- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 6: e1. DOI 10.35630/2022/12/6.15
As part of the refinement of the diagnosis, clinical management and therapy of patients with speech disorders, we present an analysis of the successful treatment of amnestic aphasia using valproic acid drug with electroencephalography monitoring for therapy verification. We suggest some organizational and neurological features of the implementation of clinical tactics in the treatment and diagnostic process in amnestic aphasia.
Keywords: amnestic aphasia, electroencephalography, diagnosis of speech disorders, treatment of speech disorders, depakine-chrono.
Diagnosis and treatment of speech disorders are relevant in modern medicine. Patients with cerebrovascular accident, traumatic brain injury, due to neurodegenerative diseases, often have speech disorders [1-5]. There are known attempts to apply innovative systems of intellectual digitalization and electroencephalography for diagnostics in the treatment of nervous diseases [6-10]. In this regard, as well as in order to clarify the organizational and clinical tactics of managing such patients, we present an analysis of a case of amnestic aphasia.
Patient M., 55 years old, a 6th grade metalworker at the plant undergoes an outpatient examination and treatment supervised by an experienced neurologist, MD. The patient applied for medical help, according to his wife and son, with complaints of "troubled communication due to forgetting words and names of objects and memory loss". Patient’s History. Sick for about 2 years after electric shock without fainting: examined "just in case" by emergency medical staff, had a consultation in the reception ward of a multidisciplinary clinical hospital of the regional center (routine examinations were made) - no pathology was detected, discharged with outpatient supervision at the place of residence. Due to the discovery and “gradual awareness of the lack of the ability to perceive speech with intact hearing, speech impairment of various levels and anxiety, he had to seek help.”
Examination was performed. Neurologist: Conscious. No meningitis signs. Cooperative. Oriented to time and place. Amnestic aphasia. Severe emotional lability. Pupils D = S. Pupillary light reflex is alert. Full range of eyeball movements. No nystagmus nor diplopia. Slight asymmetry of the nasolabial folds. Pharyngeal reflexes alert D=S. The tongue is in the middle line. Stable in the Romberg test. Coordination tests are completed. No paresis of the extremities, sensory disturbances, pathological foot and hand symptoms. The muscle tone of the limbs is preserved. Pelvic functions are controlled. Urinalysis - no pathology. Clinical blood analysis - Er - 5.0∙10¹²l; Hb - 154 g/l; Hb value - 0.97; Le - 6.3∙109l; ESR–7 mm/hour. Blood glucose - 5.3 mmol / l. Prothrombin–108%; fibrinogen - 2.8 g / l. RW-neg. Biochemical blood test: cholesterol-4.2 mmol/l; β-lipoproteins - 2.7 g / l; urea–6.4 mmol/l; ECG: sinus rhythm, 65 beats, normal position of the electrical axis of the heart. Ophthalmologist: retinal angiopathy. Therapist: apparently healthy. Fluorography – no pathology.
Speech therapist-aphasiologist: amnestic aphasia of moderate severity.
Brain MRI. The white matter of the parietal lobes contains, subcortically and paraventricularly, a few foci of gliosis (hyperintense in T2, T2-tirm, isointense in T1) without perifocal edema, up to 0.3 cm in size; the lateral ventricles of the brain are asymmetric (D<S), hydrocephalically enlarged (up to 0.8 cm on the right, up to 1.1 cm on the left), the third ventricle is enlarged up to 0.6 cm; convexity subarachnoid spaces and fissures are unevenly enlarged in the fronto-parietal areas; the lateral cerebral fissures are symmetrical, enlarged (Fig. 1-4).
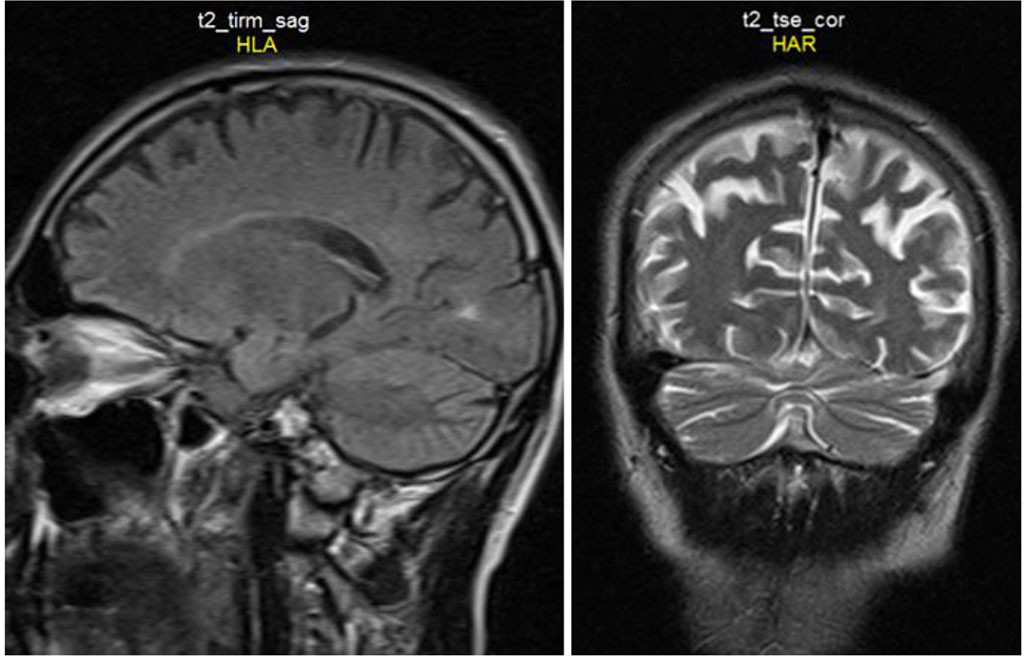
Fig. 1-2. See explanations in the text.
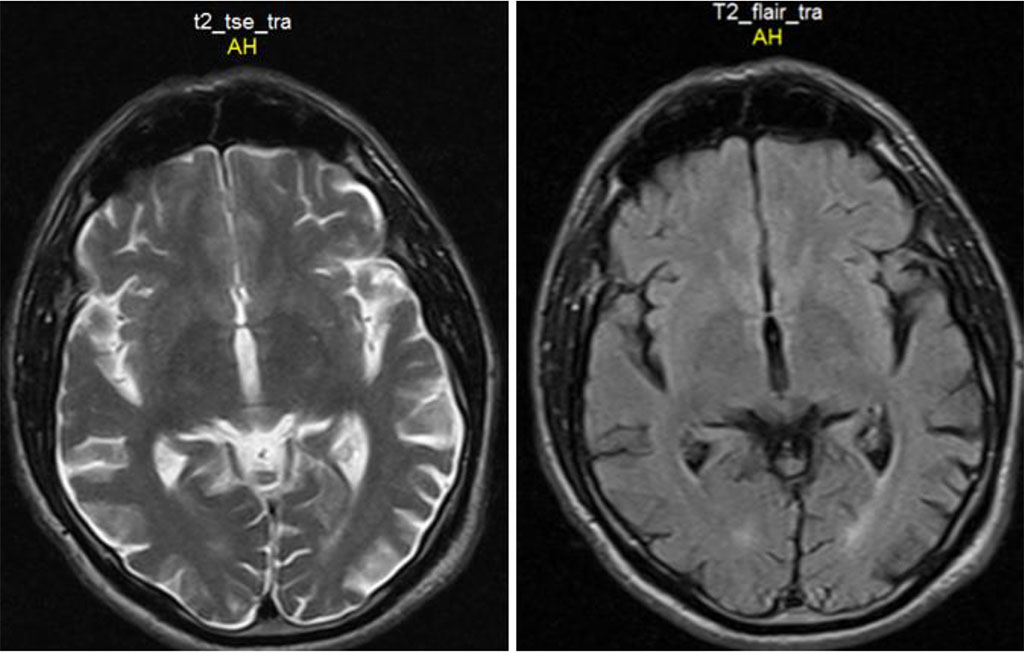
Fig. 3-4. See explanations in the text.
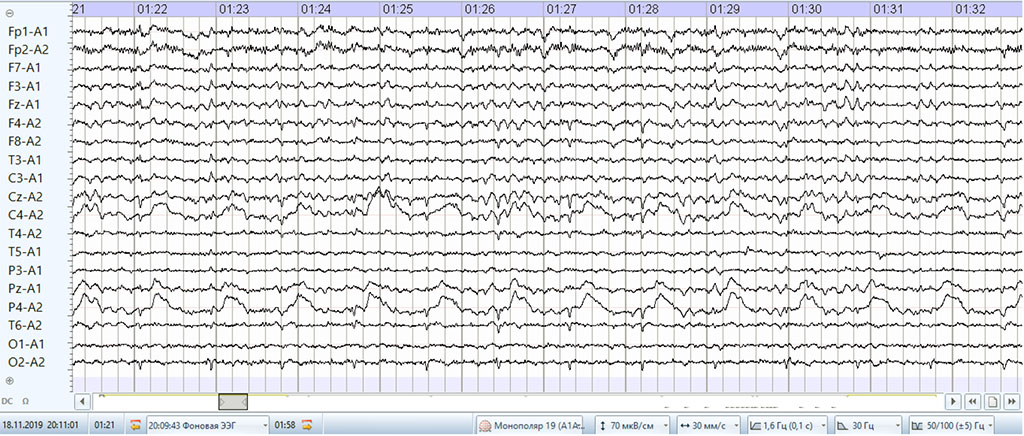
Fig. 5. Baseline EEG in amnestic aphasia (explanations in the text).
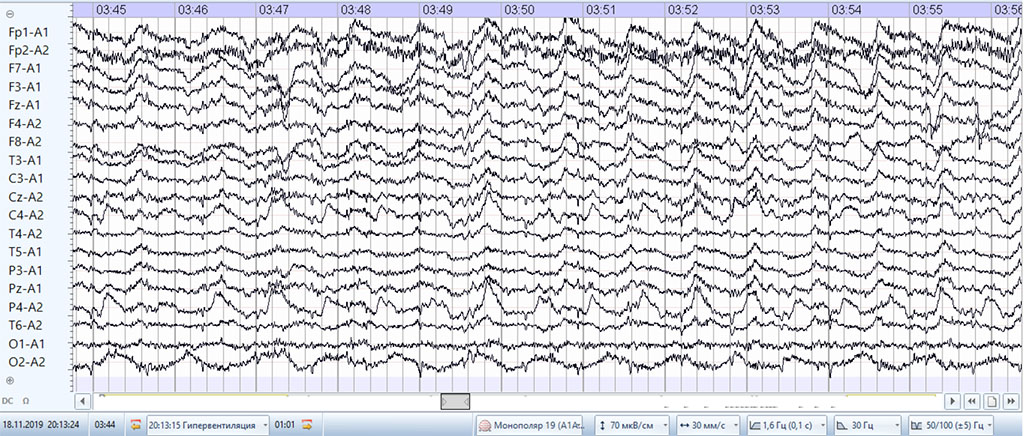
Fig. 6. EEG hyperventilation in amnestic aphasia.

Fig. 7. EEG with photic stimulation in amnestic aphasia.
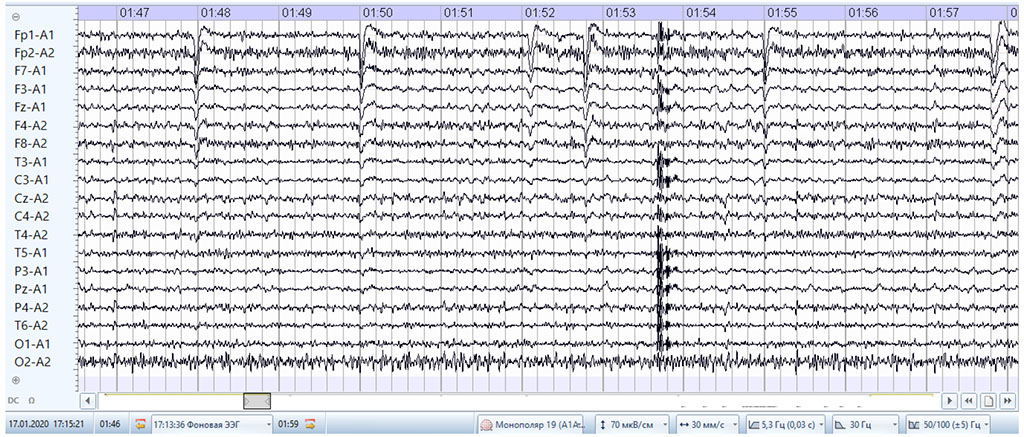
Fig. 8. Baseline EEG during the treatment of amnestic aphasia (explanations in the text).
Electroencephalography. Pronounced cerebral changes with flattened EEG biorhythms, disorganized main α-rhythm, persistent δ-range focus from the parietal and central deflections on the right in the background recording when opening the eyes, when closing the eyes, during hyperventilation, in the background after hyperventilation, during photic stimulation 3-, 8-, 15- and 21-30 Hz. A focus of the δ-range waves from the anterior frontal deflections of both sides during hyperventilation. Paroxysmal activity was not detected (Fig. 5-7).
Treatment: depakine-chrono 300 mg every 12 hours for 61 days.
Neurologist (dynamics): Amnestic aphasia is less pronounced. Emotional lability is less pronounced. The dynamics of the neurological status is improving.
Speech therapist-aphasiologist (monitoring): amnestic aphasia with positive dynamics.
Electroencephalography (monitoring). Positive dynamics has been revealed. Significant cerebral changes with a less pronounced flattening of EEG biorhythms, disorganized main α-rhythm, absence of a δ-range focus from the parietal and central deflections on the right in the background recording when opening the eyes, when closing the eyes, during hyperventilation, in the background after hyperventilation, during photic stimulation 3 -, 8-, 15- and 23 - 30 Hz. Paroxysmal activity was not detected (Fig. 8).
The proposed analysis emphasizes the organizational and neurological features of the history taking, the organizational interaction of medical staff, and the morphofunctional verification of the process which determines the following organizational and neurological features of amnestic aphasia:
Thus, in amnestic aphasia syndrome, the differential diagnosis is specified and the treatment is carried out taking into account electroencephalographic monitoring.