- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 5. DOI 10.35630/2024/14/5.503
Objective: The aim of the analysis was to assess the impact of perioperative education and the use of advice from a psychosexologist on the quality of life, including sexual life, of patients with an intestinal stoma.
Methods: Data were collected from 150 stoma patients. The Patient Identification Form, Body Esteem Scale (BES), Female Sexual Function Index (FSFI), and International Index of Erectile Function (IIEF) were used to compile and evaluate data.
Results: An analysis showed that patients who received comprehensive information in the post-operative period about stoma care and management were less likely to report complications. In the study conducted, there was no evidence of an impact of the use of psychological or psychosexual counselling on the body image and sexual functioning of patients with an intestinal stoma.
Conclusion: Postoperative education is an important element in reducing the number of postoperative complications and is an important way to achieve independence related to stoma care.
Keywords: stoma, perioperative education, postoperative complications, sexual functions, psychosexologist.
A stoma is an intentional connection between the lumen of a hollow viscus and the skin or mucosal surface. An intestinal stoma is created through exteriorizing the retained end of the bowel by dissecting the abdominal wall outside the abdominal cavity, then turning the bowel mucosa outward and suturing it to the skin. Intestinal stoma surgery is carried out for both elective and urgent indications. The most common indications for the creation of an intestinal stoma are colorectal cancer, diverticular disease and inflammatory bowel disease [1].
As a result of the creation of a stoma, there is a loss or reduction in the ability to store gastrointestinal contents and a loss of ability to control excretion. Self-image, living situation, self-esteem and self-acceptance are all altered [2].
Patients often feel uninformed about stoma management, and these feelings are associated with emotional and social problems. Stoma-related complication rates are high, negatively affecting the patients' quality of life [3]. Not surprisingly, perioperative re-hospitalisation rates due to complications of stomas are high, and this in turn impairs the functioning of medical facilities. Complications involving the skin around the stoma are the most common problems encountered in patients with an intestinal stoma, with an estimated incidence of 75% [4].
A study by Werth et al [5] found that 90% of patients felt that education during their hospital stay about stoma self-management was essential. Perioperative education helps patients adapt to life with a stoma, improving their quality of life and reducing complications and hospital readmissions. It is an important pathway to achieving independence related to stoma care. It can be seen that patients who have learned how to manage their stoma comfortably show a higher level of acceptance of their condition, which reflects positively on their level of life satisfaction [6].
In addition to the patient, family members should also be educated, as many feel inadequately prepared to assist with stoma care. Patients and their caregivers should be informed about the nature of the disease, the nature of the surgery, and the type of stoma. Basic information on the physiology of the stoma, such as the correct volume of fluid excreted and the consistency of the discharge, should be discussed with the patient. Patients should be provided with a basic understanding of stoma care products. Importantly, patients should be shown practical stoma care skills, such as removing the old stoma bag, adjusting the size and fitting a new bag. Each patient should be given the opportunity to perform these tasks under the supervision of a stoma nurse. This will increase the patient's knowledge and skills in dealing with such problems as leaking appliances or skin irritation around the stoma [7].
Research examining the impact of perioperative education on the quality of life of patients with a stoma is limited. The aim of the analysis was to assess the impact of perioperative education and the use of advice from a psychologist and/or psychosexologist on the quality of life, including sexual life, of patients with an intestinal stoma.
This was a descriptive, cross-sectional study. Data were collected from 150 stoma patients at the Clnical Hospital in Poznań and at the Department of General and Colorectal Surgery at the hospital in Łódź and at the Lower Silesian Oncology Center in Wrocław. Some of the survey questionnaires were obtained using the CAWI method (Computer-Assisted Web Interviewing). The research was conducted between April 2021 and April 2023 after obtaining necessary permissions. Those who agreed to participate in the study aged between 20 and 70 years, who had a sexual partner and who underwent ileostomy and/or colostomy were involved in the study. People who had a urostomy, people without sexual initiation and patients diagnosed with mental disorders were excluded from the study. The Patient Identification Form, Body Esteem Scale (BES), Female Sexual Function Index (FSFI), and International Index of Erectile Function (IIEF) were used to compile and evaluate data.
This study was approved by the Bioethics Committee of the Medical University of Silesia in Katowice (PCN-CBN/0022/KB1/95/21).
This form consisted of three sections: (1) sociodemographic characteristics (e.g., age, education level, marital status, chronic disease, medicine use, employment status), (2) stoma characteristics (e.g., type of ostomy, indication, stoma status, stoma care), and (3) treatment characteristics (e.g., type of surgery, type of adjuvant treatment).
The Body Esteem Scale (BES) allows determining the respondents’ attitudes toward their bodies in three subscales: Sexual Attraction (SA), Weight Concern (WC), and Physical Condition (PC). The scale consists of 35 items that can be answered on a 5-point Likert scale, scoring from 1 to 5, where 1 means I have strong negative feelings, 5 means I have strong positive feelings, and 3 means a neutral attitude. The scale takes into account 3 areas related to self-assessment of one’s body: sexual attractiveness, weight concern, and physical condition. The score is obtained after adding all the points, and as the number of points increases, the body evaluation increases.
Female Sexual Function Index (FSFI), a 19-item questionnaire assessing sexual function and satisfaction across five domains including sexual desire, arousal (both subjective and physiological), lubrication, orgasm, satisfaction, and pain. Women with a total score above 26.55 should be classified as sexually functional, with those scoring below the cutoff indicating sexual dysfunction.
This index includes 5 subscales for a total of 15 questions: erectile function (questions 1 through 5 and 15), sexual satisfaction (questions 6 through 8), orgasm (questions 9 and 10), sexual desire (questions 11 and 12), and overall satisfaction (questions 13 and 14). Each question on the IIEF is scored from 1 to 5 points, where 1 = severe dysfunction and 5 = no dysfunction. The total score range is 5 to 75. Based on this score, the degree of erectile dysfunction (ED) is classified as normal (>25), mild (17 to 25), moderate (11 to 16), or severe (0 to 10).
Data analysis was performed using SPSS 29.0 (Statistical Package of Social Science) software. Data were analysed using descriptive statistics methods (i.e. frequencies, percentages, mean scores, standard deviation, etc.). The Shapiro-Wilk test was used to determine the normality of the distribution. The chi-square goodness of fit test was used to determine whether the proportions of categorical outcomes were all equal. The chi-square test of independence was used to test the relationship between categorical variables and subgroup analyses were performed using Z test with Bonferroni correction. Relationships between quantitative data were analysed using r-Pearson and rho-Spearman correlations. Student's t-test was used to compare mean values of independent groups, while the Mann-Whitney U test was used to compare median values.
A total of 150 subjects participated in the study, including 81 women (54.0%) and 69 men (46.0%). The average age of the participants was 47.65 ± 13.05 with 39.03% of them received a secondary education and 36.0% a master's degree.
Table 1. Sociodemographic characteristics of participants at baseline
| Baseline characteristic | n |
% |
| Sex | ||
| Female | 81 | 54.0% |
| Male | 69 | 46.0% |
| Marital status | ||
| Single | 6 | 4.0% |
| Informal relationship | 28 | 18.7% |
| Married | 100 | 66.7% |
| Separated | 2 | 1.3% |
| Divorced (in informal relationship) | 10 | 6.7% |
| Widowed/widowered | 4 | 2.7% |
| Place of residence | ||
| Rural area | 44 | 29.3% |
| Town up to 50k inhabitants | 25 | 16.7% |
| City with over 50k to 100k inhabitants | 27 | 18.0% |
| City with over 100k to 200k inhabitants | 21 | 14.0% |
| City with more than 300k inhabitants | 33 | 22.0% |
| Education level | ||
| Elementary | 4 | 2.7% |
| Junior high school | 2 | 1.3% |
| Secondary | 59 | 39.3% |
| Post-secondary | 11 | 7.3% |
| Higher - bachelor's degree | 20 | 13.3% |
| Higher - master's degree | 54 | 36.0% |
| Employment status | ||
| Employed | 89 | 59.3% |
| On disability | 31 | 20.7% |
| Retired | 23 | 15.3% |
| Unemployed | 4 | 2.7% |
| In training | 3 | 2.0% |
Table 2 shows the distribution of patient responses relating to the characteristics of their stoma and life after surgery.
Table 2. The nature of the stoma emerged in patients and its management
| Baseline characteristic | n | % |
| Stoma type | ||
| Ileostomy | 73 | 48.7% |
| Colostomy | 73 | 48.7% |
| m/d | 4 | 2.7% |
| Type of the stoma surgery | ||
| Emergent surgery | 73 | 48.7% |
| Elective surgery | 77 | 51.3% |
| Stoma duration | ||
| Permanent | 83 | 55.3% |
| Temporary | 65 | 43.3% |
| n/d | 2 | 1.3% |
| Reasons for performing stoma | ||
| Cancer | 65 | 43.3% |
| Inflammatory Bowel Disease | 49 | 32.7% |
| Intestinal obstruciton | 17 | 11.3% |
| Abdominal injury | 2 | 1.3% |
| Familial Adenomatous Polyposis | 1 | 0.7% |
| Other | 16 | 10.7% |
| Pre-surgery education | ||
| Yes | 84 | 56.0% |
| No | 66 | 44.0% |
| Post-surgery education | ||
| I was given comprehensive information | 85 | 56.7% |
| I have received partial information | 58 | 38.7% |
| I have not received information on this subject | 7 | 4.7% |
| Follow-up therapy after surgery | ||
| Yes | 52 | 34.7% |
| No | 98 | 65.3% |
| Use of a psychologist or psycho-sexologist services | ||
| Yes | 26 | 17.3% |
| No | 124 | 82.7% |
| Use of a stoma clinic services | ||
| Yes | 77 | 51.3% |
| No | 73 | 48.7% |
| Participating in ostomy support groups | ||
| Yes | 67 | 44.7% |
| No | 82 | 54.7% |
| m/d | 1 | 0.7% |
Note. m/d – missing data; n/d – not determined.
First, it was examined whether pre-surgery education had an impact on the patient's ability to handle a stoma independently.
Table 3. Relationship between pre-surgery education and ability to handle a stoma
| Pre-surgery education | Total | ||||||
| Yes | No | ||||||
| N | % | N | % | N | % | ||
| The ability to handle a stoma on the first day after discharge from the hospital | Yes | 54 | 64.3% | 34 | 51.5% | 88 | 59 |
| No | 30 | 35.7% | 32 | 48.5% | 62 | 41 | |
| Total | 84 | 100 | 66 | 100 | 150 | 100 | |
Next, the link between post-surgery education and the ability to handler a stoma was tested.
Table 4. Relationship between post-surgery education and ability to handle a stoma
| Post-surgery education | Total | ||||||
| I was given comprehensive information | I have received partial information | ||||||
| N | % | N | % | N | % | ||
| The ability to handle a stoma on the first day after discharge from the hospital | Yes | 61 | 71.8% | 27 | 46.6% | 88 | 62 |
| No | 24 | 28.2% | 31 | 53.4% | 55 | 38 | |
| Total | 85 | 100 | 58 | 100 | 143 | 100 | |
A detailed analysis by Z-test for column proportions, with Bonferroni correction, showed that those who reveived comprehensive information were more likerly to be able to take care of their stoma (71.8%), compared to those who received partial information (46.6%). Among those who were unable to perform stoma care on their own, 53.4% received partial information and 28.2% received comprehensive information.
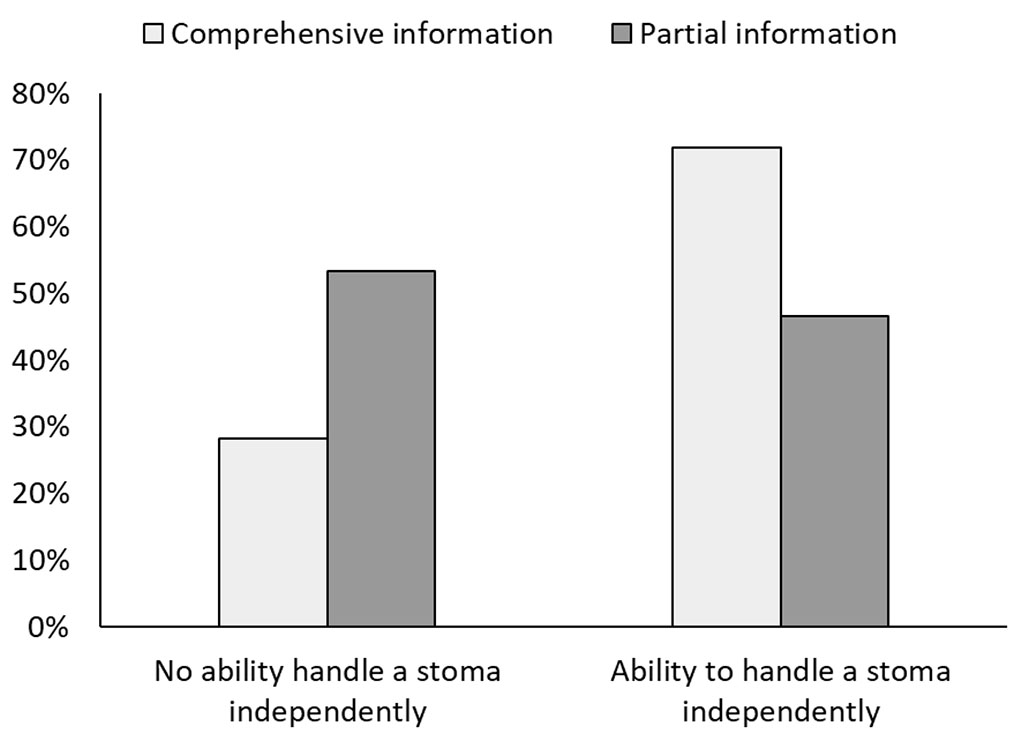
Figure 1. Relationship between post-surgery education and ability to handle a stoma
In the next step, the relationship between preoperative education and the occurrence of complications after stoma emergence was tested.
Table 5. Link between pre-surgery education and complications after stoma emergence
| Complications after stoma emergence | Pre-surgery education | ||||
| Yes | No | ||||
| N | % | N | % | ||
| Peristomal abscess | 2 | 2.41 | 0 | 0.00 | |
| No complications | 25 | 30.12 | 18 | 27.27 | |
| Peristomal hernia | 12 | 14.46 | 6 | 9.09 | |
| Prolapse of the stoma | 3 | 3.61 | 5 | 7.58 | |
| Retraction of the stoma | 3 | 3.61 | 4 | 6.06 | |
| Narrowing of the stoma | 1 | 1.20 | 7 | 10.61 | |
| Bleeding from the stoma | 15 | 18.07 | 12 | 18.18 | |
| Stool retention | 1 | 1.20 | 0 | 0.00 | |
| Inflammatory changes of the skin around the stoma | 48 | 57.83 | 35 | 53.03 | |
The analysis showed no relationship between preoperative education and complications after stoma emergence, χ2(9) = 11.92, p = .218, Vc = .25.
Next, the relationship between postoperative education and the occurrence of complications after stoma emergence was tested.
Table 6. Link between post-surgery education and complications after stoma emergence
| Complications after stoma emergence | Post-surgery education | |||
| I was given comprehensive information | I have received partial information | |||
| N | % | N | % | |
| Peristomal abscess | 0 | 0.00 | 2 | 3.45 |
| No complications | 35 | 41.67 | 6 | 10.34 |
| Peristomal hernia | 6 | 7.14 | 12 | 20.69 |
| Prolapse of the stoma | 5 | 5.95 | 3 | 5.17 |
| Retraction of the stoma | 3 | 3.57 | 2 | 3.45 |
| Narrowing of the stoma | 1 | 1.19 | 7 | 12.07 |
| Bleeding from the stoma | 11 | 13.10 | 15 | 25.86 |
| Stool retention | 1 | 1.19 | 0 | 0.00 |
| Inflammatory changes of the skin around the stoma | 40 | 47.62 | 38 | 65.52 |
A detailed analysis by Z-test for column proportions, with Bonferroni correction, showed that those received comprehensive information were more likely to report no complications (41.67%) compared to those who received partial information (10.34%). Among those who received partial information, there were more cases of peristomal hernia (20.69% vs. 7.14%), narrowing of the stoma (12.07% vs. 1.19%) and inflammatory changes of the skin around the stoma (65.52% vs. 47.62%).
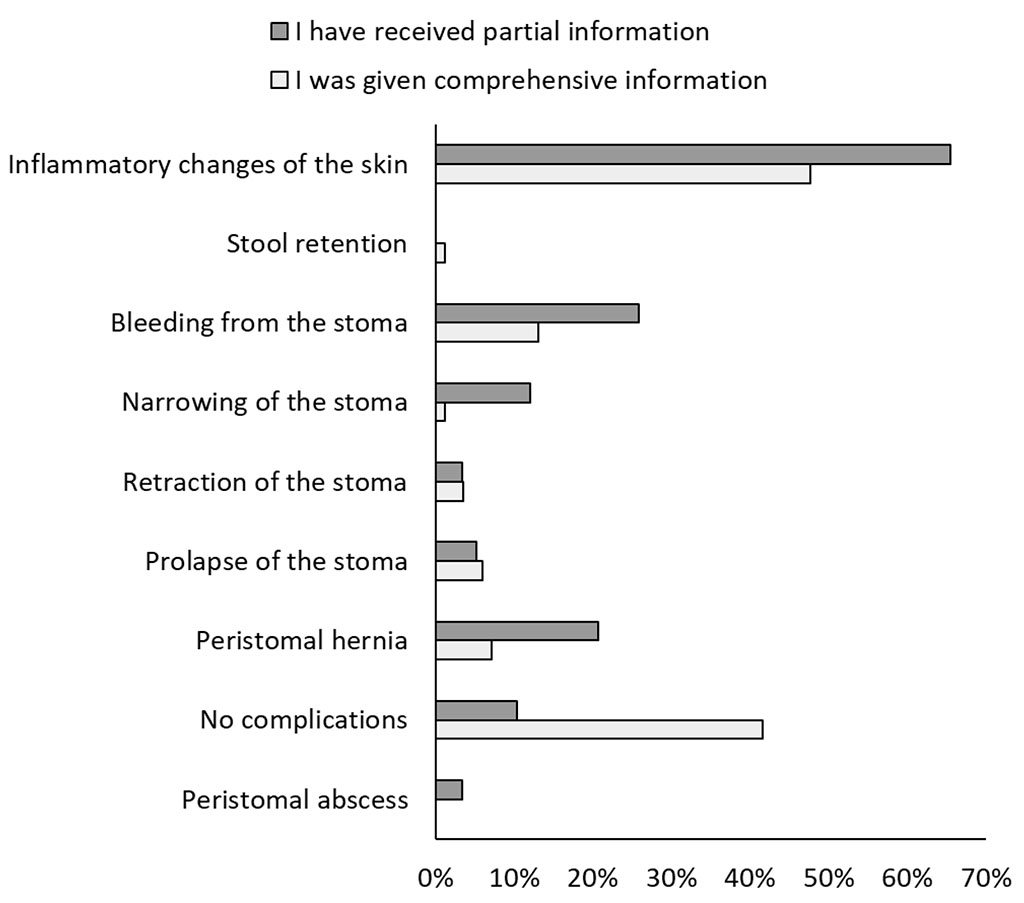
Figure 2. Link between post-surgery education and complications after stoma emergence
First, it was examined whether the use of counselling from a psychologist or psycho-sexologist had an impact on sexual functioning in women and their body image.
Table 7. Comparison of body image scores and sexual functioning - females
| Variable | Specialized help |
No
specialized help |
U | Z | p | r | ||
| Mdn | Mrank | Mdn | Mrank | |||||
| Sexual functioning | 18.1 | 34.78 | 21.8 | 42.78 | 455.00 | -1.27 | .203 | 0.14 |
| Sexual attractiveness | 40.0 | 70.00 | 41.0 | 75.37 | 1380.00 | -0.56 | .574 | 0.05 |
| Weight concern | 29.0 | 66.21 | 30.0 | 76.10 | 1289.00 | -1.04 | .300 | 0.09 |
| Physical condition | 28.5 | 66.81 | 31.0 | 75.99 | 1303.50 | -0.96 | .337 | 0.08 |
Note. Mdn - median, Mrank – mean rank, U – M-W test statistic, Z – Z test statistic, r – effect size.
Next, it was examined whether the use of counselling from a psychologist or psycho-sexologist had an impact on sexual functioning in men and their body image.
Table 8. Comparison of body image scores and sexual functioning - males
| Variable | Specialized help |
No
specialized help |
U | Z | p | r | ||
| Mdn | Mrank | Mdn | Mrank | |||||
| Sexual functioning | 6.5 | 29.19 | 8.0 | 35.76 | 197.50 | -0.89 | .374 | 0.11 |
| Physical attractiveness | 30.0 | 24.88 | 33.0 | 36.33 | 163.00 | -1.52 | .128 | 0.18 |
| Upper body strength | 26.5 | 25.19 | 29.0 | 36.29 | 165.50 | -1.47 | .141 | 0.18 |
| Physical condition | 35.5 | 25.69 | 40.0 | 36.22 | 169.50 | -1.40 | .162 | 0.17 |
Note. Mdn - median, Mrank – mean rank, U – M-W test statistic, Z – Z test statistic, r – effect size.
The next step examined whether there were differences in sexual functioning between men and women due to the use of stoma clinics.
Table 9. Comparison of sexual functioning between groups – stoma clinic services
| Variable | Using services | Not using services | U | Z | p | r | |||
| Mdn | Mrank | Mdn | Mrank | ||||||
| Sexual functioning - females | 20.9 | 38.73 | 22.1 | 43.11 | 730.50 | -0.84 | .403 | 0.09 | |
| Sexual functioning - males | 7.5 | 35.64 | 7.0 | 34.21 | 564.50 | -0.30 | .763 | 0.04 | |
Note. Mdn - median, Mrank – mean rank, U – M-W test statistic, Z – Z test statistic, r – effect size.
The analysis showed no difference between the groups in sexual functioning of females (p = .403, r = 0.09) and males (p = .763, r = 0.04).
The body image scores of men and women was then analysed according to the use of stoma clinics.
Table 10. Comparison of body image between groups – stoma clinic services
| Variable | Using services | Not using services | t | df | p | d | ||
| M | SD | M | SD | |||||
| Sexual attractiveness (F) | 42.11 | 8.55 | 40.23 | 8.66 | 1.32 | 146 | .188 | 0.22 |
| Weight concern (F) | 30.97 | 6.78 | 28.73 | 8.03 | 1.84 | 146 | .068 | 0.30 |
| Physical condition (F) | 30.41 | 7.66 | 29.55 | 7.79 | 0.68 | 146 | .497 | 0.11 |
| Physical attractiveness (M) | 36.08 | 7.62 | 32.81 | 8.06 | 1.73 | 67 | .088 | 0.42 |
| Upper body strength (M) | 31.05 | 6.92 | 28.90 | 8.81 | 1.14 | 67 | .260 | 0.27 |
| Physical condition (M) | 40.63 | 8.94 | 38.03 | 10.16 | 1.13 | 67 | .262 | 0.27 |
Note. M - mean, SD – standard deviation, t – test statistic. df – degrees of freedom, d – Cohen's d effect size.
There was also no significant difference between the groups in terms of male sexual functioning (p = .088, d = 0.42), upper body strength (p = .260, d = 0.27) and physical condition (p = .262, d = 0.27).
In the next step of the analysis, it was examined what kind of problems in the functioning of stoma clinics, patients mentioned most often.
Table 11. Most frequently mentioned problems related to stoma clinics
| Problems | % | f | fe | R | SR |
| Lack of counseling provided by a psycho-sexologist | 9.2% | 21 | 32.7 | -11.7 | -2.0 |
| Not enough home visits provided by a stoma nurse | 12.7% | 29 | 32.7 | -3.7 | -0.6 |
| No information about the existence of stoma clinics | 14.4% | 33 | 32.7 | 0.3 | 0.0 |
| Untrained staff | 10.5% | 24 | 32.7 | -8.7 | -1.5 |
| Problems with stoma equipment | 7.4% | 17 | 32.7 | -15.7 | -2.7 |
| Limited working hours of stoma clinics | 14.8% | 34 | 32.7 | 1.3 | 0.2 |
| Lack of stoma clinics locally | 31.0% | 71 | 32.7 | 38.3 | 6.7 |
| Total | 100.0% | 229 |
Note. f – observed count; fe – expected count, R - residuals, SR – standardized residuals.
The analysis showed that some of the responses were mentioned significantly more often than others, χ2(6) = 59.34, p < .001, Vc = .21. Analysis of standardized residuals showed that the problem of lack of stoma clinics locally was mentioned significantly more often than expected (SR = 6.7, 31% of responses). In addition, among the responses that were indicated less frequently than expected were lack of counselling provided by a psycho-sexologist (SR = -2.0, 9.2% of responses) and problems with stoma equipment (SR = -2.7, 7.4% of responses). The remaining responses were within the expected frequencies.
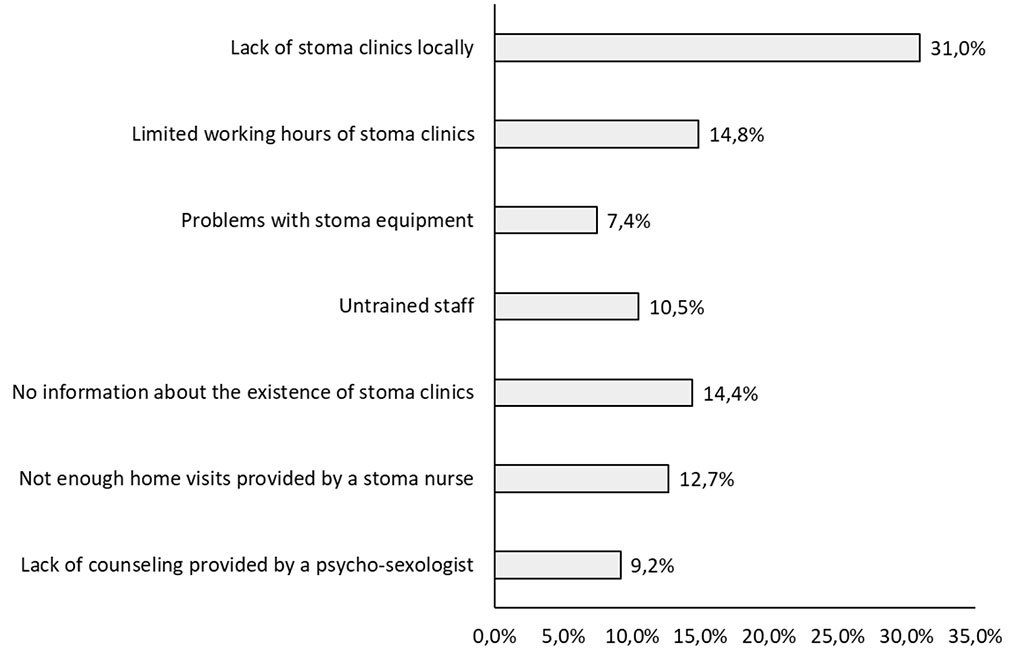
Figure 3. Most frequently mentioned problems related to stoma clinics
Next, it was examined what kind of help patients expected the most from stoma clinics.
Table 12. Forms of help expected the most from stoma clinics
| Forms of help expected | % | f | fe | R | SR |
| Getting information on how to deal with complications | 27,0% | 73 | 54,0 | 19,0 | 2,6 |
| Home visits by a stoma nurse | 15,6% | 42 | 54,0 | -12,0 | -1,6 |
| Support from a psycho-sexologist | 13,3% | 36 | 54,0 | -18,0 | -2,4 |
| Learning how to care for a stoma (performing irrigation) | 18,9% | 51 | 54,0 | -3,0 | -0,4 |
| Assistance in selecting appropriate equipment | 25,2% | 68 | 54,0 | 14,0 | 1,9 |
| Total | 100,0% | 270 |
Note. f – observed count; fe – expected count, R - residuals, SR – standardized residuals.
The analysis showed that some of the responses were mentioned significantly more often than others, χ2(4) = 19.15, p = .001, Vc = .13. Analysis of standardized residuals showed that the response: “getting information on how to deal with complications” was mentioned significantly more often than expected (SR = 2.6, 27% of responses). In addition, among the responses that were pointed less frequently than expected was support from a psycho-sexologist (SR = -2.4, 13.3% of responses) The remaining responses were within the expected frequencies.
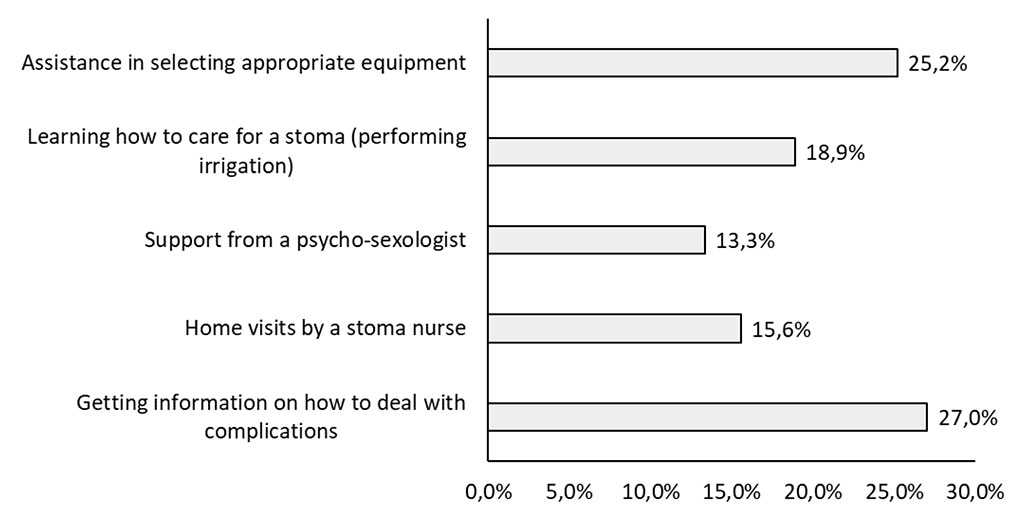
Figure 4. Forms of help expected the most from stoma clinics
The research presented by Forsmo et al. has shown that peri-operative education is an essential element, leading to increased self-management of the patients' stoma and increased life satisfaction. Therefore, the stoma education of patients in the immediate post-operative period, while still in hospital, should be an essential activity of the medical staff in order to help them to accept life with a stoma [8].
Nurses should be involved in both the pre-operative and post-operative education process for patients with a stoma. In the pre-operative phase, they inform the patient about changes in body image and give lifestyle advice. In the immediate post-operative period, nurses can impart knowledge about stoma care, proper diet, clothing choices and strategies for coping with complications [9]. Numerous studies have shown that peri-operative education improves the quality of life of stoma patients, increases stoma knowledge and the ability to manage complications [10-13].
Although pre-operative education is important for recovery, it does not replace the intensive post-operative period aimed at preparing the patient for stoma self-management. Pre-operative education should form the basis of stoma knowledge, but it is the post-operative education in hospital that is actually the final exam for the patient before being discharged home [14].
The analysis also confirmed that those who received comprehensive information on stoma care in the post-operative period were more likely to be able to manage their stoma, compared to those who did not receive complete education during this period.
According to the recommendations of the Wound, Ostomy, and Continence Nurses Society (WOCN), prior to hospital discharge, patients need to: acquire skills related to skin care around the stoma, empty the bag, change the bag, correctly select the stoma appliance, familiarise themselves with dietary and hydration guidelines, and familiarise themselves with the most common stoma-related complications [15]. Based on the ERAS protocol (enhanced recovery after surgery), patients should complete at least two stoma bag changes by the third or fourth day after surgery [16].
In practice, educational guidelines are often an unachievable standard. After stoma surgery, both doctors and nurses most often focus on the pathology present or pain control. Furthermore, given the prevalence of minimally invasive surgical techniques, hospital stays are shortened, limiting the patient’s education process [17]. Unfortunately, many stoma nurses are forced to limit patient education to a minimum of knowledge, such as how to empty a bag, without considering other important skills. Despite these shortcomings, hospital-based stoma education still plays a key role in the care of new stomas.
Despite advances in stoma surgery, post-operative complications occur in up to 30% of cases [18]. Krishnamurty et al. showed that complications, which include stoma necrosis and peristomal abscess, often occurred within 30 days of surgery [19]. Complications involving the skin around the stoma are the most common problems encountered in patients with an intestinal stoma, with an estimated incidence of 75% [20].
There is little research on the effect of stoma education on early stoma complications, such as dermatitis. In their study, Hignett et al. observed that reinforcing education on stoma management and care can effectively reduce stoma complications [21]. In order to minimise the incidence of post-operative complications and reduce the risk of hospital readmissions, it is important to support patients in developing stoma care skills themselves and learning how to select appropriate stoma care products. A key activity of medical staff, especially stoma nurses, should be to educate patients, especially in the post-operative period while still in hospital, to help them accept life with a stoma and to promote self-care. Patient education is an important route to achieving stoma-related self-efficacy, which has been shown to improve stoma acceptance and quality of life [22].
An analysis showed that patients who received comprehensive information in the post-operative period about stoma care and management were less likely to report complications compared to those who received partial information. Among those who did not receive thorough and detailed instructions during hospitalisation, there were more cases of complications such as peristomal hernia, stoma stenosis and skin inflammation around the stoma. A study by He et al. [23] also confirmed that post-operative education of stoma patients had a significant effect on reducing skin complications in the early post-operative period. Similar findings in their study were presented by Monteiro et al., and they observed a positive effect of education in the post-operative period in people with an intestinal stoma in the following aspects: knowledge, life satisfaction, length of hospitalisation, body image, quality of life, self-care skills and incidence of complications [24].
There are studies that report a reduction in the rate of complications among patients who have received pre-operative education [25-27]. However, in our analysis, there was no effect of pre-operative education on the risk of stoma complications. Even though this study included a large number of patients, it may not have been comprehensive enough in relation to the research question. It should also be noted that pre-operative education aims to explain the concept of a stoma and make preparations, e.g. marking the stoma site before surgery, but it is post-operative education that draws attention to stoma-related knowledge and nursing skills. However, it is reasonable to emphasise the fact that both forms of education are supplementary and have a beneficial effect on later life with a stoma.
Having a stoma generates psychological and physiological problems related to sexuality, which negatively affects maintaining healthy sexual relationships [28]. The majority of changes in sexual behaviour of stoma patients are caused by the stoma surgery and/or chemotherapy and radiotherapy. Surgery and complementary therapy can damage the abdomino-pelvic nerves and cause sexual problems, including: decreased libido, painful intercourse, erectile dysfunction and vaginal dryness in women [29,30]. Stoma worsens the patient's body image. In addition, the presence of a stoma bag, leakage of faecal contents, unpleasant odour and loss of control over excretion make the patient feel unsafe. Patients perceive that they are no longer desirable sexual partners and avoid sexual contact, leading to frigidity between partners and reduced quality of sexual life [31].
In the study conducted, there was no evidence of an impact of the use of psychological or psychosexual counselling on the body image and sexual functioning of patients with an intestinal stoma. This may be due to the fact that only patients with a stoma took part in the study. It seems reasonable in the future to expand the study and to invite the patients' partners to participate as well. Indeed, the Rees study showed that psychosexual counselling directed at both patients and their partners was effective in resolving patients' sexual problems and had a positive effect on their satisfaction with sex life [32].
Another point of the study was to determine what kind of post-hospital care (stoma care clinics) patients most expect and what problems they see with the functioning of such facilities. So far, there is little literature on stoma care clinics, but the importance of this form of post-hospital care for people with an intestinal stoma is great. A noticeable improvement in the quality of life in patients using stoma care clinics was observed in a study from Montreux. Patients' quality of life was shown to improve significantly if they had access to specialised care for 3 to 6 months after surgery [33]. The stoma care clinics facilitate the patient's adaptation to their new life with a stoma and, most importantly, their individual physical needs are met in a supportive environment and with the support of professional medical staff. Stoma care clinics are a significant element in the structure of the support system for patients with a stoma.
In the study carried out, it was observed that patients most expect support from the stoma care clinic in dealing with stoma complications (27%) and assistance in selecting appropriate stoma care products (25.2%). On the other hand, the most common problems related to the functioning of stoma care clinics were identified by patients as the lack of stoma care clinics in their place of residence (31%), limited working hours of the clinics (14.8%) and lack of information about the existence of such clinics (14.4%). Based on the results, it can be concluded that the availability of post-hospital care in the form of stoma care clinics is very important to patients and can make a significant contribution to improving their functioning. The analysis shows that complications from an intestinal stoma are the most common and distressing problem faced by patients after stoma surgery. As peri-operative re-hospitalisation rates due to stoma complications are high, which impairs the functioning of medical facilities, it is reasonable to pay particular attention to the provision of post-hospital stoma care in the form of stoma care clinics. This form of health care planning will not only ensure continuation of treatment but also reduce the costs associated with repeated hospitalization due to stoma complications. Although ostomy clinics are undoubtedly extremely valuable, future research that further demonstrates their importance is warranted.
There are some limitations to this research. Data were collected using cross-sectional analysis, which did not capture changes in patient experiences over time. The use of longitudinal studies would allow for a more dynamic and detailed understanding of how the quality of sex life patients with a stoma changed over time.
Additionally, the study should be expanded to include information related to the manner in which perioperative education was conducted. In the study, postoperative education had an impact on the incidence of stoma complications and the ability to care for the stoma, but the importance of preoperative education was not observed. It is therefore important to understand how the method of education (time devoted to education, methods used) influences subsequent results related to complications and the ability to independently manage the stoma.
Finally, sexual functioning is also influenced by the patient’s spouse/significant other. The study did not include patients' partners, which is another limitation. Insofar as sexual functioning encompass a wide spectrum of physiological, biological and psychological processes, and are impacted by dynamics within the relationship, we believe that the psychosocial functioning of the patient’s partner should also be assessed. It is reasonable to expand the research by including the patient's spouse.
As a result of the creation of a stoma, there is a loss or reduction in the ability to store gastrointestinal contents and a loss of ability to control excretion. Self-image, living situation, self-esteem and self-acceptance are all altered.
Perioperative education helps patients adapt to life with a stoma, improving their quality of life and reducing complications and hospital readmissions. It is an important pathway to achieving independence related to stoma care. An analysis showed that patients who received comprehensive information in the post-operative period about stoma care and management were less likely to report complications. Among those who did not receive thorough and detailed instructions during hospitalisation, there were more cases of complications such as peristomal hernia, stoma stenosis and skin inflammation around the stoma.
In the study conducted, there was no evidence of an impact of the use of psychological or psychosexual counselling on the body image and sexual functioning of patients with an intestinal stoma. This may be due to the fact that only patients with a stoma took part in the study. It seems reasonable in the future to expand the study and to invite the patients' partners to participate as well.