- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 5: e1. DOI 10.35630/2199-885X/2022/12/5.4
Using the method of immune histochemistry, the qualitative and quantitative features of gender hormone receptors in the structure of the mucous membrane epithelium of woman cervix in the postmenopausal period were studied and its relationship with the proliferative activity of keratinocytes was explored. The significance of estrogen deficiency in proliferative activity in the epithelial structure of the mucous membrane of the cervix in the postmenopausal period is shown. Additional targets for therapeutic action have been identified in order to regulate and normalize proliferative activity and prevent neoplasia and malignancy in the structure of the cervical epithelium. It has been established that the most variable indicators are in the structure of the mucous membrane of the exocervix, and the most stable - in the endocervix. A promising direction in predicting disruptions of intercellular interactions leading to malignancy in the structures of the mucous membrane of the cervix in postmenopausal women is the standardization of Ki-67 assessment against the background of indicators of the level of estrogen and progesterone reception in the system of differons of the epithelial layer.
Keywords: cervical mucosa, postmenopause, malignancy, hormone receptors, estrogens, progesterone, proliferation.
According to WHO data, up to 500,000 new cases of cervical cancer are registered annually and about 240,000 women die from cervical cancer every year. This formidable statistics determines the relevance of research in this direction and dictates the need for a detailed and deeper study of the epithelium covering the cervix [13]. WHO is developing a strategy to end cervical cancer as a global public health problem that proposes a reduction in mortality to four per 100,000 women, with double cervical screening, early diagnosis and treatment of pre-invasive lesions and invasive cancer up to 90% [3, 14]. Serious disorders in the body of postmenopausal women are accompanied by severe clinical manifestations, including not only vegetative-vascular disorders, but may also be accompanied by malignancy in the cervical mucosa (CM) [2, 9, 11]. The individual characteristics of postmenopausal women require the development of personalized methods for monitoring patients with a severe course of the postmenopausal period and a deep analysis of the causes of disturbances in the system of regulation of cell proliferative activity in the structure of epithelial differons [8, 13]. Li Z., Lin Y., Cheng B., Zhang Q., Cai Y. (2021) and Lin S., Gao K., Gu S., (2021) sure that there are no perfect models for comparative analysis [7, ten]. Despite the fact that the activity of reception to sex hormones is well studied by Ahn K.H., Kim H.Y., Cho G.J. (2020) in experimental animals, and Punnonen R., Lukola A. in women in the reproductive period, this issue in vivo in the postmenopausal period is practically not resolved [1, 12], which determined the choice of the direction of our research. The question of the paracrine regulatory interaction of hormone-positive cells and proliferation in the MC, which is observed in the endometrium of the uterus in animal models, has also not been sufficiently studied.
The aim of the research was to study the characteristics of the sex hormones receptors and their role in the proliferative activity of keratinocytes in the postmenopausal period. In this regard, the following tasks were set:
1. to establish the features of estrogen and progesterone reception in the cells of the epithelial cover of the cervical mucosa (CM) in the postmenopausal period. 2. To study the proliferative activity in the structures of cervix depending on changes in estrogen and progesterone reception in the CM.
Biopsy specimens of the mucous membrane of the cervix of 149 patients with severe postmenopausal period were taken in the ecto-, endocervix and at the place of transition of the ectocervix to the inner part of the cervix in accordance with the order of the Ministry of Healthcare of the Russian Federation dated April 29, 1994 N 82 "On the procedure for conducting pathological studies" and in accordance with the nomenclature of methods for clinical laboratory diagnostics of the Ministry of Health of the Russian Federation (order No. 64 of February 21, 2000). As a control, were used the materials of tissue sections of the cervical cancer and endometrium in 15 women over 50 years old with a favorable menopausal history and in the postmenopausal period who underwent diagnostic hysterectomy for a benign and non-inflammatory cause. The general morphological picture was obtained using the method of staining with hematoxylin and eosin. Immunohistochemical methods for detecting the cellular nuclear antigen Ki-67, as well as for the receptors for sex hormones in human CM were performed according to standard protocols. The number of expressed cells was counted per 100 cells in each section using the morphometric software of an Olympus BX52 microscope.
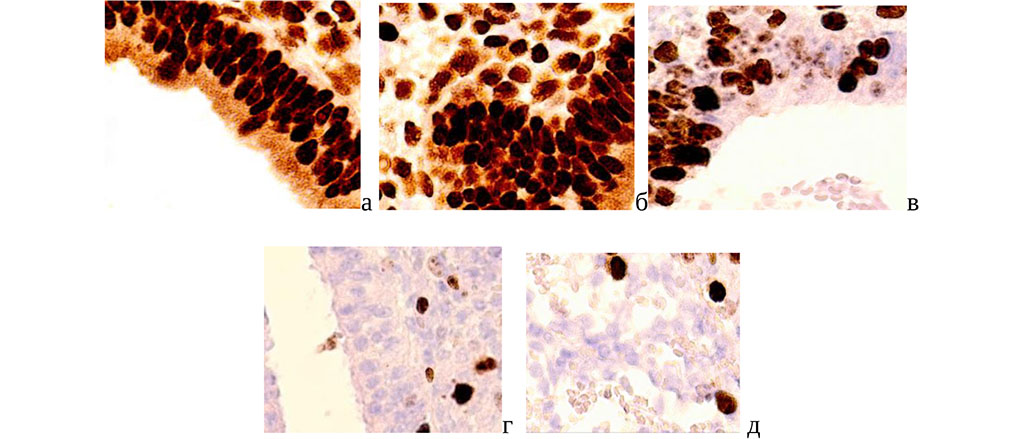
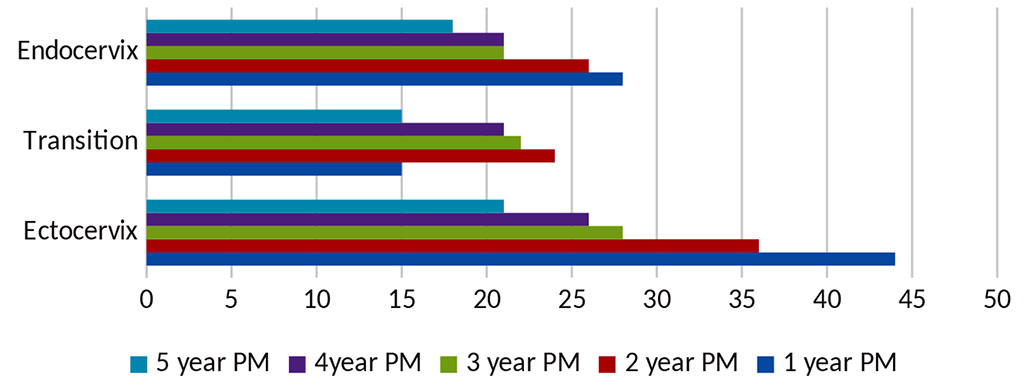
In postmenopausal women in CM with a severe course of the postmenopausal period, an increased level of progesterone receptors was noted against the background of a sharp decrease in the detection of estrogen receptors in the cylindrical epithelium, both in daughter and reserve cells, as well as in the underlying connective tissue compared to material of women with a normal course of post menopause (Fig. 1).
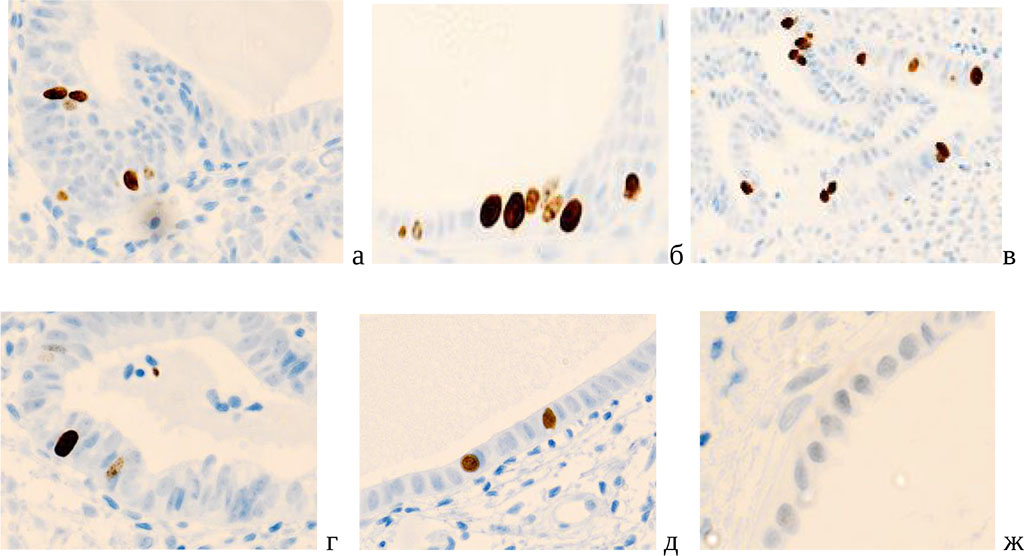
Figure 1. Cervical mucosa of postmenopausal women. A, b) with a severe course; c, d) with a normal course. Immune histochemistry to detect the localization of receptors for sex hormones with additional staining with hematoxylin. (a, b, c – progesterone receptors; d, e – estrogen receptors). Magnification x400.
Also in postmenopausal period, there is an increase in the activity of progesterone receptors with a simultaneous decrease in the level of estrogen and is associated with the dynamics of proliferative activity in the epithelial plate of the MC. At the same time, there is a statistically significant excess of all indicators in women with a severe course of the postmenopausal period. For greater clarity, these data are presented in diagrams (Fig. 2, 3, 4, 5).
Figure 2. Quantitative characterization of progesterone-positive cells in the norm in the cervix mucous membrane in postmenopausal women.
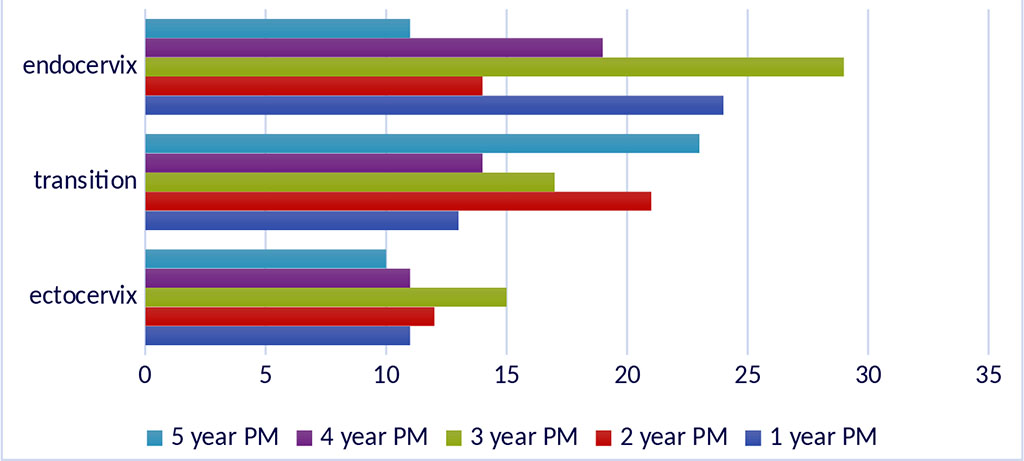
*Note - PM-postmenopause
Figure 3. Quantitative characteristics of progesterone-positive cells in cervix mucous membrane in the pathology postmenopausal.
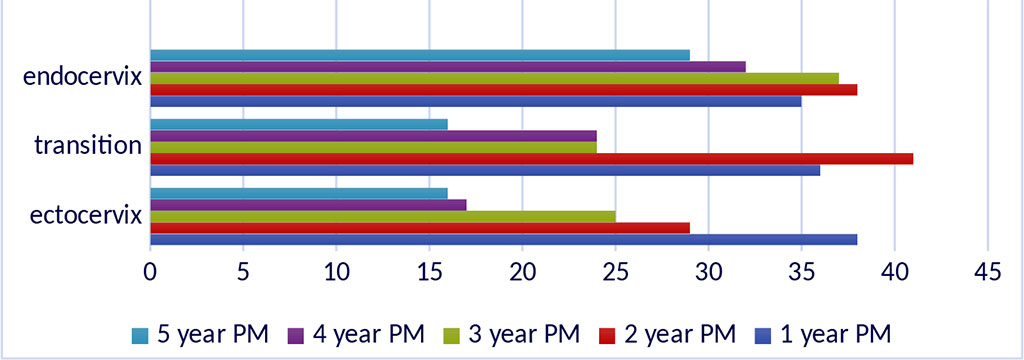
*Note - PM-postmenopause
Figure 4. Quantitative characterization of estrogen-positive cells in cervix mucous membrane in the postmenopausal women in normal conditions
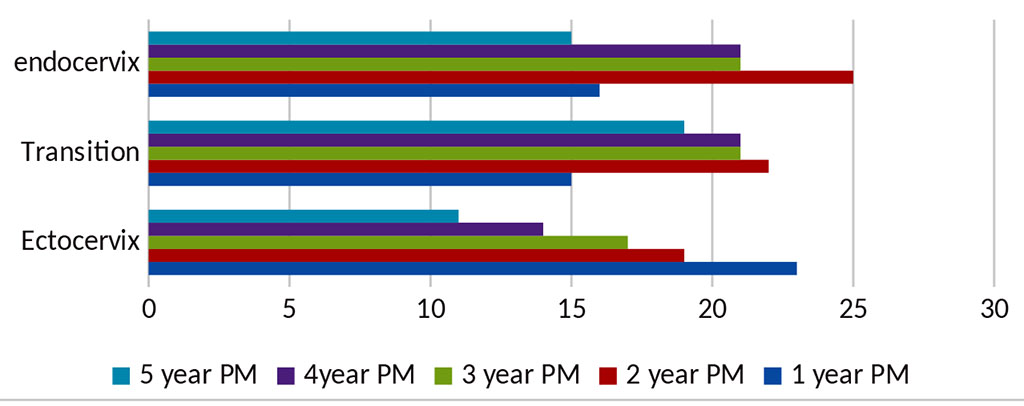
*Note - PM-postmenopause
Figure 5. Quantification of estrogen-positive cells cellsin cervix mucous membrane postmenopausal women with pathology.
*Note - PM-postmenopause
The analysis of proliferative activity in different periods of post-menopause in women had differences in different departments of the CM (Fig. 6).
Figure 6. Cervical mucosa of a 54-year-old woman. Immune histochemistry to detect the localization of the Ki-67 gene protein with hematoxylin staining. Microphoto. Magnification A, c) x 200; b, d, e, g) x400.
The number of Ki67-positive cells during developing pathology in the postmenopausal period increases to a greater extent in the CM of the exocervix compared to the norm, which can be associated with contamination of pathogens and adaptive desquamation of the epithelium on the surface of the epithelium, these data are presented in the diagram (Fig.7, 8).
Figure 7. Diagram of proliferative activity in the MOS of postmenopausal women in the norm.
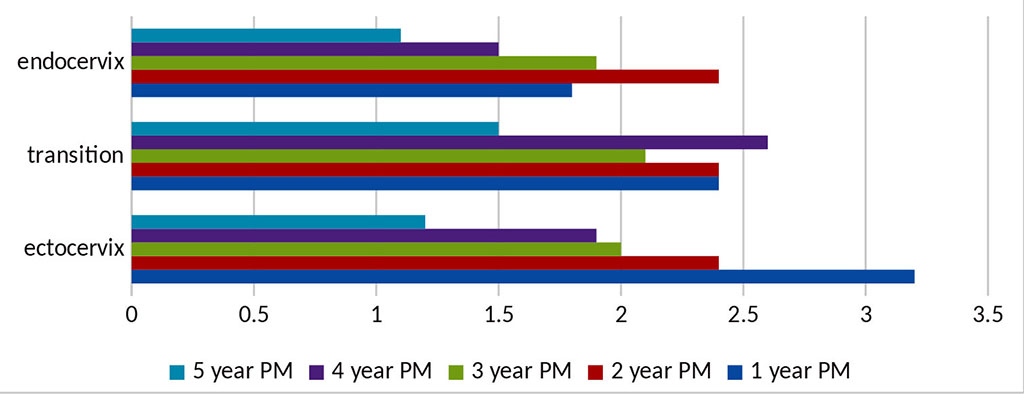
*Note - PM - postmenopausal period
Figure 8. Diagram of proliferative activity in pathology in the mucous membrane of the cervix of postmenopausal women.
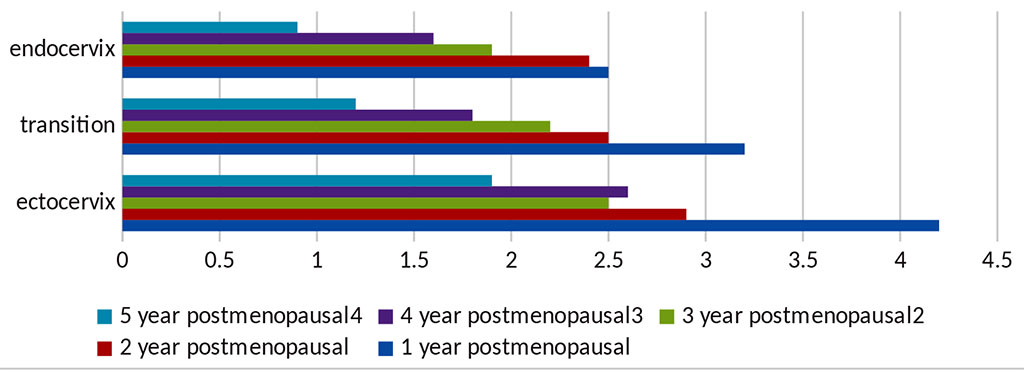
*Note - PM - postmenopausal period
According to the obtained data, in norm, proliferative activity is highest in the exocervix in the first year of postmenopause and at the site of the transition of the exocervix to the endocervix in the 1st, 2nd, and 4th years of postmenopause. It is these years that can be considered critical in terms of the greatest load on the epithelium of the transitional zone of the CM for the control of proliferation in postmenopausal patients. An increase in proliferative activity in the epithelial layers of the CM for the 5th year of the postmenopausal period leads to the depletion of the regenerative potential and a decrease in the barrier properties of the integumentary epithelium. This indicates a violation not only in the reproductive system of postmenopausal women, but also in the organs of central regulation, causing intense pronounced changes in target organs. Friedrich M., Mink D., Villena-Heinsen C., et al. (1998), Li Y., Shoyele O., Shidham V.B. (2020) noted that the currently used Pap smear staining in postmenopausal women for the differential diagnosis of cervical atrophic processes and high-grade intraepithelial neoplasia (CIN2-3) gives a correct assessment only in 87%, in 13% it is represented by false positive results [ four]. Screening with a Pap smear or biopsy / curettage, according to Lashmanova N., Braun A., Cheng L., (2021), has variable efficiency, sometimes the error reaches 50% [6]. Gupta R., Sodhani P., Mehrotra R., Gupta S. (2019) indicate diagnostic errors in 20.4% of cases and propose to solve morphological problems in the interpretation of pathology using more wide and detailed research spectra [5].
Thus, the analysis of the expression of cell sex hormone receptors in postmenopausal women showed that in the normal course of postmenopause in a comparative aspect with a complicated course, all indicators in various departments of the CM are exceeded. A group of patients with increased expression of receptors for sex hormones and high proliferative activity of the CM structures in postmenopause is a risk group and needs a special examination to clarify the hormonal activity of the ovaries, determine the level of estrogen receptors not only in the blood, but also during diagnostic extirpations for the purpose of timely morphological monitoring and prevention of malignancy. Recommendations for the appointment of targeted hormone replacement therapy within the framework of the principles of maximum oncological vigilance should be based on a comprehensive morphological basis, not only on the state of activity of estrogen and progesterone-positive cells-targets of the CM, but also their ratio to the indicators of the number of proliferating cells. Therefore, the expansion of the diagnostic resource based on methods for detecting sensitivity to sex hormones and the proliferative activity of the CMepithelium in postmenopausal women is becoming increasingly important in monitoring for the prevention of malignancy.
Presented data can be used as a model for a comparative analysis in the prognostic plan for the clinical assessment of abnormalities in the proliferation system and receptor sensitivity to sex hormones of the epithelial cells of the CM in postmenopausal women, as well as for making decisions in the development of a strategy and individual planning of conservative and surgical treatment.
