- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2023. 13; 5: e1. DOI 10.35630/2023/13/5.510
The article presents and analyzes the effect of combined therapy of atorvastatin and essential phospholipids in patients with rheumatoid arthritis (RA) and lipid metabolism indicators in non-alcoholic fatty liver disease (NAFLD). We examined and treated 77 RA patients with NAFLD (64 women (83.1%) and 13 men (16.9%)), under the age of 55 years old. The patients were divided into 3 groups. Additionally to RA antirheumatic therapy, the first group (n=25) received atorvastatin, the second group (n=26) - essential phospholipids, and the third group (n=26) - a combination of atorvastatin and essential phospholipids for 6 months. Assessment of the state of lipid metabolism was carried out by studying the laboratory indices of a lipid profile. A hypolipidemic effect was revealed when using both atorvastatin and essential phospholipids in patients with RA NAFLD, which increases with their combined use. Whereas the levels of total cholesterol, triglycerides (TG), low-density lipoprotein (LDL) cholesterol, and very-low-density lipoprotein (VLDL) cholesterol levels in the blood serum significantly decrease with a simultaneous increase in the content of high-density lipoproteins (HDL) cholesterol. We revealed pronounced hypolipidemic and hepatoprotective effects in RA patients with NAFLD due to combined use of atorvastatin and essential phospholipids.
Keywords: rheumatoid arthritis, nonalcoholic fatty liver disease, lipid metabolism disorders, dyslipidemia, atorvastatin, essential phospholipids
Rheumatoid arthritis (RA) is the commonest form of inflammatory polyarthritis with a population prevalence up to 1%. [3, 6, 10]. With the participation of a cascade of pathogenetic changes, processes are involved in the development of RA, which aggravate the course of the disease and are characterized by immunoinflammatory lesions of internal organs [1, 4, 12].
RA is one of the most common and disabling systemic diseases of the connective tissue. The development of inflammatory processes in the body of RA patients leads to disorders of lipid metabolism [7]. Proinflammatory cytokines are directly related to changes in blood lipid profile, which supports the concept of the role of chronic inflammation in the development of dyslipidemia [13]. These changes will contribute to the development of fatty liver infiltration in the form of steatosis [5, 14].
In addition to disease-modifying antirheumatic therapy for the treatment of RA patients with combined non-alcoholic fatty liver disease (NAFLD), it is possible to recommend the use of lipid synthesis blockers - statins, because in addition to cholesterol-lowering properties, statins, in particular atorvastatin, exert many pleiotropic effects, including anti-inflammatory and antithrombotic effects [14].
When prescribing pharmacotherapy to patients with RA, one should not forget that NAFLD increases the risk of developing hepatotoxic effects of drugs that cannot be prescribed in patients with RA. It has been established that with the development of NAFLD, the activity of enzymes that participate in the metabolism of drugs and ensure the detoxification function of the liver - cytochrome P450, glutathione transferase - decreases [5, 8]. This fact can reduce the tolerability and effectiveness of drugs prescribed for the RA treatment. Therefore, the relevance of the problem of choosing an effective and safe therapy for this category of patients is obvious, especially in cases of prescribing drugs for a long period of time.
The aim of the study was to evaluate the effect of the combined therapy of atorvastatin and essential phospholipids on the change in lipid metabolism indicators in patients with rheumatoid arthritis and non-alcoholic fatty liver disease.
For the study we selected 77 patients with RA with a chronic course of the disease and diagnosed with NAFLD, under the age of 55 years old, who signed the patient's consent to participate in the study. RA was diagnosed according to ARA criteria (1987); patients with hepatitis, alcohol abuse, >55 years old were not included. An ultrasound research method was used to assess the hepatobiliary system and an assessment of laboratory biochemical indicators of blood was carried out.
All patients were divided into three groups. All patients continued to receive RA antirheumatic therapy. The first group consisted of 25 RA with NAFLD patients (21 women (84%) and 4 men (16%)), who additionally received atorvastatin in a daily dose of 10 mg in the evening for 6 months. The second group consisted of 26 RA with NAFLD patients (22 women (84.6%) and 4 men (15.4%)), who additionally received essential phospholipids at a dose of 600 mg (two capsules) three times a day for 6 months. The third group consisted of 26 RA with NAFLD patients (21 women (80.8%) and 5 men (19.2%)), who, in addition to RA antirheumatic therapy, received essential phospholipids at a dose of 600 mg (two capsules) three times a day and atorvastatin at a daily dose of 10 mg for 6 months.
Statistical analysis was performed using program Statistica. The reliability of differences was defined at p <0.05.
The analysis of the results of lipid metabolism showed that in all studied groups of patients with RA and NAFLD, a proatherogenic serum lipid profile was observed, which was expressed by a reduced level of HDL-cholesterol, a high level of TG, LDL-cholesterol, and VLDL-cholesterol. Presumably, the accumulation of fat in the liver can be an independent factor of dyslipidemia and indicates the possible presence of a direct pathogenetic chain: liver steatosis - dyslipidemia - atherosclerosis. Changes in the lipid profile in blood serum may indicate metabolic disorders, changes in the quantitative and qualitative composition of lipids in the liver, and atherogenic dyslipidemia in patients with RA and NAFLD, in turn, is the most important risk factor for the development and progression of cardiovascular pathology.
The use of atorvastatin in patients of the I group leads to an increase in HDL-cholesterol to the level of 1.33±0.128 mmol/L (Fig. 1) and a decrease in LDL cholesterol to a level of 3.16±0.470 mmol/L (Fig. 2).
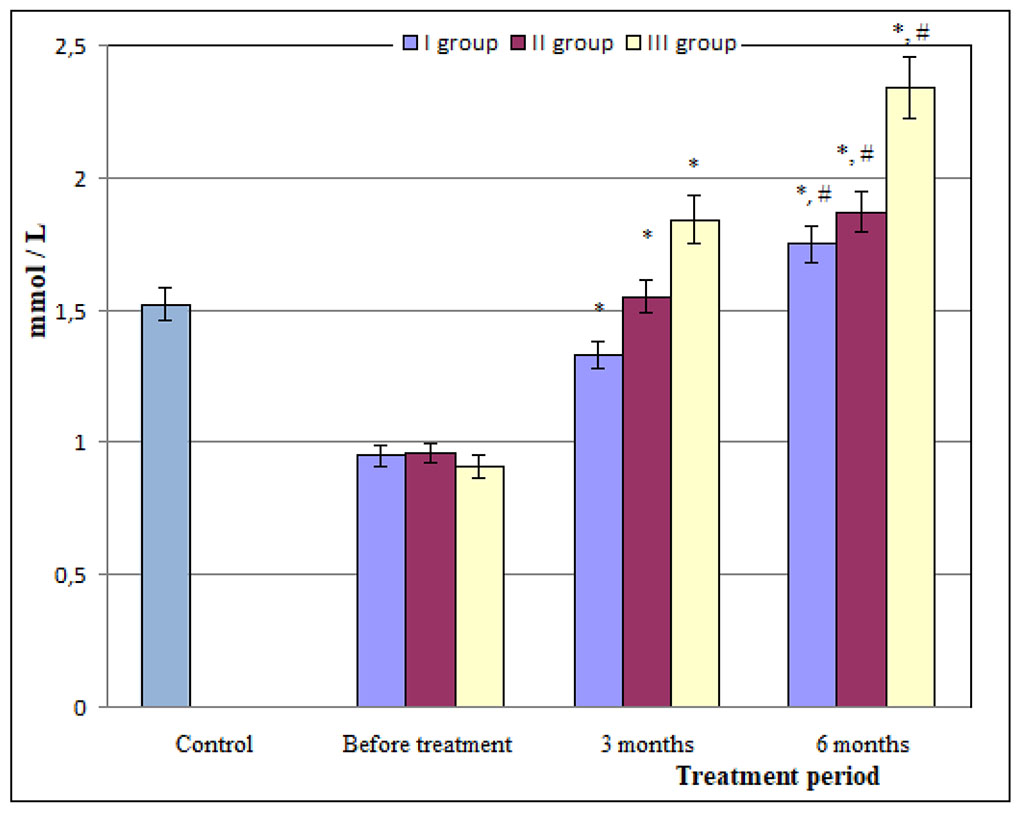
Figure 1. The content of HDL-cholesterol in the blood serum of patients with RA and NAFLD under the effects of atorvastatin and essential
phospholipids
* – statistically significant difference with
indicators characteristic before the treatment, p<0.05; # –
statistically significant difference according to the indicators
observed after 3 months of treatment, p<0.05
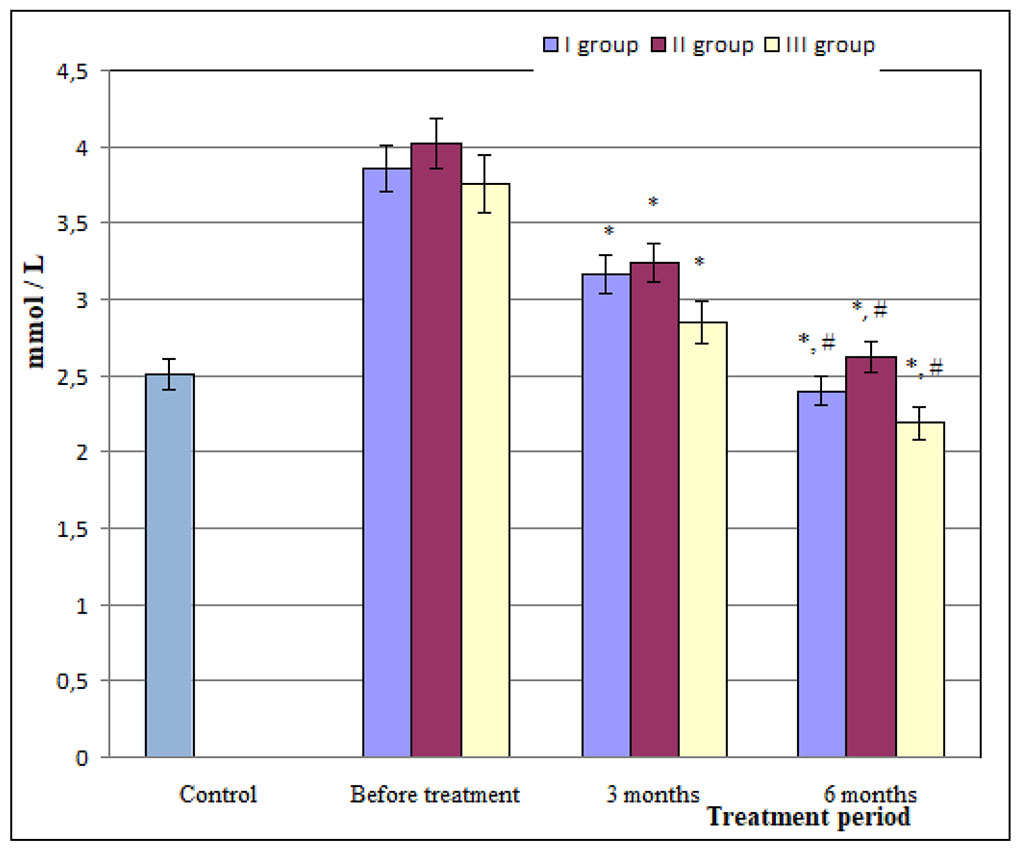
Figure 2. The content of LDL-cholesterol in the
blood serum of patients with RA and NAFLD under the effects of
atorvastatin and essential phospholipids
* – statistically significant difference with indicators
characteristic before of treatment, p<0.05; # – statistically
significant difference according to the indicators observed after 3
months of treatment, p<0.05
Antiatherosclerotic changes are indicated by a decrease in the atherogenicity index until 3.03±0.549 (Table 1). At the same time, the total cholesterol, TG, VLDL-cholesterol levels in the blood serum decreases. However, the studied indicators are at the level of the upper limit of the norm, which indicates the need for further treatment in this category of patients (Table 1).
Table 1. Indicators of lipid metabolism in the blood serum in patients with RA and NAFLD under the effects of atorvastatin and essential phospholipids, M±m
Treatment period |
The investigated indicator | |||
| Total cholesterol, mmol / L | TG, mmol / L | VLDL cholesterol, mmol / L | Atherogenicity index | |
| І group (n=25) | ||||
| Before treatment | 7.66±0.651 | 2.37±0.132 | 0.94±0.091 | 5.09±0.882 |
| After 3 months | 5.29±0.416* | 1.78±0.234* | 0.79±0.05* | 3.03±0.549* |
| After 6 months | 4.82±0.287*, # | 1.49±0.338*, # | 0.67±0.015*, # | 1.76±0.204*, # |
| ІІ group (n=26) | ||||
| Before treatment | 6.89±0.831 | 2.69±0.121 | 0.92±0.081 | 5.11±0.631 |
| After 3 months | 5.62±0.331* | 1.85±0.163* | 0.73±0.034* | 2.63±0.286* |
| After 6 months | 4.56±0.295*, # | 1.40±0.128*, # | 0.61±0.052*, # | 2.41±0.264* |
| ІІІ group (n=25) | ||||
| Before treatment | 7.34±0.531 | 2.93±0.221 | 0.96±0.071 | 5.23±0.337 |
| After 3 months | 4.77±0.305* | 1.54±0.336* | 0.69±0.051* | 1.75±0.072* |
| After 6 months | 4.21±0.287*, # | 1.25±0.272*, # | 0.56±0.024*, # | 1.54±0.114*, # |
* – statistically significant difference with indicators characteristic before of treatment, p<0.05; # – statistically significant difference according to the indicators observed after 3 months of treatment, p<0.05
Correction of the lipid profile of the blood with lipid metabolism indicators approaching the norm is observed 6 months after the start of treatment (Fig. 1, Fig. 2, Table 1). Obviously, the decrease in the concentration of total cholesterol and LDL cholesterol in the blood serum is related to the mechanism of action of atorvastatin, which, by inhibiting HMG-CoA reductase, reduces the biosynthesis of cholesterol in the liver. In addition, under the action of atorvostatin, the number of liver LDL receptors on the surface of cells increases, which leads to increased uptake and catabolism of LDL, which is manifested by a decrease in LDL cholesterol and VLDL cholesterol in blood serum.
Similar to atorvastatin, essential phospholipids have a corrective effect on the state of lipid metabolism. Thus, already 3 months after their use in patients of the II group, the content of LDL cholesterol decreases by 19.4% (Fig. 2), the level of total cholesterol decreases by 18.4%, the level of TG by 31%, and by 20.7% - the content of VLDL cholesterol (Table 1) with a simultaneous increase in the level of HDL cholesterol by 61.9% (Fig. 1) compared to the indicators observed in patients of the II group before treatment (p<0.05). 6 months after the additional introduction of essential phospholipids to the RA treatment scheme, their hypolipidemic effect is even more significant, as the level of total cholesterol decreases by 66.2%, the level of TG - by 52%, and the content of VLDL cholesterol - by 66.3% (Table 1) , the content of LDL - by 65.2% (Fig. 2) (р<0.05), along with this, the level of HDL cholesterol increases by 94.8% (Fig. 1) compared to the indicators observed in patients of the II group before treatment (р<0.05). It should be noted that both after 3 months and after 6 months, the atherogenicity index decreases by 1.7 and 2.9 times, respectively, compared to the indicators observed in patients of the II group before treatment (р<0.05) (Table 1).
The results show that essential phospholipids have a significant antiatherogenic effect. This established fact may be related to the direct or indirect effect of essential phospholipids on the process of lipogenesis in the liver, in particular on SREBP-1 (sterol regulatory element binding protein-1). It is known that SREBP-1 is a hepatocyte transcription factor that ensures the synthesis and control of lipogenesis enzymes, in particular acetyl-CoA-carboxylase, fatty acid synthase [2]. In addition, essential phospholipids can affect nuclear receptors that control TG metabolism, synthesis and catabolism of lipids in the liver, namely: PPARs (peroxisome proliferator-activated receptors), FXR (farnesol X receptor), LXR (liver X receptor), HNF -4α (hepatocyte nuclear factor-4α) [9]. In particular, under the action of essential phospholipids, PPAR-α activity can increase and microsomal, mitochondrial and peroxosomal oxidation of fatty acids - the main substrate of TG - can be activated. PPARs activate lipoprotein lipase, which ensures TG hydrolysis [9]. Under the action of essential fatty acids, the activity of SREBP-1 can decrease and, as a result, the processes of lipogenesis are inhibited due to the reduced synthesis of fatty acids by hepatocytes.
It is believed that phospholipids are able to modify HDL cholesterol by affecting the fluidity of their lipids and the transport of cholesterol inside these particles, as a result of which the removal of cholesterol from cells is facilitated, the normal level of total cholesterol in the blood is maintained and an antiatherogenic effect is realized. In addition, it is known that essential phospholipids inhibit the activity of HMG-CoA reductase, which significantly affects the synthesis of cholesterol, reducing its amount. The unidirectional effect of atorvastatin and essential phospholipids on the parameters of the blood lipid profile that we found prompted us to study their combined effect in RA with NAFLD patients.
The results of the studies showed that the most pronounced hypolipidemic effect is observed with the combined use of atorvastatin and essential phospholipids (group III) compared to their separate use (group I and group II). It was established that already 3 months after the combined administration of these medicines in patients of the III group, all the investigated indicators approached the norm. Thus, the level of total cholesterol decreased to 4.77±0.305 mmol/L, TG to 1.54±0.336 mmol/L, VLDL cholesterol to 0.69±0.051 mmol/L (Table 1), LDL cholesterol to 2.85±0.104 mmol /L (Fig. 2). At the same time, the content of HDL cholesterol in blood serum increased to the value of 1.84±0.043 mmol/L (Fig. 1), as a result of which atherogenicity index decreased to the level of 1.75±0.072 (Table 1). During the six-month combined use of atorvastatin and essential phospholipids, the hypolipidemic effect increased (Fig. 1, Fig. 2, Table 1), which indicates the effectiveness of the treatment regimen proposed by us. Therefore, both atorvastatin and essential phospholipids, when administered to patients with RA and NAFLD, have a pronounced hypolipidemic effect, which increases with their combined use, since the levels of total cholesterol, TG, LDL cholesterol, and VLDL cholesterol in the blood serum significantly decrease with a simultaneous increase in the content of HDL cholesterol. The corrective effect of the combined use of atorvastatin and essential phospholipids that we have established can have a positive effect on the functional state of the liver.