- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 6: e1. DOI 10.35630/2022/12/6.18
Varicocele is a disease that often occurs in infertile men. The prolonged existence of venous reflux in the pampiniform plexus of the scrotum contributes to the progress of the deterioration of the ejaculate, up to the total absence of germ cells in it. Aim: To assess the effect of varicocele on male infertility. Methods: All men (n=72) with varicocele and azoospermia included in the study were divided into two groups. In the first group (n=31), surgical treatment of varicocele was not performed and testicular biopsy was performed immediately. The men of the second group first underwent the microscopic subinguinal varicocelectomy, and after 6 months, according to indications, microTESE was performed. As a result, in the first group of patients, spermatozoa extraction was successful in 1/3 of men, and in the second group - in 2/3 (p<0.01).
Conclusion: In patients with azoospermia, surgical treatment of varicocele helps to restore spermatogenesis in 16.6%. Also, the operation according to the microscopic subinguinal varicocelectomy improves the effectiveness of testicular biopsy by 26.3%.
Keywords: Varicocele, male infertility, azoospermia, surgical treatment, microscopic subinguinal varicocelectomy.
Varicocele is a disease that is relatively common among young and middle-aged men. Varicocele rarely brings physical suffering to the patient. However, it is widely known that varicocele occurs frequently in men with impaired fertility. Among infertile men, varicocele is detected in 40% of cases [1, 2]. Many authors believe that with varicocele there is a "heat shock" of the scrotum, a decrease in testicular oxygenation, which leads to oxidative stress [3, 4]. Also, operations in the inguinal region can lead to impaired blood flow and venous outflow in the vessels of the spermatic cord, which can also change sperm fertility [5].
To date, there is no consensus on the correction of disorders in the ejaculate with varicocele. Most authors recommend surgical treatment of varicocele - ligation of the pampiniform plexus veins. Microscopic subinguinal varicocelectomy is considered the "gold standard" for varicocele treatment. After surgical correction of varicocele, sperm parameters improve in 70% of men and in almost half of the patients the chance of conception increases. This improvement in sperm quality usually becomes noticeable around 3–4 months after surgery [4]. Microsurgical varicocelectomy can improve sperm quality and increase sperm count by several times in patients with severe oligospermia [6]. However, it is still unclear the chances of conception after varicocelectomy in men with azoospermia.
Aim: To assess the effect of varicocele on male infertility.
The study included men (n=72) who, according to the semen analysis (WHO, 2010), had no spermatozoa in the ejaculate. All men consented to the study and analysis of personal data. All patients had varicose veins of the spermatic cord on the left. All men were diagnosed with varicocele based on physical examination of the scrotum and ultrasound of the testis and spermatic cord using the Valsalva maneuver. The presence of varicocele and azoospermia in patients of reproductive age were the inclusion criteria for patients in the study. The exclusion criteria were: age under 18 years, obstructive azoospermia, metabolic syndrome, abnormalities in the karyotype. Given the severe form of pathospermia in order to overcome the male factor of infertility in all patients in the future, it was supposed to perform a testicular biopsy (micro TESE) to obtain germ cells for egg fertilization using assisted reproductive technologies (ART).
All patients were divided into two equal groups. The first group included men (n=31), who underwent testicular biopsy immediately, i.e. without prior surgical treatment of varicocele. This tactic was used because of the patients refused the microscopic subinguinal varicocelectomy. The second group included men (n=41), who first underwent surgical treatment of varicocele (microscopic subinguinal varicocelectomy), and after 3 months, micro-TESE was performed to obtain spermatozoa from testicular tissue.
In all patients (n=72), we performed a histological examination of testicular biopsy. We performed standard histological posting of the material. All sections of the testis were stained with hematoxylin and eosin, followed by their study using light microscopy.
The statistical analysis was performed using spreadsheets “EXCEL” and “STATISTICA 8.0”. The significance of differences between quantitative indicators was assessed using the Mann - Whitney test. Differences were considered significant at p<0.05.
After six months of observation of patients of the second group, spermatozoa were found in the ejaculate in 7 (16.6%) patients. Therefore, these men were excluded from the study. Therefore, the second observation group finally consisted of 34 patients, and they underwent a testicular biopsy (micro TESE) because they had azoospermia.
In the first group of patients, spermatozoa extraction was successful in 11 (35.4% of patients). In the second group of patients, during testicular biopsy, germ cells were found in 21 (61.7%) patients (Fig. 1).
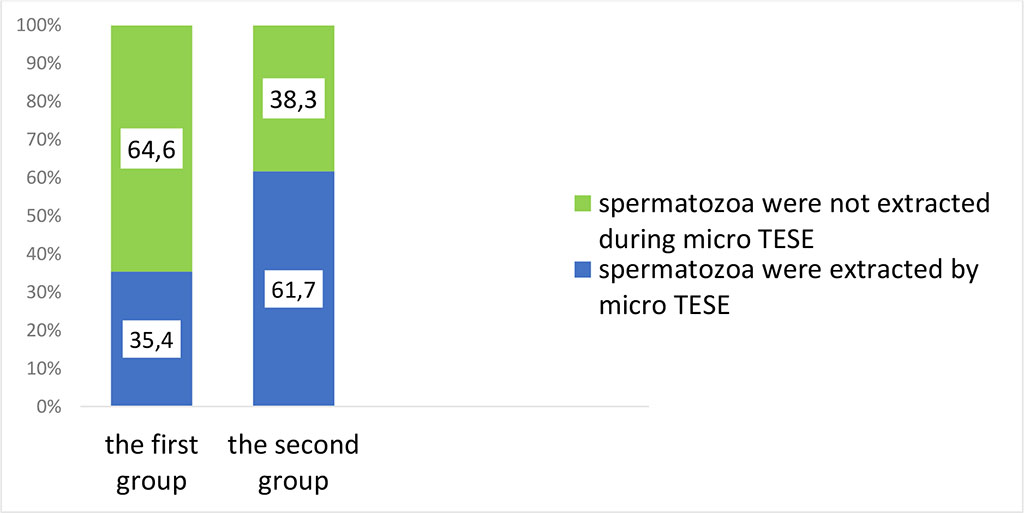
Fig. 1. The effectiveness of testicular biopsy (micro-TESE) in patients of the first and second groups.
Analysis of histological sections of testicular biopsies showed that in the majority of men of the second group 26 (76.4%), hypospermatogenesis and a block of spermatogenesis at the stage of round spermatids were detected in the convoluted seminiferous tubules. While in the first group of patients, similar indicators were encountered almost 30% less frequently (Fig. 2).
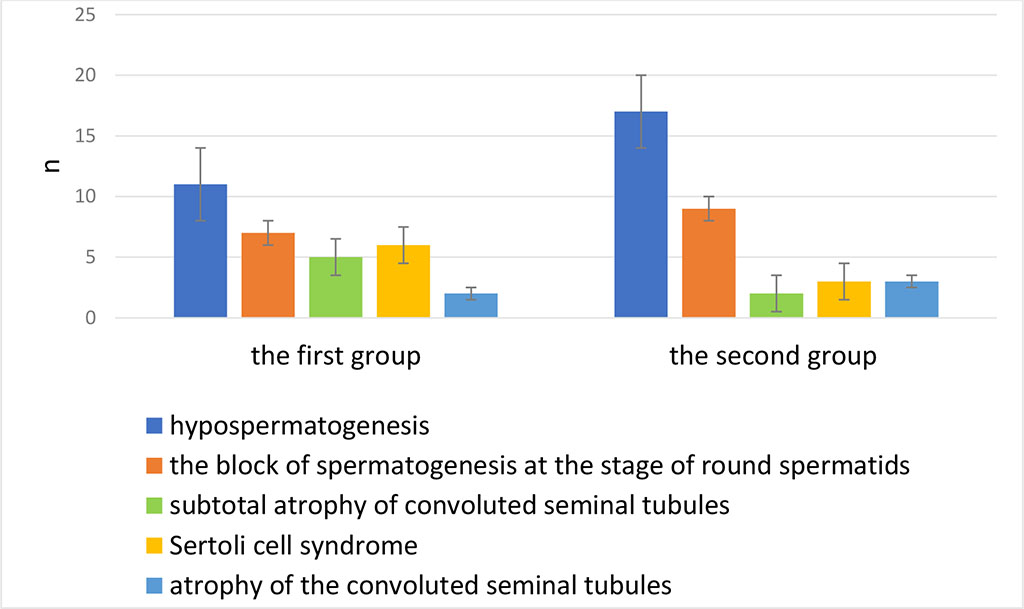
Fig. 2. Morphological Analysis of the results from testicular biopsies in the first and second groups
Varicocele is present in 4.3–13.3% of men with non-obstructive azoospermia [7]. Varicocelectomy helps eliminate venous reflux in the scrotum, eliminates factors that impair spermatogenesis. According to Jacobson D.L. and Ko E.Y., 18% of men with azoospermia improved spermatogenesis after simple varicocelectomy [4]. The results of the study by Birowo P. et al. showed that out of a total cohort of 104 men with azoospermia, spermatozoa suitable for ART were found in 29 (69.1%) patients who had previously undergone surgical treatment of varicocele versus 17 (27.4%) patients in whom varicocelectomy was not performed (relative risk: 2.51, 95% confidence interval: 1.60-3.96, P < 0.001) [1]. In turn, Seiler F found that ejaculate parameters returned to normal in 32% of patients after surgery using the microscopic subinguinal varicocelectomy. The authors found significant improvements in total sperm count (p < 0.005), sperm concentration (p < 0.005), and total motile sperm count (p < 0.005) among patients with severe oligozoospermia [8]. However, among patients with azoospermia, spermatozoa were found in the ejaculate only in 1 case. Our study showed that microscopic subinguinal varicocelectomy improves the condition of the spermatogenic epithelium and the effectiveness of testicular biopsy in every third patient with azoospermia [8].
Surgical treatment of varicocele in patients with azoospermia makes it possible to restore spermatogenesis in every sixth patients and improve the results of testicular biopsy by 26.3%. Therefore, microsurgical varicocelectomy improves the effectiveness of assisted reproductive technologies and enables the patient to become a genetic father.