- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 6: e1. DOI 10.35630/2022/12/6.27
Despite the progress observed in implantology and the rapid evolution of preventive and treatment options employed to treat major dental issues, the number of patients who need prosthetics with removable dentures still remains high, with no decrease trend to be expected soon. Modern dentistry, when dealing with issues related to dentition restoration, makes full use of basic thermoplastic polymers incorporating injection molding technology, whereas the said polymers can boast of such properties as biological inertia, proper aesthetics, strength, flexibility, resistance to external effects, lightness and elasticity. The conventional techniques used for cleaning and disinfecting removable dentures made of thermoplastic polymers fail to be up to the respective advanced requirements – such dentures create environments that are favorable for adhesion and microbial colonization. Aiming to evaluate the effectiveness of the modern means used for cleaning and disinfecting removable denture structures based on thermoplastic polymers, there was a study carried out to investigate the surface of 60 experimental samples of Acry-free ® thermoplastic, including methods of scanning electron microscopy and atomic force microscopy. To analyze the effect that cleaning and disinfecting agents work on the hygienic status of partially removable dentures made of thermoplastics (manufactured for 74 patients suffering from partial adentia), the Ambjornsen E. questionnaire was employed. The developed original set of preventive measures involved thorough oral hygiene activities with a manual toothbrush and mouthwash balms, as well as a consistent use of a special toothbrush and gel paste to take care of the removable dentures, followed with ultrasonic treatment and cleansing with effervescent tablets. The data of scanning electron microscopy and atomic force microscopy showed that using the original set of preventive measures resulted in improved quality of the thermoplastic polymers surface – by 1.1 – 1.5 times, if compared with conventional hygiene and disinfection products. As the data of sociological monitoring reveal, 12 into using the developed preventive measures, over 69% of patients were satisfied with the aesthetic properties of their dentures based on thermoplastics; as for the patients sticking to the practice relying on traditional hygiene and disinfection products, the similar indicator would not exceed 25%. In order to prevent the occurrence of major dental issues, as well as to increase the useful life of dentures made of thermoplastics and used by patients with partial adentia, it is wise to employ an individual approach to the selection of preventive measures that involve specialized extra hygiene products.
Keywords: removable dentures, thermoplastic polymers, hygienic status of dentures, oral hygiene, cleaning and disinfection of removable dentures, denture surface quality.
According to the statistics issued by the World Health Organization, partial absence of teeth is one of the most common diseases; the number of people with secondary adentia reaches 75% in various parts of the globe, the need for dental treatment with removable dentures going up to 58% [1].
Partial absence of teeth is characterized by functional and aesthetic issues affecting the masticatory & speech organs, and such issues include disturbed dentition unity; functional overload of the preserved teeth periodontium as well as that of the masticatory muscles and temporomandibular joints; a decrease in the interalveolar height; poorer appearance and speech [2-9].
Rational prosthetic treatment can be offered to patients with partial adentia only based on an individual approach thus aiming to recreate a stable morphological, functional and aesthetic optimum [10-17].
Experts claim that personalized prosthetic treatment cannot be performed without taking into account the craniofacial patterns, which is explained by the fact that the human bite depends on individual morphological and functional factors [18-26].
There have been more than a few studies focusing on the maxillofacial area and seeking to see whether or not the face parameters reveal any dependence on the size of various dental arches in case of physiological and proper functional occlusion. The authors have proven that the reconstruction of dental arches in patients with partial adentia will take an in-depth analysis of craniometric indicators, while also taking into account the structure type that the face gnathic parts may belong to [27-35].
In modern dentistry, there is an ever-growing interest that doctors take in basic thermoplastic polymers used to manufacture partial removable dentures. Thermoplastic polymers can offer the following advantages: high aesthetic value; flexibility; resistance to external effects; possible use of dentoalveolar clamps as fixation elements; minimal traumatic effect on the supporting teeth periodontal tissues; accurate fitting and stable fixation due to the thermal injection technology; elasticity; enhanced strength and maintainability; possible use as conditionally removable dentures that are fixed on implants with lock fasteners; biological inertia due to lack of a residual monomer; lack of hygroscopic capacity; leveling of the masticatory pressure peaks, which helps slow down the resorption and atrophy of the jaws alveolar ridge [36-40].
Experience shows that basic thermoplastic polymers bear certain significant technical disadvantages, which will affect the quality and durability of removable dentures, namely, such polymers being hard to process and polish, which will eventually result in a rapid loss of aesthetics and the patient’s dissatisfaction with the changing appearance of the dentures. Moreover, the increased microbial contamination of the dentures will increase the risk of occurrence (chronization) of the oral mucosa diseases [41-43].
The features typical of the dental health status manifested by older patients who use removable dentures include: concomitant somatic pathology; reduced adjustment capacity; multiplicity of dental pathology; high level of complexity in the dental system pathology; poor oral hygiene; lack of special knowledge concerning hygiene activities and means of care for removable orthopedic dentures; specific psychological status; limited finance availability [44-46].
The cleaning and disinfecting agents to be used to clean removable dentures, made of thermoplastic polymers, are subject to the following requirements nowadays: low toxic activity; antimicrobial activity in low concentrations; a wide range of action; lack of side effect due to the injection molding technological specifics; stability maintained through storage. In view of the above, the issue of studying the means and methods employed for disinfection and cleaning thermoplastic polymer-made removable dentures appears relevant, just like it requires further study.
Aim of the study: to examine the effect that preventive measures will have on the hygienic status of thermoplastic polymer-made removable dentures, based on the qualitative indicators of the dentures surface, and on the data obtained through a medical & sociological monitoring.
The study in question was a randomized clinical examination involving 74 patients (38 females and 36 males; age 45-68) with partial adentia (both the lower and the upper jaws), who applied seeking to restore dentition defects using removable dentures. The study group included patients featuring 6 or more teeth on one of the jaws; these were both patients who came for newly manufactured dentures (for the first time) and patients who came seeking repeated dentures. The prosthetic treatment for dentition issues was carried out using removable dentures made of Acry-free ® thermoplastic polymer (Perflex Ltd, Israel), Type 3 (ISO (1667-99)).
The measures, including dental clinical examination, instrumental and lab diagnostics, X-ray examination, prosthetic treatment, and sociological monitoring, was performed subject to the Protocol for the management of patients with partial absence of teeth. Depending on the study aims, the patients were broken into two groups. Group 1 (n=42; 23 females, 21 males) who got their first dentures (made of thermoplastic), had a set of preventive measures developed for them: 1) brushing teeth with a manual toothbrush and using toothpastes of both therapeutic and preventive effect; brushing done twice a day (morning and evening); 2) mouthwashing done with special balm-solution after meals; 3) a special toothbrush used for cleaning removable dentures (Paro Prothesen; Paro, Switzerland) and a toothpaste gel (Dentipur Gel; Helago Pharma, Germany), while the dentures were cleaned for 60 seconds; 4) ultrasonic treatment of removable dentures in a Sonic Denture Cleaner container (China) also using effervescent cleaning PRESIDENT tablets for dentures (Denture), treatment time – 10 min. Group 2 patients (n=32; 18 females, 14 males), after they got their removable dentures made of thermoplastics, followed conventional recommendations for prosthetic disinfection treatment. The soft plaque and food residue in this case were removed from the dentures with a toothbrush and a toothpaste, following which the dental set was washed in running water until completely cleaned. For disinfection, the dentures were placed in a 1% chlorhexidine digluconate solution for 10 minutes.
The patients were additionally asked to check if they are subject to and professional hazards, whether they comply with the rules of oral hygiene, practice bad habits, how much they smoke and consume coloring drinks, have any allergies, as well as questions were asked to find out their experience in terms of using removable dentures. The groups were formed so as to have approximately equal numbers of males and females, as well as around similar numbers of smokers in each. Once the dentures were made, the patients were instructed regarding the rules of use, proper oral hygiene, and made aware of hygiene products and modes of maintaining hygiene.
The data reported by patients concerning their personal subjective feelings, as well as their feedback on the hygienic condition of the removable dentures, were scored in points following the Ambjornsen E. method (1968). The plaque accumulating on the dentures was examined in 5 sites to be further evaluated based on a 4-point scoring system as per each site: 0 – no visible plaque could be obtained when scraping the dentures basis with a sharp tool; 1 – plaque was visible only on the tool used to scrape the basis; 2 – the areas under examination did contain some visible plaque; 3 – abundant visible plaque observed in the examined areas. The results were evaluated through summing up the scores for all the sites. The evaluation criteria identifying the contamination status on the removable dentures were as follows: 5.0-5.5 – very poor; 4.0-4.9 – poor; 3.0-3.9 – satisfactory; 2.0-2.9 – good; 1.0-1.9 – high.
The experimental part of the work implied producing 60 samples (15×15 mm in size) by injection molding using Acry-free ® thermoplastic polymer, following strictly the instructions as offered by the manufacturer. The processing was done employing metal, corundum, carborundum, electroplated diamond and vacuum-sintered diamond rotary tools of various type (cutters, heads, burs featuring various degrees of abrasiveness). Further on, all the samples were given finishing treatment (grinding, polishing) using dental equipment and respective supplies. Polishing was done until the visible shine status.
The finishing treatment over, the samples were placed in a solution of artificial saliva prepared based on the formula by T. Fusayama (1975): 0.42 g/l KCl + 0.4 g/l NaCl + 0.795 g/l CaCl2 + 0.69 g/l Na2HPO4 + 0.005 g/l Na2S9H2O + 1 g/l urea + distilled water up to 1 liter. The pH value of the artificial saliva was 6.5−7.3; t° - 37° C; exposure time – 12 hrs, which was a match to the average time dentures are used in between hygienic and disinfection treatment procedures. All the samples made from Acry-free ® thermoplastics were divided into two equal groups. The control group samples (n=30) received daily hygienic and disinfection treatment identical to the measures followed by the patients of Group 1: cleaning with a special Paro Prothesen toothbrush and Dentipur Gel paste-gel for 60 seconds; ultrasound treatment in a Sonic Denture Cleaner container using cleansing PRESIDENT tablets, for 10 minutes.
The comparison group samples (n=30), too, were treated according to the daily hygienic and disinfection practice identical to that followed in Group 2: cleaning with a medium-hard manual toothbrush and a hygienic toothpaste for 60 seconds; disinfection treatment in 1% chlorhexidine digluconate for 10 minutes. The total length of the experimental study was 30 days, after which all the samples were extracted from the artificial saliva solution in order to check the effect that the hygienic and disinfection treatment methods had on the quality indicators of the Acry-free ® thermoplastic surface.
The microstructure just like the surface quality of Acry-free® thermoplastic were evaluated through scanning electron microscopy and scanning atomic force microscopy. The Acry-free ® thermoplastic surface had its microstructure analyzed with a TESCAN MIRA 3 LMH scanning electron microscope (Japan) in three randomly selected fragments on each sample at ×200 and ×32000 magnifications, and at an accelerating voltage of 10.0 kV (Fig. 1).
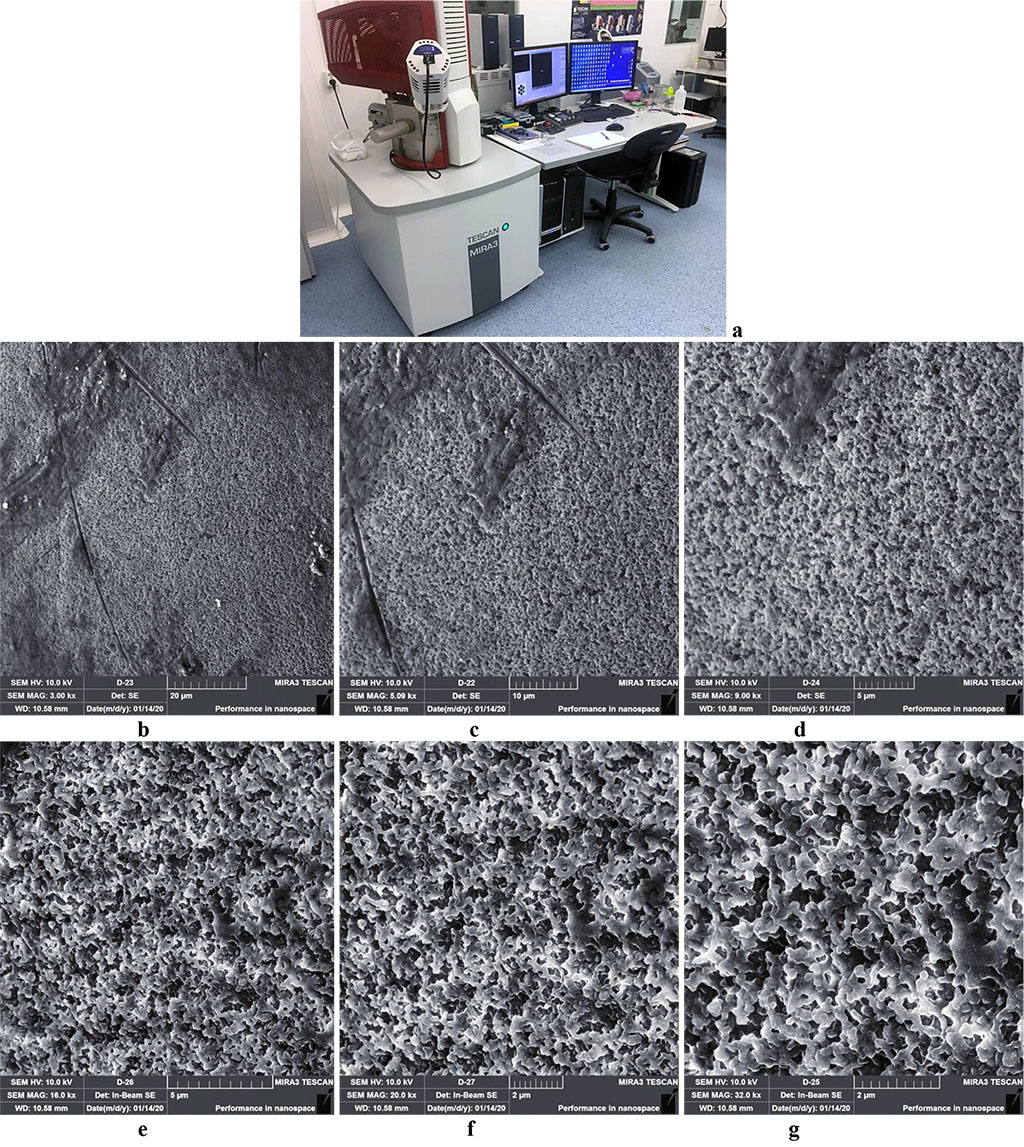
Figure 1. Scanning electron microscope TESCAN MIRA 3 LMH (a); surface microstructure of Acry-free® thermoplastic at ×3000(b), ×5000(c), ×9000(d), ×16000(е), ×20000(f), ×32000(g) magnification.
Atomic force microscopy, which allows obtaining a reliably objective surface a 3D-simulation of the studied areas, was done on a NTEGRA PRIMA scanning probe microscope (NT-MDT, Russia; resolution – from 50×50 microns to 10×10 microns; 1000 to 2000 scan points; frequency 1 and 0.5 Hz). There was the contact mode used with the NSG 10 NT-MDT cantilever (Fig. 2).
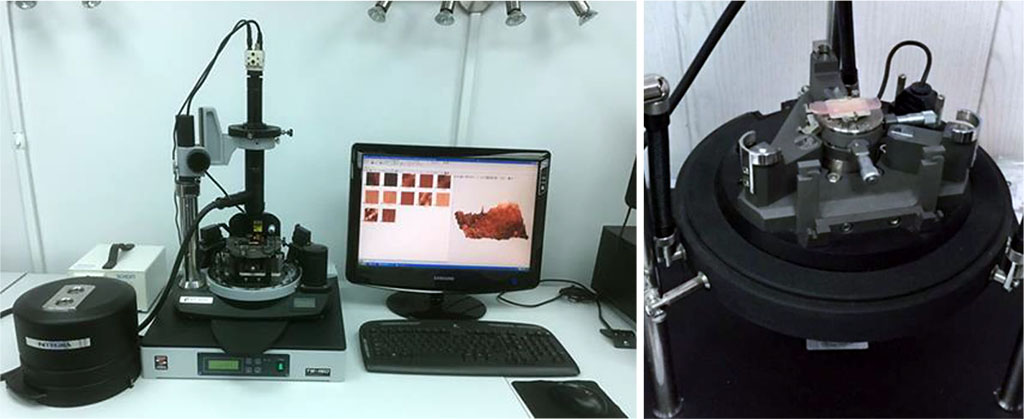
Figure 2. Scanning probe microscope NTEGRA PRIMA.
The heterogenous surface was controlled through the phase mapping method. To carry out a better visual study of the polymer samples surface, two-dimensional (2D) and three-dimensional (3D) models were analyzed. To check the normality distribution, the Shapiro-Wilk criterion was used. The data statistical processing was performed with IBM SPSS Statistics 24.0 software in Windows 10, while the differences were viewed as statistically significant at p<0.05.
The scanning electron microscopy outcomes obtained 30 days into the experiment, revealed surface quality defects in the microstructure of the Acry-free® thermoplastic polymer samples (Fig. 3,4).
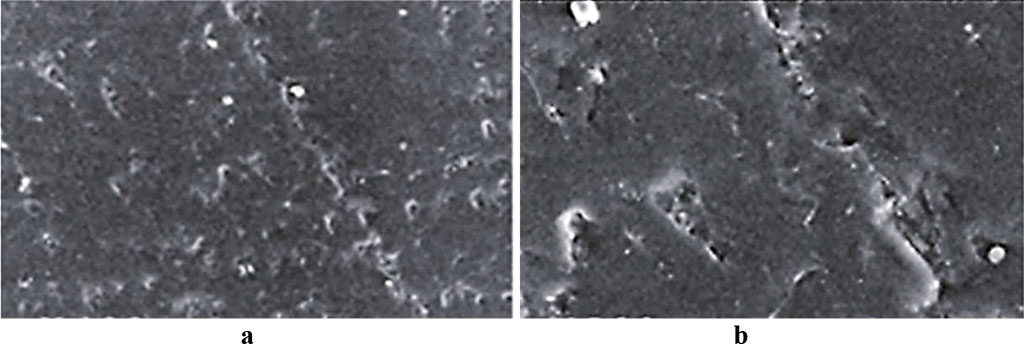
Fig. 3. Acry-free® thermoplastic sample surface, control group, 30 days into the experiment (a – magnitude ×200; b – magnitude ×500).
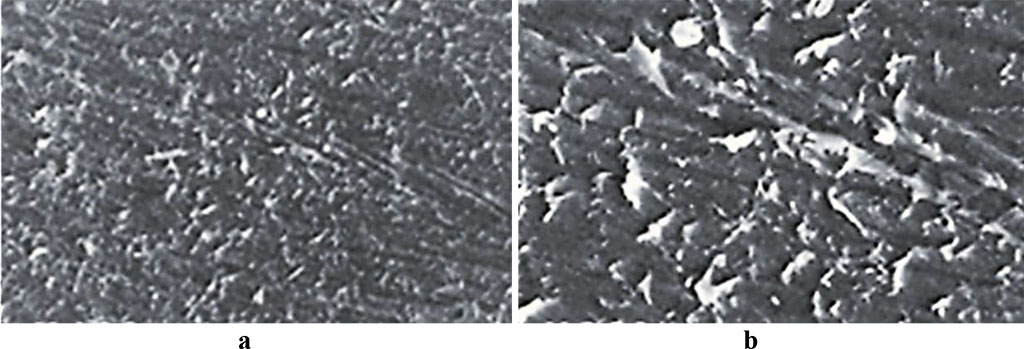
Fig. 4. Acry-free® thermoplastic sample surface, comparison group, 30 days into the experiment (a – magnitude ×200; b – magnitude ×500).
To reach a reliable assessment of the Acry-free® samples surface quality, as well as the respective microstructure, following various hygienic and disinfection procedures, we have developed a scoring system based on the following criteria: 0 points – no defect identified; 1 point – mild defect; 2 points – moderate defect; 3 points – significant defect. Table 1 offers a view of the surface quality defects observed on Acry-free® thermoplastics samples 30 days after the beginning of the experiment.
Table 1. Defects observed on the surface of Acry-free® thermoplastic samples, 30 days into the experiment (points)
| Samples | Type of defect | |||
| Abrasive surface | Cracks | Pores | Scratch lines | |
| Control group | 1 | 0 | 1 | 0 |
| Comparison group | 3 | 0 | 3 | 1 |
The scanning electron microscopy data show that 30 days following the start of the experiment, the microstructure of the Acry-free ® thermoplastic samples in the control group featured defects that could be described as abrasiveness/roughness and porosity of a degree to be classified as low. The samples in the comparison group, however, were found to bear defects like significant roughness and porosity, as well as they had slight or prominent scratch lines. Notable is that there were no such defects as crack observed in either of the two groups.
The Acry-free® thermoplastic samples had their abrasiveness parameters quantified. The said parameters were identified based on the images of the surface within a spot sized 50×50 nm, with atomic force microscopy employed, while using the following indicators: Ra – the arithmetic mean of the profile deviation absolute values within the base length; Rz – the sum including the average absolute values of the heights of the five largest profile projections, and the depths of the five largest profile depressions, within the base length; Rmax − the greatest height of the profile irregularities within the base length (Table 2).
Table 2. Abrasiveness parameters, Acry-free® thermoplastic samples, prior to, and following the experiment, (nm)
Samples |
Abrasiveness indicators | |||||
| Ra | Rz | Rmax | ||||
| Prior to the experiment | Following the
experiment |
Prior to the experiment | Following the
experiment |
Prior to the experiment | Following the
experiment |
|
| Control group | 53 ± 14 | 72 ± 29 ⃰ | 807 ± 264 | 883 ± 351 ⃰ | 94 ± 48 | 119 ± 61 ⃰ |
| Comparison group | 58 ± 12 | 106 ± 47 ⃰ | 789 ± 278 | 964 ± 512 ⃰ | 107 ± 42 | 172 ± 93 ⃰ |
Note. * − statistically reliable compared to the values obtained prior to the experiment (р<0.05).
As the atomic force microscopy results in the control group showed 30 days into the experiment, the surface morphology has the following averaged roughness parameters: Ra = 72 ±29 nm, Rz = 883±351 nm, Rmax = 119±61 nm. When assessing the surface quality of the control group samples, a few relief structures (depressions, bulges, scratches, ridges) were identified. The location density and the severity degree of these issues is insignificant (Fig. 5).
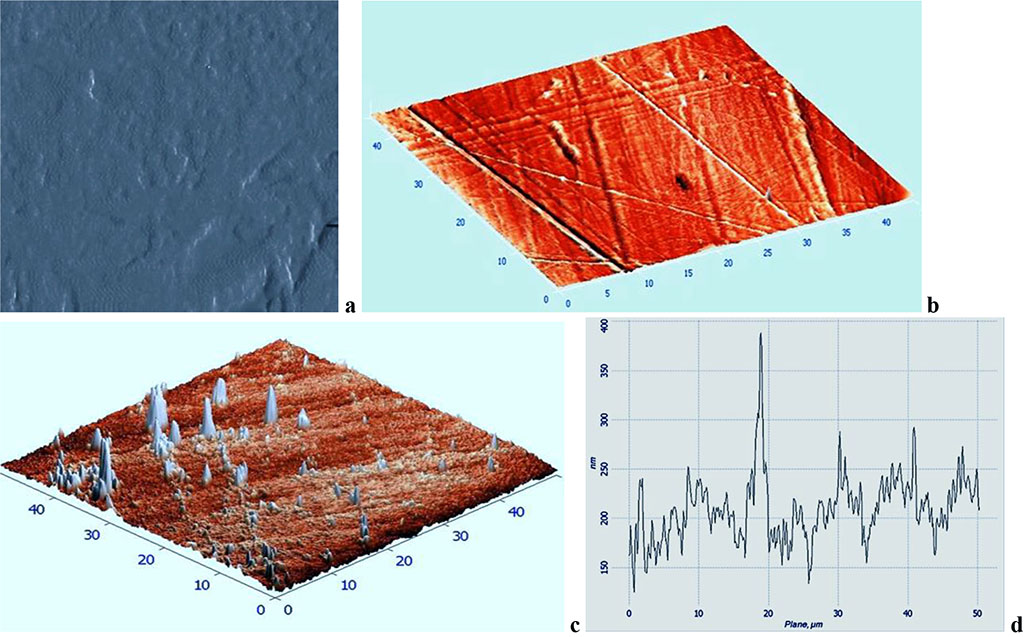
Fig. 5. Topographic two-dimensional (a), respective three-dimensional (b, c) AFM image and the surface profile curve (d) of the Acry-free® thermoplastics sample, control group, 30 days into the experiment (scanning area: 50×50 nm).
The AFM data obtained in the comparison group 30 days following the beginning of the experiment show that the surface morphology of the samples has the following averaged roughness parameters: Ra = 106 ± 47 nm, Rz = 964 ±512 nm, Rmax = 172±93 nm. When assessing the surface quality of the comparison group, a number of structure patterns were observed (depressions, bulges, scratches, ridges), while the location density and the severity degree of these formations was significantly above similar factors in the control group (Fig. 6).
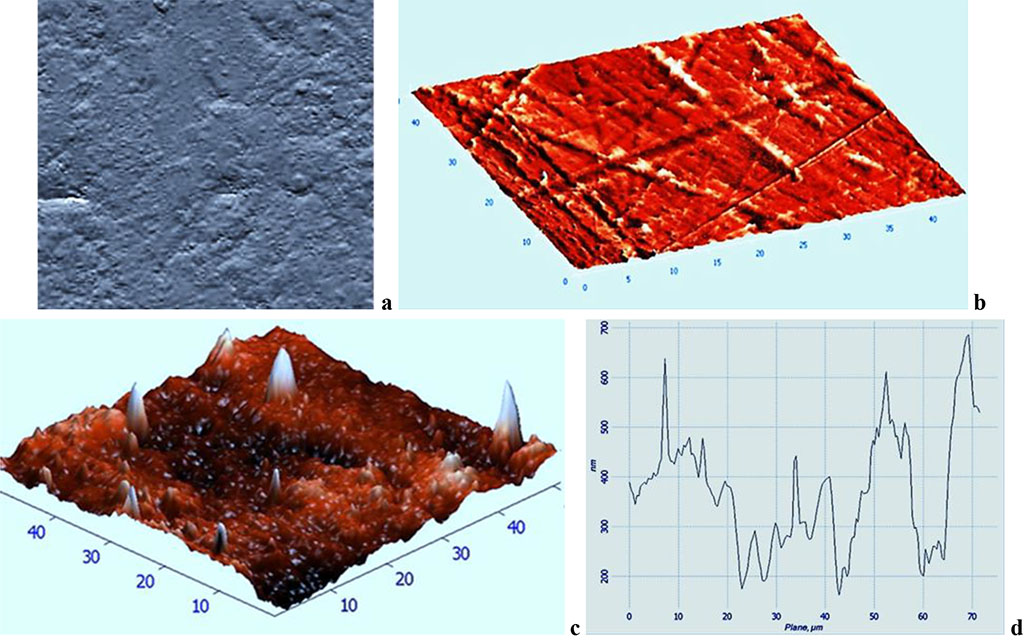
Fig. 6. Topographic two-dimensional (a), respective three-dimensional (b, c) AFM image and the surface profile curve (d) of the Acry-free® thermoplastics sample, comparison group, 30 days into the experiment (scanning area: 50×50 nm).
The surface quality analysis performed on Acry-free® thermoplastic samples 30 days into the experiment showed that the averaged quantitative roughness parameters (Ra, Rz, Rmax) in the control group were 1.1 – 1.5 times lower than similar values in the comparison group. The data obtained through atomic force microscopy indicate that, due to the specially developed preventive measures that were taken, the surface quality of Acry-free® thermoplastic samples featured a 10-50% improvement, if compared with traditional hygiene and disinfection products.
The survey revealed lack of patients’ awareness about hygienic procedures that can be used for oral care and dentures: 52.7% (n=39) of the patients were not informed about the specifics of hygienic oral care and removable dentures; 47.3% (n=35) received recommendations from the dentist; 36.5% (n=27) referred to booklets, brochures, and mass media as the source of information; 97.3% (n=72) did not know about special means to be used for cleaning removable thermoplastic dentures. As the survey data showed, 31.1% (n=23) of the respondents cleaned their dentures twice a day; 60.8% (n=45) cleaned the said appliances once a day, while 75.7% (n=56) brushed their teeth spending less than 2 minutes on the procedure, and changed the toothbrush once it got worn out. Of the entire number of respondents, 5.4% (n=4) used additional means, namely, cleansing tablets, to take care of their dentures; 12.2% (n=9) used dental powder to clean their dentures, with another 82.4% (n=61) never using any extra hygiene products.
Of all the Group 1 patients (n=42), following 30 days of using partial removable dentures made of Acry-free® thermoplastic, the level of cleanliness could be described as satisfactory in 30.9% (n=13) of the cases; 69.1% (n=29) had it good, whereas the poor level was not to be identified. As far as Group 2 is concerned (n=32), 30 days into using Acry-free® thermoplastic partially removable dentures, 53.1% (n=17) of the cases were found to have a satisfactory level of structural cleanliness; a good level was observed in 25.0% (n=8) of the cases, whereas the level considered poor was identified in 21.9% (n=7) of the cases.
An analysis of the sociological survey (questionnaire) data aimed at assessing the hygienic status of removable dentures (Acry-free® thermoplastic) makes it obvious that the best results were to be seen in Group 1 where the patients used the developed set of preventive measures, with more than 69% of patients left happy with the design, both the aesthetic and the pragmatic stance. As for Group 2, though, where conventional hygiene and disinfection products were used to clean the removable dentures, only 25% of the patients were satisfied with the aesthetics of the dentures, which means a need for regular preventive examinations to be held in order to control how clean the dentures are. Besides, there is also a need to select extra means for hygienic care, as well as professional cleaning of the removable dentures to be performed in a dental laboratory.