocular manifestations constitute the third, after rheumatological and dermatological, extraintestinal symptoms of CD and UC. [3] Eyeball involvement is observed in 12-35% of patients with ulcerative colitis and 25-70% of patients treated for Crohn's disease. [14]
The first report on ocular manifestations in IBD was published by Crohn in 1925 and mentioned patients who were likely to have keratomalacia and xerophthalmia. [29]
Eyeball involvement is usually primary and manifests itself during an exacerbation of the underlying disease, and the scope of pathology includes both asymptomatic cases and those resulting in blindness. In some patients, ocular symptoms precede gastrointestinal symptoms. [14]
Primary symptoms:
Episcleritis and anterior uveitis have been reported in patients with both Crohn's disease and ulcerative colitis. However, scleritis, conjunctivitis and dry eye syndrome are observed primarily in patients with CD. [14]
Episcleritis
Episcleritis is the most common manifestation of ocular symptoms associated with IBD. The inflammatory process involves the episcleral vessels located in Tenon's capsule. Symptoms include mild or moderate pain in the eyeball, tearing with or without photophobia, and discomfort. On physical examination, the inflammation manifests as limited or, less often, diffuse redness of the episclera, which fades after local application of a vasoconstrictor. Visual acuity and pupillary reaction to light are preserved. The cornea is not affected. Inflammation is self-limiting, it is necessary to stabilize the underlying disease. In order to reduce pain and discomfort, it is recommended to use cold compresses. [23] In severe or recurrent cases, NSAID therapy may be considered, with cyclooxygenase-2 being preferred. Constant monitoring by a gastroenterologist is then necessary due to the risk of triggering a relapse of the underlying disease. In resistant cases, infliximab may be considered. [14,23]
Scleritis
Scleritis occurs in less than 1% of IBD patients. Unlike episcleritis, it can develop during a period of remission. The hyperemia present during physical examination does not fade under the influence of local decongestants due to the inflammation of the deep vessels of the sclera. The clinical picture includes severe retrobulbar pain, radiating to the temporal area, jaw and forehead, without photophobia. Visual acuity is not impaired. Therapy involves the use of systemic steroids or immunosuppression. [23] Lack of effective therapy may lead to retinal detachment or optic neuritis. [14]
Uveitis
Uveitis can be divided according to the structures involved. If the anterior chamber is affected - inflammation of the iris and ciliary body - we talk about inflammation of the anterior uvea. Indirect occurs when the inflammation affects the vitreous body and the retina affects the posterior section of the uvea. The inflammatory process may affect all sections of the uvea, which is called panuveitis.
Anterior uveitis mainly affects patients undergoing treatment for Crohn's disease. The physical examination describes photophobia, pain, redness, tearing and decreased visual acuity. Physical examination reveals ciliary hyperemia, perikeratic hyperemia, miosis, and anterior chamber effusion (Tyndall's sign). Slit lamp examination may sometimes show corneal precipitation and posterior adhesions.
Therapy includes the use of topical corticosteroids combined with topical cycloplegic medications. In severe or refractory cases, periocular or systemic injection or anti-TNF drugs may be considered. [14,23]
Depending on the primary outbreak, its severity and duration, it may be complicated, by cataracts, glaucoma, band keratopathy, vitreous hemorrhage, cystoid macular edema, retinal detachment, retinal ischemia, optic atrophy, chronic eye pain and blindness.
Keratopathy
It covers the area associated with active scleritis ranging from mild to severe. The clinical picture includes peripheral ulcerative keratitis (PUK), stromal keratitis and peripheral corneal thinning.
PUK is a form of keratitis associated with the active phase of IBD and threatening vision loss. Physical examination reveals unilateral or bilateral corneal ulceration with epithelial loss, stromal thinning and limbal inflammation, as well as limited or diffuse scleritis. The therapy uses infliximab. [23]
Other
Infiltrates and scars that may cover every layer of the cornea - both the epithelium, stroma and endothelium. The location of lesions outside the visual axis does not worsen visual acuity.
All patients with inflammatory bowel disease showed a tendency towards thinner corneal thickness, while decreased tear secretion was more frequently observed in patients with Crohn's disease.
The immunosuppressive therapy and anti-inflammatory drugs such as 5-aminosalicylic acid may worsen the symptoms of dry eye syndrome.
Salzmann's nodules revealed by the replacement of Bowman's layer with eosinophilic material are also considered an ocular manifestation of Crohn's disease.
It should be remembered that IBD is a relative contraindication to laser refractive surgery, and among CD patients in remission and during LASIK and PRK therapy, necrotizing keratitis requiring intensive steroid therapy has been observed. [23]
Ocular symptoms associated with IBD also include perforating scleromalacia, orbital inflammatory disease, occlusions of the central retinal artery and its branches, central retinal vein occlusion, retinal vasculitis, and optic neuritis.
Secondary ocular involvement is related to pharmacotherapy used to control and treat the underlying disease, in particular during glucocorticoid therapy (GCS). For this reason, every patient using glucocorticoids should be routinely checked by an ophthalmologist due to the risk of cataracts and glaucoma. [14]
Appropriate cooperation between an ophthalmologist and a gastroenterologist, quick diagnosis and appropriate therapy will help avoid irreversible consequences of ocular involvement and loss of vision. [14,23]
Celiac disease belongs to the group of autoimmune diseases and occurs in genetically predisposed people (HLA DQ2/8 gene). The disease may be overt (symptomatic) or hidden. The classic form is limited to gastrointestinal disorders with diarrhea and weight loss, associated with crypt hypertrophy and intestinal villi atrophy and a positive serological test result. The atypical form occurs without symptoms from the digestive system or with scant changes in the intestinal mucosa, but with a positive serological test and the presence of extraintestinal symptoms. Ocular manifestations of celiac disease are rare, but the possibility that they may be the first symptom of a systemic disease should be taken into account. The clinical picture may then include orbital myositis, uveitis, thyroiditis associated with orbitopathy, nyctalopia (night blindness), dry eye syndrome, cataract, central retinal vein occlusion, and neuro-ophthalmological symptoms. Moreover, ophthalmological symptoms can be divided into those related to malabsorption disorders and those resulting from immunological disorders. [17,8]
Symptoms resulting from malabsorption disorders include:
Retinopathy
The clinical picture consists of characteristic yellow-white punctate changes in the peripheral part of the retina and changes visible in the electroretinogram (ERG). Patients often suffer from vitamin A deficiency, the normalization of which leads to improvement of the clinical condition. [17]
Dry eye syndrome
The main cause of dry eye syndrome in people with celiac disease is vitamin A deficiency. Physical examination may reveal Bitot's spots resulting from keratinization of the periapical conjunctiva. In more severe cases, liquefying corneal necrosis (keratomalacia) may occur. Retinoic acid 0.1% is used topically in therapy. [17]
Cataracts
Chronic diarrhea leading to dehydration, vitamin D deficiency and hypocalcemia are the probable causes of cataracts. This is due to the fact that a low level of calcium in the aqueous humor changes the permeability of the lens epithelium, disturbing the osmotic balance and thus leading to clouding of the lens. [17]
Pseudotumor of the brain
Idiopathic intracranial hypertension associated with poisoning or, rarely, vitamin A deficiency. Clinically, it is manifested by swelling of the papillae of the optic nerve (oedema papillae nervi optici- papilledema) in the presence of normal radiological findings and the absence of any other possible cause of increased intracranial pressure. [17]
The symptoms resulting from an immune defect include:
Inflammation of the orbital muscles:
The pathophysiological basis is considered to be eosinophilic and granulomatous infiltration and the presence of anti-gliadin antibodies. The clinical picture includes diplopia, pain with eye movements and proptosis. It responds well to steroid therapy. [17]
Uveitis, thyroiditis with orbitopathy and
Occipital calcification of the brain:
Local inflammatory foci and vasculitis result in neuro-ophthalmological changes as a result of defective immune mechanisms. [17]
The ocular manifestations of celiac disease are not different from the ocular manifestations of other inflammatory bowel diseases. [18]
Table 1. Basic ophthalmological symptoms present in autoimmune diseases
| Autoimmune disease | Eye symptoms |
| Diabetes |
|
| Sjogren's syndrome |
|
| Systemic lupus erythematosus (SLE) |
|
| Rheumatoid arthritis (RA) |
|
| Ankylosing spondylitis (AS) |
|
| Juvenile idiopathic arthritis (JIA) |
|
| Thyroid eye disease |
|
| Inflammatory bowel diseases (IBD) |
|
| Celiac disease |
|
An ophthalmological examination allows for early detection of eye symptoms related to autoimmune diseases. Many patients may not realize that their visual disturbances are related to an autoimmune disease. Early diagnosis and treatment are key to avoiding complications and minimizing the risk of vision damage. Ocular symptoms may worsen or improve depending on disease activity.
Patients with autoimmune diseases require comprehensive health care, and the team of specialists should include an ophthalmologist.