- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 6: e1. DOI 10.35630/2022/12/6.12
Background: Antibiotic-resistance is one of the most important problems in modern medicine. The overuse and misuse of antibiotics caused the development of drug-resistant pathogens. It is the reason for more difficult treatment for patients.
Objective: To monitor E.coli sensitivity to antibiotics and to evaluate its antibiotic resistance in a multidisciplinary hospital setting.
Methods: The study is presented by a statistical analysis of the results of microbiological examination of materials obtained from patients infected with E.Coli, treated in different departments of Tver Clinical Emergency Hospital (Russia) in 2018-2020. A total of 142 results of microbiological examination of urogenital tract, abdominal cavity and wound surfaces were processed.
Results: The number of antibiotics to which the Gram-negative Escherichia Coli is resistant also increases with the age of the patients. Among the investigated antibacterial drugs in terms of the total number of microorganisms with resistance to them, the lowest clinical efficacy was observed in the drugs of the cephalosporin series. Among the most frequent diseases caused by the studied strains of E.coli are intestinal infections and urinary tract infections. In addition, infections caused by persistence of E. coli as a background disease can significantly complicate the underlying disease.
Conclusion: The results present a rapid spread of resistance genes in the studied E.coli strains. It is the imperative for the improvement of antibiotic resistance monitoring using various laboratory methods. Based on the results of microbiological research it is necessary to create a database that will allow to select the optimal strategy for the drug treatment of patients according to its resistance profile.
Keywords: Sensitivity, antibiotic resistance, E.Coli, antibacterials.
The World Health Organization is concerned about the spread of antibiotic resistant strains of microorganisms. This phenomenon is now becoming an epidemic. In most countries, antimicrobial resistance to infectious agents increases every year. The increase of antimicrobial resistance has been linked to an increase in the use of antibiotics, due to a general lack of awareness of the need for caution in practice. A WHO survey of more than ten thousand respondents in 12 countries has exposed gaps in the understanding of the mechanisms by which antimicrobial resistance develops in microorganisms. For example, among one thousand respondents in Russia, only half (56%) had taken antibiotics in the previous six months. However, another part of respondents (44%) have started taking medication, without a medical prescription. Also, two-thirds (67%) of respondents thought that antibiotics can be used to treat viral diseases (e.g. flu), while a quarter of respondents (26%) stop taking the medicine once they feel better [1].
The challenge of preventing the growth of antimicrobial resistance is being addressed by a wide range of specialists from different fields. Among the main options for strategies to combat antimicrobial resistance are the development and introduction of innovative drugs, the systematization of data for treatment selection following individual patient resistance profiles. Prevention is also very important. It includes the raising awareness of the problem among all segments of the population, doctors and other health personnel [2,3,4,5].
E.coli bacteria occupy a special place in this case. Commensal strains of E. coli are an integral part of the normal human intestinal microflora. If specific virulence factors are acquired, opportunistic E. coli can form nosological strains which determine a wide range of diseases. In addition to typical intestinal pathologies, extraintestinal forms of the pathogen cause infections of other localizations, among which uropathogenic and meningitis-associated strains are the most common [6,7,8].
E. coli are widespread. The pathogenic strains are easily transmissible. They can remain on various surfaces in health care facilities for up to 18 months as a nosocomial infection. It makes it difficult to treat patients in hospitals due to the possibility of E.coli infection. The present study is therefore important in determining the severity of the problem and how to address it (WHO Information Bulletin, 31 July 2020).
Objective: Monitoring of E.coli sensitivity to antibiotics and determination of antibiotic resistance of this pathogen in a multidisciplinary hospital setting.
The study is presented by a statistical analysis of the results of microbiological examination of materials obtained from patients infected with E.Coli, treated in different departments of the Tver Clinical Emergency Hospital (Russia). Microbiological examinations of 142 patients from 2018 and 2020 were processed. The samples were obtained from the abdominal cavity, urogenital tract, cervical canal and wound surface of patients with purulent infections that are associated with E.coli persistence.
A standard method of bacteriological examination of microbial flora was carried out. It consists of material collection, transportation and inoculation of samples on nutrient media, followed by incubation in an electric dry-air thermostat TS-80 "KZMA", where the temperature was 37°C and the exposure time was 24 hours. In case of the presence of microbial growth, further diagnosis of strain sensitivity to various antibacterial agents was carried out by disc-diffusion method. The level of resistance of isolated microorganisms to antimicrobial drugs was assessed by estimating the diameter of the growth retention zone around the disks with the tested drugs in accordance with special tables.
Special attention was paid in this study to the most frequent diseases caused by E.coli persistence. The sensitivity and resistance of these microorganisms to common antibacterial agents in clinical practice were assessed, as well as the correlation of the above parameters with the sex and age of the patients.
In this study the average number of antimicrobials susceptible to which a given organism is sensitive was related to the gender of the patient. During the study period it was observed that strains colonizing female patients exhibited greater sensitivity to the full range of antimicrobials examined. The absolute number of effective drugs was calculated as a weighted average. The percentages were equated due to the different numbers of patients studied in the study years 2018 and 2020. In women, the value of the number of effective antimicrobial drugs in treatment was 4.67 drugs per person in both years and in men 3.89 in 2018 and 4.47 in 2020.
Changes regarding sensitivity to antimicrobials depending on the age of the patient whose microflora was the subject of the bacteriological study were also noted. The calculations were made according to the method previously described in order to exclude subjectivity in the methodology.
Three age groups were studied: patients younger than 40 years, 41 to 65 years, and older than 65 years.
The most vulnerable group, with the most antimicrobial resistant microflora in almost all time and age intervals, was young people under forty years of age. They were followed in half of the cases, particularly in males, by the group aged forty to sixty-five years. On average, the microflora of the group of patients aged sixty-five and above showed the highest sensitivity to the full range of drugs studied. In the study, based on an assessment of the mean values for practical use with patients in the group under forty years of age, there was an average "drop-out" of one drug from the physician's armory compared to the other patient groups (Table 1).
Table 1
| 2018 | ||||||||
| Age | Number
of patients surveyed |
Total number of effective antimicrobials in the group | Average value detected | |||||
| М | F | М | F | М | F | |||
| <=40 | 8 | 22 | 27 | 92 | 3,38 | 4,2 | ||
| 41-65 | 13 | 13 | 59 | 69 | 4,54 | 5,3 | ||
| >=66 | 6 | 16 | 19 | 77 | 3,17 | 4,8 | ||
| 2020 | ||||||||
| Age | Number
of patients surveyed |
Total number of effective antimicrobials in the group | Average value detected | |||||
| М | F | М | F | М | F | |||
| <=40 | 7 | 23 | 29 | 96 | 4,1 | 4,17 | ||
| 41-65 | 5 | 10 | 21 | 46 | 4,2 | 4,6 | ||
| >=66 | 6 | 13 | 31 | 68 | 5,17 | 5,2 | ||
During the analysis of the results, two correlations were found:
In addition to studying the correlation between patient age and bacterial resistance, the sensitivity of E.coli to various antibiotics was studied (Table 2).
Table 2
| Antibiotic | Sensitivity to antimicrobial drugs for 2018, % | Sensitivity to antimicrobial drugs for 2020, % | Changes, % |
| Tetracycline | 2,6 | 1,6 | -1 |
| Cifloproxacin | 15,4 | 1,6 | -13,8 |
| Ceftriaxone | 73,1 | 0 | -73,1 |
| Cefepime | 62 | 22 | -40 |
| Amikacin | 1,3 | 3,1 | 1,8 |
| Imipenem | 67 | 83 | 16 |
Our findings show the development of resistance of isolated strains to Ceftriaxone in 2020. Thus, comparing the sensitivity of E.coli to Ceftriaxone in 2018, there is a surge in resistance to the drug in patients under 40 years of age (32%), and a slight increase in patients over 65 years (6.25%).
In addition to Ceftriaxone, a decrease in E.coli sensitivity to Cifloproxacin, Cefepime, and a non-significant decrease in sensitivity to Tetracycline and several other drugs were observed. However, a relatively high efficacy in 2020 was observed for Imipinem (+16%), and sensitivity to Amikacin increased [3].
The highest antibiotic resistance of E.coli, on average, for 2020 is observed for drugs of generation III and IV. Absolute immunity was shown in the group of Cephalosporins: Ceftriaxone (generation III), Cefoperazone-sulbactam (generation III), and in the group of Fluoroquinolones - Moxifloxacin (generation IV). These studies indicate the general nature of the development of resistance of microorganisms to a number of drugs, and should be considered more broadly than in the framework of "nosocomial" infections.
Changes in E.coli sensitivity were observed in Tetracycline Fluoroquinolone group but in lower generations I and II, however they are not quite significant. Compared with 2018, in 2020 there was a sharp decrease in sensitivity to Cifloproxacin, a second-generation Fluoroquinolone antibiotic, from 15.3% to 1.56%, and to Cefepime, a fourth-generation Cephalosporin antibiotic, from 61.54% to 21.88%.
Despite the continued sensitivity of III generation drugs and more, they cannot be considered for the treatment of infections caused by Escherichia Coli, as they do not comply with the principles of rational antibiotic therapy.
E.Coli causes a wide range of diseases. The most common consequences of urinary tract infections are urolithiasis, benign prostatic hyperplasia, cervicitis, oophoritis and salpingitis. The most common gastrointestinal infections include acute appendicitis, cholelithiasis and intestinal obstruction. Often the infection can develop as a background disease, accompanying such problems as closed brain injury and combined injury. More detailed list of the identified diseases and the frequency of their occurrence could be seen in Figures 1 and 2.
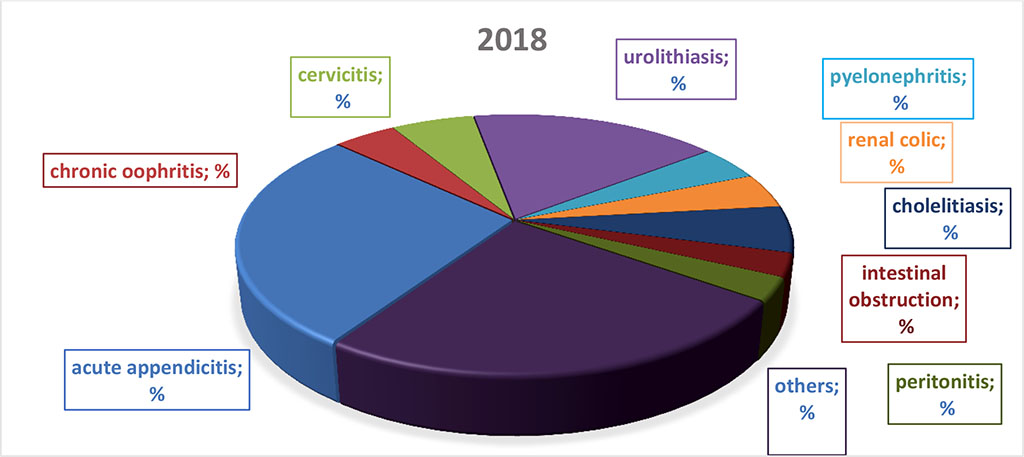
Figure 1
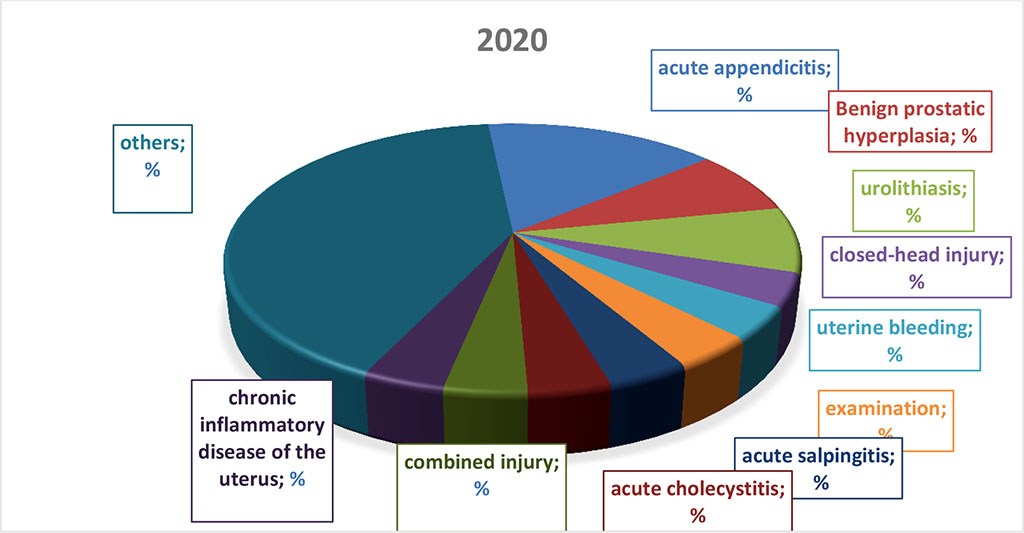
Figure 2
Antibiotics are some of the most important and significant medicines created by man and have been widely used in clinical practice for more than 70 years.
The research undertaken confirms the WHO's concerns on a small scale. The increasing qualitative and quantitative resistance of Escherichia coli to antibiotics complicates the treatment of patients with a wide range of diseases. Some of the antibiotics used in practice lose their efficacy, even in short-term studies. In the absence of changes in the indications and regimens of antibiotic therapy, the development of better drug resistance in microorganisms may be initiated in the future. To avoid complicating the situation, there is a need to improve the skills of doctors and other medical staff, to educate citizens about the need for sensitivity in antibiotic use, to create individual resistance profiles for each individual patient and to create a common base that will allow all levels to determine the most effective way of antibiotic therapy.