- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 5. DOI 10.35630/2024/14/5.507
Defining the sequence and methods of revascularization in patients with multifocal atherosclerosis should be associated with a minimal risk of adverse events and identification of predictors of adverse outcomes of operations, which is of great importance for improving the results of surgical treatment. We present a clinical case of successful treatment of a patient with multifocal atherosclerosis. The case included atherosclerotic disease of the left subclavian artery with complete steal syndrome of the brachiocephalic arteries, arteries of the lower limbs and arteries of the heart. It is shown that, when choosing a method for treating multifocal atherosclerosis, treatment should begin with preserving and restoring blood supply to the brain, and followed by restoring blood supply to other body parts.
Keywords: atherosclerosis, multifocal atherosclerosis, subclavian steal syndrome (SSS), stage-by-stage treatment, subclavian artery stenting, cerebral revascularization
Cardiovascular diseases are the leading cause of disability and mortality worldwide, and atherosclerosis is the main pathological process causing them [1]. Atherosclerosis is a systemic and chronic pathological change in the layers of the arterial wall that begins at an early age and remains latent and asymptomatic for a long time before progressing to advanced stages [2]. Atherosclerosis is a multifocal pathological process, widely studied in recent decades. It tends to develop over time in a completely asymptomatic manner, manifesting symptoms at a late stage, becoming difficult to treat from a clinical point of view, with even fatal events (acute myocardial infarction, ischemic cerebral stroke, etc.) [3-5].
Multifocal atherosclerosis is a topical modern challenge due to its high medical and social significance. The choice of optimal surgical treatment tactics for patients with multifocal atherosclerosis is complicated by the involvement of several arterial systems with a high risk of developing adverse events in each of them [6, 7]. Hemodynamically significant stenosis of the brachiocephalic arteries is verified in 20% of patients with indications for coronary artery bypass grafting. Determination of the revascularization method associated with the minimal risk of adverse cardiovascular events in this group of patients, along with the determination of predictors of adverse outcomes of operations, is of great importance for improving the results of surgical treatment.
Stenosis of the carotid arteries occurs in 15–20% of all patients who have suffered an acute cerebrovascular accident (including a transient ischemic attack). Clinical studies have shown that carotid endarterectomy reduces the absolute risk of ischemic stroke by 50% in patients with severe atherosclerosis of the brachiocephalic arteries. However, in the postoperative period, the likelihood of myocardial infarction increases, which has been noted in many randomized controlled trials [8]. Despite the fact that acute cerebrovascular accidents (including transient ischemic attacks) are frequent complications of surgical treatment of this group of patients, myocardial infarction is an equally important cause of disability and mortality. This conclusion is reflected in many clinical studies, while the risk factors for the development of infarction have not yet been fully studied [9].
Due to the lack of randomized studies and uncertainty in Russian and foreign recommendations regarding the choice of the optimal revascularization strategy in patients with multifocal atherosclerosis, the practical significance and relevance of the presented clinical case are beyond doubt.
The purpose of the study was to present a case from the authors' archive, with successful treatment of a patient with multifocal atherosclerosis.
A 69-year-old patient was routinely admitted with complaints of pain in the calf muscles at rest. From the anamnesis: considered himself ill for several years, since pain in the lower limbs first appeared while walking. He did not seek medical help. Over time, the pain-free walking distance decreased. After pain in the calf muscles appeared at rest, he was sent for additional examination. Results of clinical investigations: EchoCG dated 09.04.2024 – hypertrophy of the interventricular septum and posterior wall of the left ventricle. Atherosclerosis of the coronary arteries. The size of the heart chambers and hemodynamics within the age-related constitutional norm. The integrity of the septa preserved. The valve apparatus unremarkable. Ejection fraction 69%. EGD dated 10.04.2024 – erythematous gastropathy. Cardiac insufficiency of the 2nd degree. Ultrasound Duplex ultrasound of the arteries of the lower limbs dated 22.03.2024 – atherosclerosis of the arteries of the lower limbs. Hemodynamically significant stenoses of the common femoral arteries, popliteal arteries and deep femoral arteries on both sides. Subtotal stenosis of the left superficial femoral artery, occlusion of the anterior tibial arteries on both sides. CT scan of the brachiocephalic arteries dated 03.04.2024 – occlusion of the left subclavian artery. CT scan of the aorta and arteries of the lower limbs dated 29.03.2024 – total occlusion of the left common iliac artery and external iliac artery. Occlusion of both internal iliac arteries. Stenosis of the right external iliac artery at 69.1%. Occlusion of both superficial femoral arteries. Duplex ultrasound of the brachiocephalic arteries dated 16.04.2024: 1. Atherosclerosis of the extracranial sections of the brachiocephalic arteries with stenosis of (on the LEFT) common carotid artery at 30%; carotid bifurcation at 45-50%; orifice of the internal carotid artery at 50-55%; (on the RIGHT) common carotid artery at 25-30%; carotid bifurcation at 35%; orifice of the internal carotid artery at 45%; external carotid artery at 35%; orifice of the subclavian artery at 30%; 2. - S-shaped tortuosity of the right common carotid artery, without an increase in the linear velocity of blood flow. 3. Complete steal syndrome on the left. Associated diseases: Condition after AIS in the left middle cerebral artery territory on 02.06.2023. Chronic cerebral ischemia. Moderate cognitive impairment, right-sided pyramidal insufficiency, dysarthria. IHD, class I stable angina, atherosclerotic cardiosclerosis. 2A HF. Hypertension stage 3, risk 4. Ventral hernia.
The patient’s case was discussed at a multidisciplinary team meeting, and multi-stage surgical treatment was recommended: Stage 1 – transluminal balloon angioplasty with stenting of the left subclavian artery, Stage 2 – aortofemoral bifurcation bypass.
Description of the surgical intervention: Access: right brachial artery. Set of surgical consumables: Hydrophilic guidewire 0.35 – 1 pc, Absolute Pro 10.0×60 mm peripheral self-expanding stent – 1 pc. Using local anesthesia Sol. Lidocaini 0.5%-2.0 ml, the left brachial artery was punctured and catheterized. A 6 Fr. introducer was installed. Direct angiography of the left subclavian artery was performed. Occlusion at the orifice of the vertebral artery was visualized. Fig. 1-3.
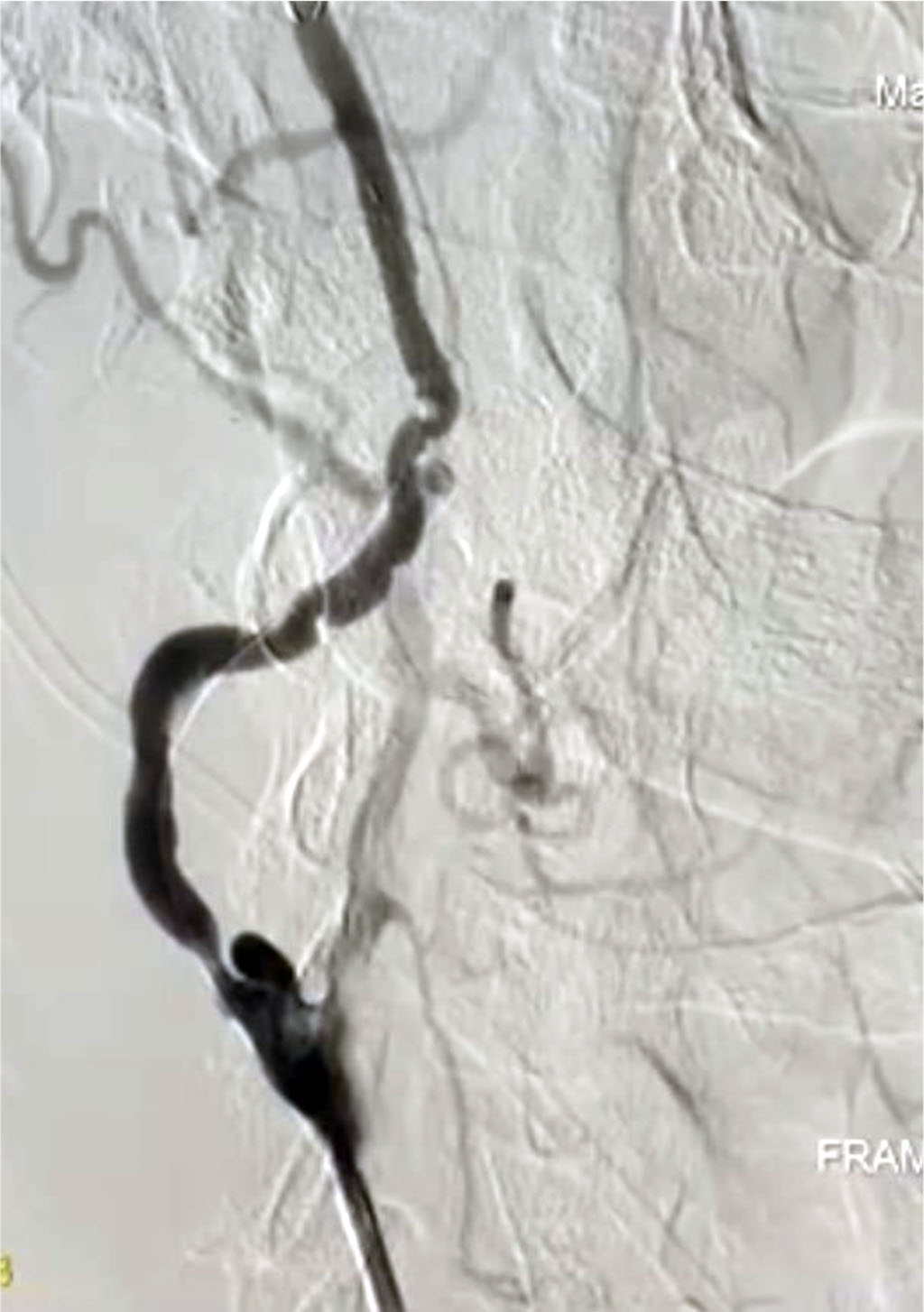
Fig. 1. Subclavian steal syndrome, blood supply to the arm through the left vertebral artery

Fig. 2. Subclavian steal syndrome, stenosis of the left subclavian artery
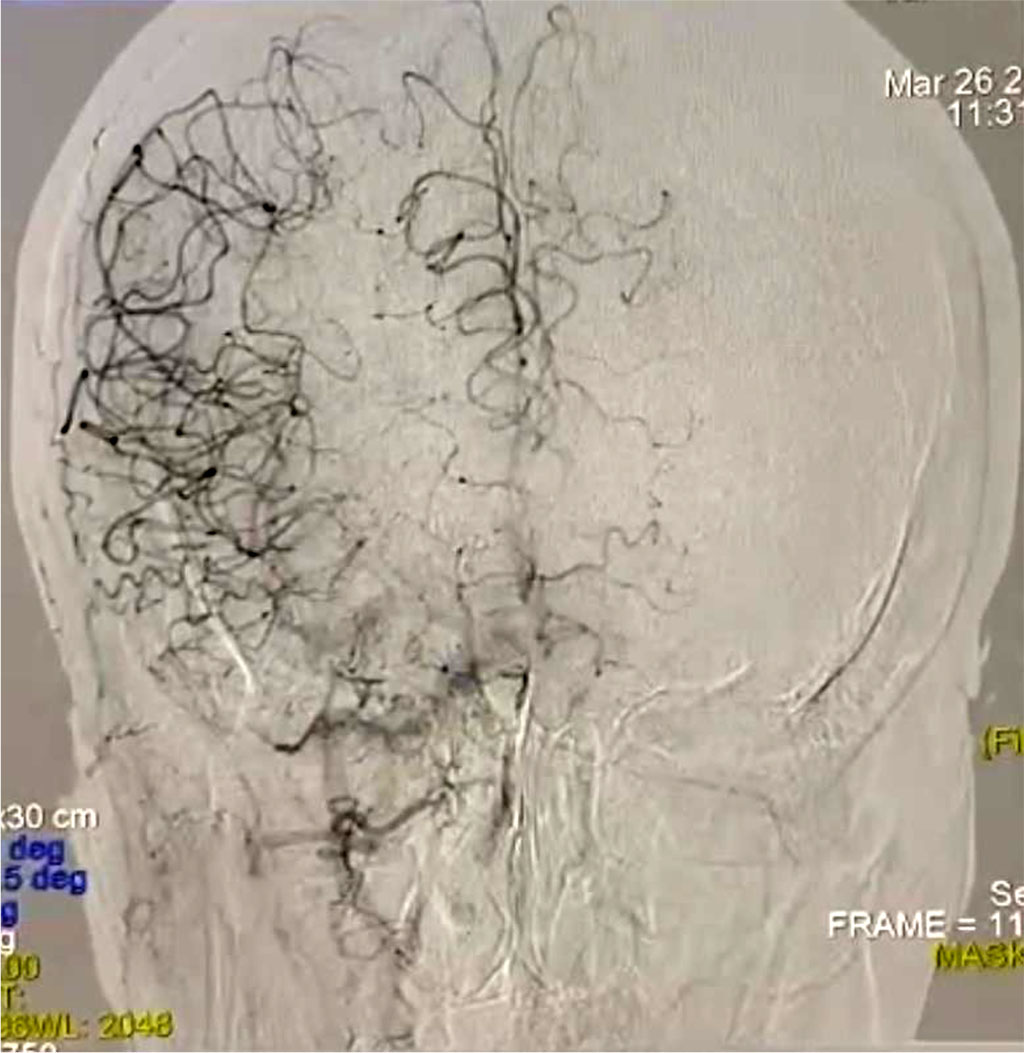
Fig. 3. Lack of blood supply in the left hemisphere
Recanalization was performed with a Comand guidewire followed by BAP in the occlusion site with 8.0x20 mm balloon catheter. A 10.0×60 mm Absolute Pro self-expanding stent was delivered antegradely through the introducer along a 0.35 guidewire and implanted at the orifice of the left subclavian artery, then postdilatation was performed with a 8.0×20 mm balloon catheter under a pressure of 8-10 atm. According to the control, the left subclavian artery was patent, without signs of malposition, proximal nor distal dissection, no distal embolism was detected.

Fig. 4. Stenting of the left subclavian artery

Fig. 5. Restoration of blood flow in the left hemisphere
The stent was implanted in the desired position. The instruments were removed, a pressure bandage was applied. Recommendations: 1. Bed rest for 24 hours. 2. Monitoring the puncture site. 3. Follow-up ultrasound examination.
Stenosis of the left subclavian artery leads to steal syndrome due to the discharge of blood from the vertebrobasilar system into the blood flow of the left upper limb. Due to this, cerebral ischemia and weak blood supply to the arm occur. Steal syndrome is not often encountered in practical medicine, being, as a rule, a manifestation of multifocal atherosclerosis. The result is a reversal of blood flow in the vertebral segment on the affected side. Blood does not flow to the basilar artery (located in the posterior cranial fossa) which supplies the brainstem, temporo-occipital brain regions, and cerebellum [10]. The indicated cerebral areas are subject to ischemia, which is clinically manifested by vertebrobasilar symptoms [11,12].
According to the results of one meta-analysis, the incidence of adverse coronary events is significantly higher after carotid endarterectomy compared with carotid angioplasty with stenting, which was associated with the administration of dual antiplatelet therapy after stenting, as well as with the activation of proinflammatory cytokines and a prothrombotic condition as a result of open surgery [13,14].
When choosing a method for treating multifocal atherosclerosis, treatment should begin with preserving and restoring blood supply to the brain, and at the next stage, to other body parts.