- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2023. 13; 6: e1. DOI 10.35630/2023/13/6.606
The authors presented a clinical case of left subclavian steal syndrome in a 62-year-old man. The main complaints were dizziness, tinnitus, memory loss and unsteady gait. The patient had severe concomitant pathology: coronary heart disease, hypertension, heart failure. X-ray endovascular technologies (balloon dilatation and stenting) made it possible to completely restore blood flow in the affected segment. After treatment, the above complaints disappeared. Minimally invasive X-ray endovascular techniques have particular benefits in patients with severe comorbid pathology.
Keywords: vertebral-subclavian steal syndrome, steal syndrome, vertebral artery, atherosclerosis, angiography, vascular stenting
Subclavian steal syndrome, first reported by Contorni L., is a phenomenon involving reversed blood flow in a branch of the subclavian artery, which occurs as a result of hemodynamically significant ipsilateral occlusion or severe stenosis of the proximal subclavian artery [1]. In this condition, called subclavian steal syndrome by Fisher, blood is pumped from the contralateral vertebral artery to the opposite vertebral artery, thereby blood is “stolen” from the main artery [2-4].
The incidence of subclavian steal syndrome in the UK population is about 1.3%, and is more common among men than among women. Among people with neurological symptoms undergoing Doppler examination of the vessels of the head and neck, the frequency of this pathology is approximately 17% [5-7].
Most patients are asymptomatic, but patients with coronary artery bypass graft may suffer from angina (associated with load on the upper extremity ipsilateral to the graft) and stenosis (so-called “coronary-subclavian steal”). Subclavian steal may also manifest as vertebrobasilar insufficiency or, most commonly, arm claudication [8-12].
Careful examination of segmental pulsatility and pressure, as well as the use of duplex ultrasonography, magnetic resonance angiography, computed tomography, or conventional angiography, can confirm the presence of subclavian stenosis. Subclavian artery stenosis, regardless of symptoms, is a marker of atherosclerotic disease and an increased risk of cardiovascular and cerebrovascular events [13].
Previously, percutaneous angioplasty with a balloon catheter was used to relieve stenosis of the subclavian artery. Due to the limitations of this technique, it is currently replaced by stent implantation which is commonly used to treat subclavian stenosis [14-16]. In this study, we report a case of subclavian steal syndrome that was diagnosed and successfully treated using newly developed diagnostic tools and medical devices.
Patient M., 62 years old, was admitted to the clinic with a following diagnosis: ICD-10 code: I65 Atherosclerosis. Occlusion of the right internal carotid artery. Hemodynamically significant stenosis of the left subclavian artery. Steal syndrome on the left.
Concomitant diseases: ICD-10 code: I11.9 IHD. Class 1 heart failure. Hypertension stage 2. Risk of cardiovascular complications 3 stage 1.
Patient was admitted with complaints of periodic dizziness, tinnitus, gradual memory loss over the last year, and unsteady gait.
Medical history: The above complaints have been bothering him for the past few years. Gradually, the episodes of dizziness intensified, and headaches became more frequent. He took a consultation with a vascular surgeon, got an additional examination. It revealed hemodynamically significant stenosis of the left subclavian artery. He was recommended scheduled hospitalization for further examination and determination of further treatment tactics.
Objective status: Skin color: normal, clean. Skin turgor: normal. State of the oral cavity and pharynx: moist mucosa, normal color.
Conjunctiva: normal color, moist. Peripheral lymph nodes: not enlarged. Heart rate: 78 beats per minute. Respiratory rate: 18 breaths per minute. Breathing: vesicular, active on both sides. No rales in the lungs. Tongue: wet.
The abdomen of the correct shape, not bloated, symmetrical; evenly engaged in breathing. Dimensions: not enlarged. Lumbar region: unchanged. Diuresis and stool: normal.
Data from instrumental studies: EGD - focal atrophy of the antral gastric mucosa. Duodenogastric reflux.
Doppler ultrasound of the lower limb veins: preserved patency of the deep and saphenous veins of both lower limbs.
Echo: Dilatation of the right atrium. Left ventricular myocardial hypertrophy. Preserved valvular function. Increased echogenicity of the myocardium, heterogeneous structure. Grade I diastolic dysfunction. Preserved systolic function.
CT angiography of brachiocephalic vessels: CT picture of atherosclerosis of brachiocephalic arteries:
Surgery: Balloon angioplasty and stenting of the left subclavian artery. Surgery record: local anesthesia using Sol. Lidocaini 2% - 2.0 ml. The left radial artery was punctured and catheterized. A 6F introducer was installed. Selective angiography of the brachial and subclavian arteries on the left (where occlusion of the proximal segment of the subclavian artery on the left was detected). Recanalization of the subclavian artery was performed with a 0.35 conductor with the support of a guiding catheter; the conductor was inserted into the descending aorta. Next, an Armada 0.35 8.0x6.0 mm balloon catheter was inserted through a 0.35 hydrophilic guidewire, and predilation of the occlusion zone was performed with a pressure of 6 atm. Next, a 10.0x60 mm Absolute Pro self-expanding stent was delivered, positioned, and implanted using a 0.35 guidewire. Control arteriography of the left radial artery revealed no signs of malposition, proximal or distal dissection. Pressure bandage was applied. The duration of the surgery was 60 minutes.
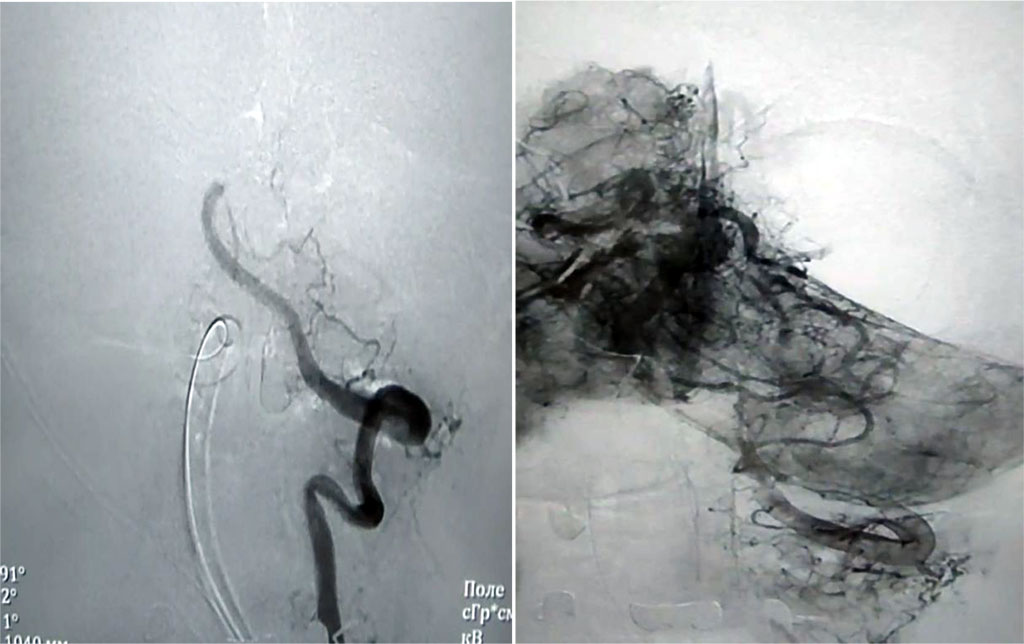
Figure 1. Angiography of the cranial vessels before surgery
Conservative treatment: antiplatelet therapy, antihypertensive, infusion, gastroprotective, antispasmodic therapy.

Figure 2. Angiography of the cranial vessels after balloon dilatation and stenting
After treatment, the patient showed positive dynamics due to regression of the above symptoms and an increase in the distance of pain-free walking. He did not require further inpatient treatment in the cardiovascular department. The patient was discharged from the department in satisfactory condition with follow-up care by a surgeon at the local clinic.
Thus, this clinical case shows the effectiveness of X-ray endovascular surgery for critical stenosis of the carotid arteries. In addition, minimally invasive techniques have a particular advantage in patients with severe concomitant pathology.