- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2023. 13; 6: e1. DOI 10.35630/2023/13/6.604
The purpose of this prospective single-center study was to determine the feasibility of minilaparotomy for aortoiliac segment and its effect on intraoperative and postoperative outcomes.
Materials and Methods: From August 2020 to July 2022, the authors used minilaparotomy in 24 patients with aortoiliac atherosclerotic occlusive disease. The comparison group included 27 patients undergoing laparotomy. The age of the patients ranged from 58 to 83 years, among them 37 men and 14 women. In the group with traditional access, 9 aorto-bifurcational and 18 linear operations were performed; in the minimal incision group, there were 7 bifurcational and 17 linear interventions.
Results and Discussion: The duration of surgery was 196.5±26.7 minutes for operations with traditional access, and 146.3±16.7 minutes in the group with minimal incision. On average, minimal incision surgeries were shorter by 52.3±14.4 minutes (p≤0.05). For patients from the group with minimal incision, the length of stay in intensive care was 1.27±0.4 days, and with traditional access 2.3±0.3 (p≤0.05). Postoperative bed stay for the group with mini-access was 6.4±0.5 days, for patients with classic access 9.2±1.2 days (p≤0.05). 4 patients in the comparison group had postoperative paresis, and in one of them it was complicated by eventration. In the long-term postoperative period, two patients in the comparison group required surgery for an incisional hernia.
Conclusions: Minimal incision access to the aorta can reduce surgical trauma and intervention time, shorten the patient’s stay in the intensive care unit and postoperative bed, and minimize perioperative and postoperative complications. During repeated reconstructive interventions on the aorta, a “high” mini-access to the aorta allows to quickly reach the optimal area of the aorta for anastomosis and minimize organ trauma, as well as prevent adhesions in the abdominal cavity.
Keywords: aorta, abdominal surgery; arterial occlusive diseases/surgery; femoral artery/surgery; iliac artery/surgery; laparoscopy/methods; minilaparotomy/methods; vascular surgical procedures/methods; surgical procedures, minimally invasive/method
Lower extremity obliterating atherosclerosis is one of the most common and severe nosologies in vascular surgery, often leading to disability of the working-age population, and sometimes resulting in death [1,2]. Despite the intensive development of pharmacology and cellular technologies at the present stage, the treatment of arterial lesions of the lower extremities remains mainly a surgical problem [3-8].
Steno-occlusive lesions of the aortoiliac segment represent the most difficult problem for vascular surgeons, requiring large and traumatic operations, especially with bifemoral lesions [9-13]. A separate problem is posed by repeated bypass operations, when the surgeon should find shuntable “sites” above and below previous anastomoses, which in turn leads to larger incision, increased trauma and a high risk of postoperative complications. For a long time, total laparotomy from the xiphoid process of the sternum to the pubic symphysis was considered universal access to the infrarenal aorta. This incision is convenient for the surgeon and allows full access to the infrarenal aorta and iliac vessels, but it increases the time of surgery and the rehabilitation period and more often leads to the formation of postoperative complications: intestinal paresis and eventrations in the early postoperative period and ventral hernias in the long-term period [14-16].
With the necessary tools and thanks to the well-coordinated work of the operating team in many leading clinics, such operations are regularly performed from mini-access, which significantly reduces the postoperative burden on the patient and the timing of hospitalization, prevents the occurrence of early and distant complications [17-19]
Purpose of the study is to conduct a comparative analysis of the results of surgical treatment of patients during operations on the aortoiliac segment using a minimal incision.
From August 2020 to July 2022, 89 interventions on the aortoiliac segment were performed in the Department of Surgery at St. Luke Hospital, Simferopol. They included 16 aortobifemoral reconstructions and 73 linear bypasses and prosthetics. Of the total, 38 aortofemoral and iliofemoral bypasses were performed through a retroperitoneal access. The study groups included 51 patients with laparotomy access to the aorta, including 27 with a traditional access, and 24 using a minimal incision access.
The patients’ age ranged from 58 to 83 years, among them 37 men and 14 women. It is also worth noting that the group of patients who underwent a mini-access to the aorta included the oldest patients, patients with severe concomitant pathology and patients requiring repeated interventions after previous bypasses on the iliac and aortic segments.
By traditional access we mean a midline laparotomy of 25 to 35 cm in length. A mini-access was performed along the linea alba of the abdomen, by two thirds in the epigastric area and by one third in the mesogastric area, 7-9 cm long. Fig. 1, 2.
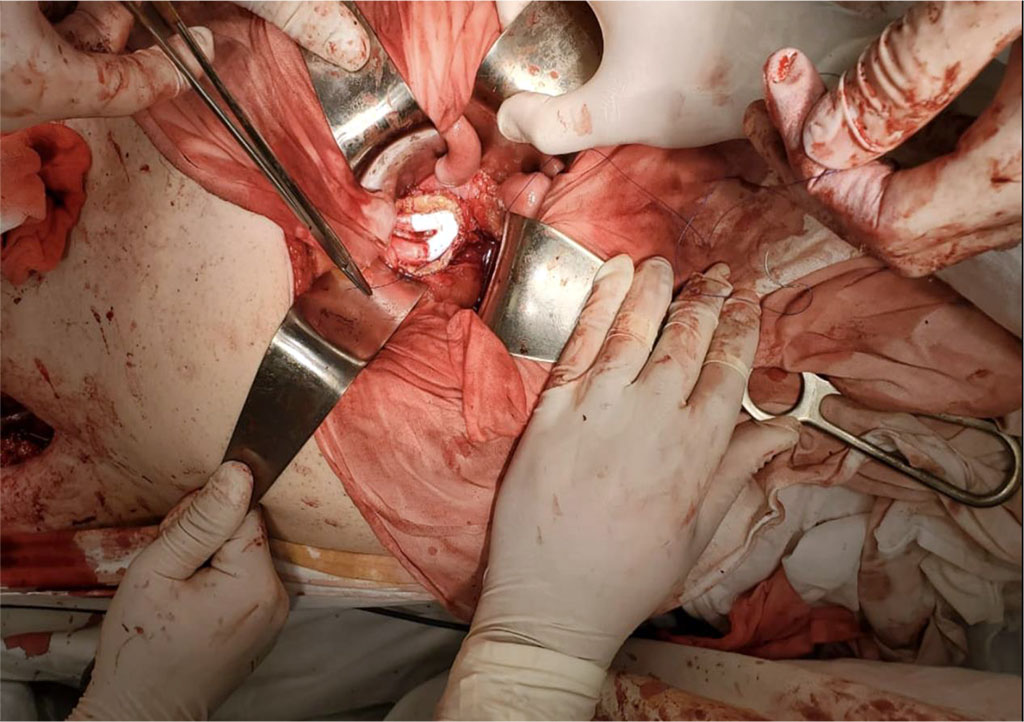
Figure 1. Formation of a proximal anastomosis - the end of the bifurcation prosthesis to the end of the aorta - through a mini-access in a patient with an aortic aneurysm

Figure 2. Completion of aortobifemoral alloshunting through a mini-access in a patient with Leriche syndrome
Additionally, the head of the operating table was moderately lowered and a bolster was placed under the patient’s lower back. The intestines were moved upward and to the sides using wet abdominal wipes, and the wound was expanded with three or four thin long hooks. In most cases, the duodenum was mobilized directly below the renal arteries to better visualize the aorta. The site for minilaparotomy access was chosen in the projection of the infrarenal aorta between the renal and inferior mesenteric arteries. This section of the aorta is usually less affected by atherosclerosis than the bifurcation and represents a good shuntable “site” for proximal anastomosis. In three patients with an aortic aneurysm, the aneurysmal neck was located immediately below the renal arteries, which also made it possible to use this surgical approach; two patients with a total aneurysm of the infrarenal aorta had the inferior mesenteric artery reimplanted. All surgeries were performed using spinal anesthesia with an epidural catheter at the stage of isolating the femoral arteries with a transition to endotracheal anesthesia at the abdominal stage. All patients were recommended to wear an abdominal bandage during the postoperative period. In the group with traditional access, 9 aorto-bifurcational and 18 linear operations were performed; in the mini-access group there were 7 bifurcational and 17 linear interventions. We analyzed the time of surgical intervention, the number of intensive care and postoperative bed days, and 42 of 51 patients were interviewed or examined from 2 to 16 months after the surgery for the occurrence of postoperative hernias.
Statistical analysis of the obtained data was carried out using the methods of variation statistics with the Student's test. Values at p≤0.05 were considered significant.
The duration of surgery was 196.5±26.7 minutes with traditional access and 146.3±16.7 minutes in the group with mini-access. On average, surgeries using the mini-access were shorter by 52.3±14.4 minutes than when using the traditional “classical” access. Tab. 1.
Table
1. Intra- and postoperative parameters depending on the method of
access to the aorta
(M±m; abs)
| Criteria | Type of access, type of surgery | |||
| Classic (n=27) | Mini-access (n=24) | |||
| Bifurcation (n=9) | Linear (n=18) | Bifurcation (n=7) | Linear (n=27) | |
| Duration of surgery (min) | 224,5±27,6 | 167,5±16,8 | 175,7±22,3* | 118,2±14,4* |
| Volume of intraoperative blood loss (ml) | 679,3±120,5 |
457,4±80,5 |
432,3±57,7* |
322,3±108,3 |
| Duration of pain relief (days) | 3,8±1,3 |
2,7±1,3 |
1,5±0,3* |
1,2±0,4* |
| Duration of treatment in the ICU (days) | 2,3±0,3 |
2,2±0,5 |
1,2±0,3* |
1,1±0,2* |
| Activation time (days) | 5,5±0,5 |
5,6±0,4 |
4,5±1,2 |
4,8±1,1 |
| Total bed-days (days) | 9,2±1,2 | 6,4±0,5* | ||
| Complications by Clavien-Dindo | ||||
| CDI | 7 | 6 | 2 | 1 |
| CDII | 3 | 1 | - | - |
| CDIIIA | - | - | - | |
| CDIIIB | 1 | - | - | - |
| CDIVA | - | 1 | - | - |
| CDIVB | - | - | - | - |
| CDV | - | - | - | - |
*– values at р≤0,05
It is worth noting that this access to the aorta, precisely at the level of the renal arteries, significantly simplifies operations with repeated reconstructions, since it allows to perform a low-traumatic operation even in the presence of adhesions and access to an intact aorta suitable for shunting.
For patients from the mini-access group, the period of stay in intensive care was 1.27±0.4 days. All patients in this group were activated the next day after surgery and began receiving enteral nutrition. The period of stay in intensive care for patients with the classic access was 2.3±0.4 days, which was associated with more severe pain and the need for prolonged epidural anesthesia, intestinal paresis in 4 patients, one of whom developed eventration requiring re-suturing of the laparotomy wound. Postoperative bed stay was 6.4±0.5 days for the group with mini-access, and 9.2±1.2 days for patients with classic access.
Among 42 patients in whom we were able to track long-term results, there were no complications in the form of postoperative ventral hernias in the group of patients with a mini-access; in the group of patients with traditional access to the aorta, a ventral hernia appeared in one patient 10 months after surgery and in one patient 2 months after laparotomy, for which they underwent allohernioplasty.
Thus, a minimally invasive approach provides better results than traditional midline laparotomy. It provides good visualization of the surgical field, however, it gives the surgeon a little less room for maneuver. If necessary, the minilaparotomy can easily be extended to a midline laparotomy. A small incision in the anterior abdominal wall and a thin postoperative scar provide an aesthetically pleasing result and the impression of a much less extensive surgical procedure. Minilaparotomy is technically feasible with access to the aortoiliac segment, has an acceptable great vessel clamping time, less blood loss and a lower percentage of complications in the early and postoperative periods.