- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2023. 13; 6: e1. DOI 10.35630/2023/13/6.605
Purpose of the Study: In this article, the team of authors shares their own experience of performing the procedure of therapeutic angiogenesis with plasmid DNA in the department of surgery.
Materials and Methods: From November 2020 to December 2021, the department performed 64 procedures of therapeutic angiogenesis using plasmid DNA in 32 patients with distal steno-occlusive lesions of lower limb arteries, with CAI II-A - CAI III according to Pokrovsky-Fontaine. All patients included in the statistics of this work were questionnaired (SF-36) and thoroughly interviewed during the writing of this article.
Results: Of the 32 patients, only two (6.25%) noted a deterioration in their condition, of which one patient with CAI III and diabetes underwent hip amputation after 1.5 months. In the second patient, three months after the repeated procedure of therapeutic angiogenesis, the distance of pain-free walking decreased from 350 to 250 meters, which can be associated with severe nicotine addiction and inability to quit smoking. Four patients did not note any significant changes in their condition in the period from 2.5 to 6 months after repeated administration of the drug. 12 patients (37.5%) noted moderate positive changes in the form of an increase in pain-free walking distance, a decrease in pain, and an improvement in quality of life. 14 patients (43.75%) claimed a significant increase in pain-free walking distance and assessed the results of the therapy as good. The greatest positive dynamics were observed in the groups CAI II-A and CAI II-B. The peak of positive dynamics of pain-free walking distance was noted 3-6 months after the second administration of the drug.
Conclusion: As a result of treatment with plasmid DNA, we noted a significant positive effect from the procedure, especially in patients with intermittent claudication. In a group of patients with critical ischemia, the procedure of therapeutic angiogenesis became the only means to preserve the limb.
Keywords: chronic arterial insufficiency, therapeutic angiogenesis, plasmid deoxyribonucleic acid
Obliterating arteriosclerosis of lower limb arteries is one of the most common diseases of the cardiovascular system, and in terms of mortality and disability of the population it competes equally with coronary heart disease and lesions of the arteries of the neck and brain. [1-6] The disease is associated with the formation of cholesterol plaques in the lumen of the arteries, narrowing of the lumen of the latter with the development of ischemic syndrome of the lower limbs. Atheromatous damage to the arteries has a polyetiological genesis: dysmetabolic conditions, a response to damage, etc. The main risk factors for the development of this disease include smoking, elevated cholesterol and blood sugar levels. Based on the localization of the process, the aortoiliac, femoral-popliteal and tibial segments are distinguished. To classify ischemia of the lower limbs, we used the Fontaine-Pokrovsky classification of chronic arterial insufficiency [7-10].
Despite the fact that chronic ischemia of the lower limbs remains a surgical issue, in practice, vascular surgeons often encounter non-shuntable cases. This type of patients includes patients with distal lesions of the arterial bed, when reconstructive interventions are impossible. For the treatment of patients with similar damage to the arteries of the lower limbs, therapeutic methods of treatment remain relevant, especially modern methods of cell therapy, growth factor therapy, pharmacotherapy and physiotherapeutic techniques. [11-14]
Thanks to the rapid development of pharmacology and molecular biology in recent years, the range of treatments for non-shuntable patients has increased, including the use of red bone marrow stem cells, mesenchymal stromal cells and many others. In our clinic, over the last year and a half, we have begun to actively use the method of therapeutic angiogenesis using plasmid deoxyribonucleic acid [supercoiled annular double-stranded] for patients with tibial artery lesions.
It is worth noting that plasmid DNA is the first gene therapy drug for therapeutic angiogenesis registered in Europe, the effectiveness of which has been confirmed by many studies [15-19]. Since 2013, the drug has been included in the National Recommendations and is recommended for use in patients with lower limb ischemia. The drug contains a highly purified supercoiled form of the VEGF165 plasmid, encoding the formation of vascular endothelial growth factor (VEGF).VEGF is the most active angiogenic factor, acting at many stages of angiogenesis, and VEGF165 is the most active isoform of the cytokine and has great mitogenic potential for endothelial cells, participates in the process of migration and proliferation of endothelial cells and prevents apoptosis of circulating endothelial cell precursors. [20-24]
The purpose of the study was to analyze the results of using the plasmid DNA drug in patients with chronic arterial insufficiency in the surgical department.
From November 2020 to December 2021, 32 patients with non-reconstructible lesions of the arterial bed of the lower limbs underwent the procedure of therapeutic angiogenesis in the surgical department. There were 23 men (71.85%) and 9 women (28.15%). The age of the patients was 69.5±8.9. The degree of lower limb ischemia is reflected in Table 1.
Table 1. Distribution of patients by degree of ischemia
| Degree of ischemia according to Fontaine-Pokrovsky | CAI II-А | CAI II-B | CAI III |
| Number of patients | 11 (34,375%) | 15 (46,875%) | 6 (18,75%) |
Before each procedure, all patients underwent a standard pre-hospitalization examination: general blood and urine tests, blood glucose levels, coagulogram, lipidogram, ECG, chest x-ray and some others; the condition of the vascular bed was assessed using duplex ultrasound mapping of the lower limb arteries with "Hitachi Arietta V70" device.
The procedure of therapeutic angiogenesis was carried out according to a standard method: 1.2 mg of plasmid DNA was diluted in 5-10 ml of physiological solution and a series of injections were performed into the muscles of the lower leg in the projection of the tibial arteries. The procedure was repeated after 2 weeks. During therapeutic angiogenesis, all patients took standard therapy with statins and aspirin. 29 patients (90.625%) had concomitant diseases, 26 (81.25%) suffered from coronary heart disease and hypertension, 7 patients (21.875%) had a history of diabetes mellitus, 6 patients (18.75%) were obese. 16 patients (50%) were smokers at the time of the primary procedure; they were strongly recommended to quit smoking. Treatment of concomitant pathology was carried out under the supervision of relevant specialists.
As of this writing, all patients have completed the SF-36 questionnaire and been thoroughly interviewed. Mann-Whitney U-test was used as non-parametric statistical criterion, on the basis of which p-value was calculated. Values at r≤0,05 were considered reliable.
Of the 32 patients, only two (6.25%) noted a deterioration in their condition, of which one patient with CAI III and diabetes underwent hip amputation 1.5 months after the repeated administration of plasmid DNA due to the progression of diabetic complications. In the second patient, three months after the repeated procedure of therapeutic angiogenesis, the distance of pain-free walking decreased from 350 to 250 meters, which can be associated with severe nicotine addiction and inability to quit smoking. Four patients did not note any significant changes in their condition in the period from 2.5 to 6 months after repeated administration of the drug. 12 patients (37.5%) noted moderate positive changes in the form of an increase in pain-free walking distance, a decrease in pain, and an improvement in quality of life. 14 patients (43.75%) claimed a significant increase in pain-free walking distance and assessed the results of the therapy as good. These results are reflected in Table 2.
Table 2. Pain-free walking distance in patients undergoing therapeutic angiogenesis
| Pain-free walking distance | Decreased | No change | Increased (from 100 to 300 meters) | Significantly increased (from 150-300 to 700-900 meters) |
| Number of patients | 2 (6,25%) | 4 (12,5%) | 12 (37,5%) | 14 (43,75%) |
The greatest positive dynamics were observed in the groups CAI II-A and CAI II-B. The peak of positive dynamics of pain-free walking distance was noted 3-6 months after the second administration of the drug. Fig. 1.
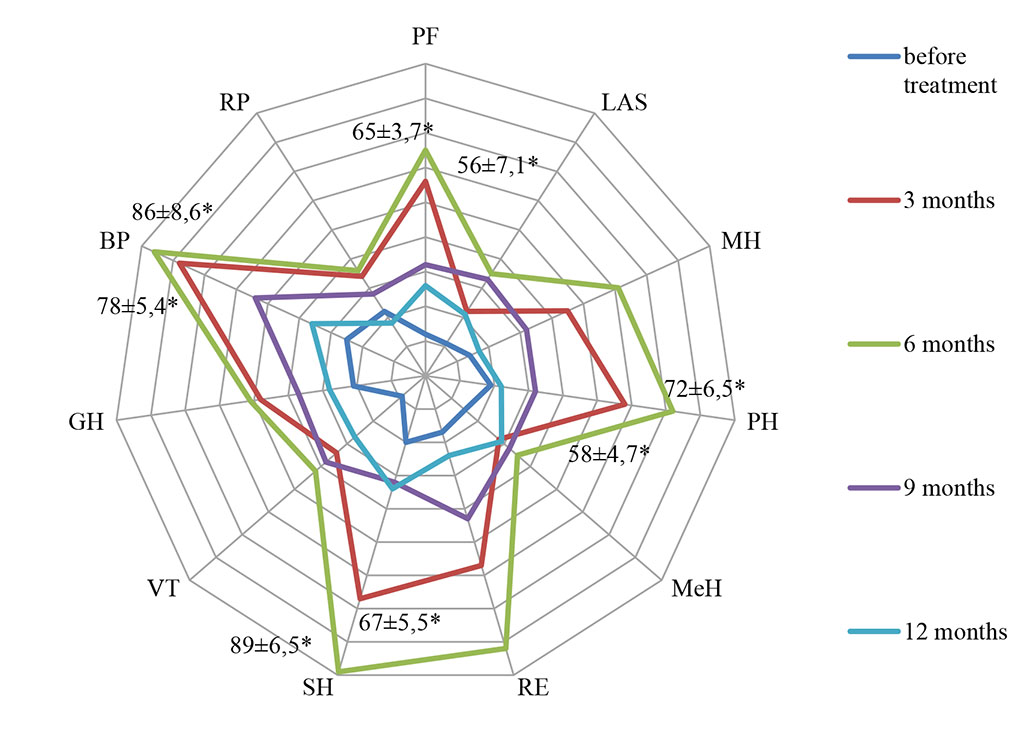
Figure 1. Indicators of quality of life of patients (SF-36 scale) during treatment (* – values at p≤0,05)
Less pronounced changes were observed in patients with diabetes and active smokers. In five out of six patients from the group with CAI III, the phenomena of critical ischemia regressed, and the affected limb was preserved. Two patients with neuroischemic diabetes mellitus noted a regression of neurological symptoms. One of these patients noted an improvement in the sensitivity of the skin of the foot and a decrease in numbness. The second patient noted a significant decrease in burning sensation in the sole area characteristic of polyneuropathic complications of diabetes. Most of the patients from the groups with increased pain-free walking distance also noted warming of the skin of the legs and feet. We did not observe any significant complications of the injections. Mortality from the procedure was 0.
It is also worth noting that the team of authors often takes an active surgical position in their daily professional activities. However, the method of therapeutic angiogenesis with plasmid DNA in patients with inoperable lesions of the arterial bed of the lower limbs allowed us to effectively help these patients without radical surgery.