- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 5: e1. DOI 10.35630/2199-885X/2022/12/5.18
The study involved an analysis of the data gum biopsies obtained through light microscopy and polarization microscopy in order to identify pathomorphological features and the collagen Type I & Type III ratio in 56 children with occlusion issues, periodontal diseases and various undifferentiated connective tissue dysplasia (UCTD). 32 healthy children with intact periodontium served as a control group. For the histological examination of gum biopsies, the respective sections were stained with hematoxylin and eosin, while Picro-Sirius Red Stain Kit reagents were used to assess the Type I and Type III collagen distribution in the gum connective tissue. The image processing was performed in the ImageJ 1.47 software, while when analyzing the color histograms, the ratio of the red pixels (Type I collagen) and the green pixels (Type III collagen) was identified. The Type I/III collagen ratio (1.41±0.09) in children with chronic catarrhal gingivitis, occlusion issues and a “prominent” degree of UCTD was found to be significantly lower (p≤0.05) the similar ratio observed in patients with clinically healthy periodontium (2.01±0.09), as well as in patients with “mild” and “moderate” UCTD (1.63 ± 0.17) with homogeneous clinical and morphological dental manifestations. The effectiveness of the developed comprehensive dental treatment program for periodontal issues in children with abnormal occlusion associated with UCTD, including conservative anti-inflammatory treatment, pharmacological correction and orthodontic treatment, is justified by an increase in the amount of mature Type I collagen, a decrease in the developing immature Type III collagen, and inflammation in the periodontal tissues. A sufficient degree of maturity and differentiation of connective tissue was also achieved.
Keywords: connective tissue dysplasia, inflammatory periodontal disease, dental anomaly, polarization microscopy, Type I collagen, Type III collagen, morphological studies.
Numerous research papers are focused on undifferentiated connective tissue dysplasia (UCTD), which due to its high prevalence causes a significant risk of developing multiple organ pathology. There is clinical evidence pointing at the fact that an increase in the UCTD signs falls on the “critical” period of the child’s physical evolution (age of 11-15) due to the active growth phase, whereas the “immaturity” of connective tissue leads to morphological and functional issues affecting organs and body systems, while contributing to the development of secondary (associated) pathological conditions, including those involving the dental system [7,24,37].
The level of dental health is an overall health status indicator for the entire body, so a high incidence of dental issues (25.2%-84.3%) in childhood points at the need for an in-depth study of the etiopathogenesis of orthodontic nosological forms, which, in turn, is to help develop effective diagnostic algorithms and optimal tactics to treat occlusion disorders [14,18,22,26,30,36,46].
The connective tissue system, which is decisive for the functional and morphological integrity of the body, has a role in the development of most maxillofacial structures, while children with dysplastic disorders feature a high prevalence of dental anomalies, carious and non-carious lesion of teeth, periodontium and temporomandibular joint [1,3,5,44].
There is scientific evidence proving that most periodontal tissues (gum, periosteum, bone tissue of the well and of the alveolar process, the periodontium ligament system) have connective tissue origin, and dysplastic changes (hemorrhagic syndrome; microcirculatory disorders; insufficiency of nonspecific resistance mechanisms; failure of bone, muscle and fibrous structures) intensify inflammation and destructive pathological processes, affect negatively reparative and physiological regeneration mechanisms, and slow down bone remodeling. This pathogenetic complex develops ground for an early onset of periodontium issues, facilitates their progression, chronic course with a high rate of exacerbations, while conventional dental measures employed to treat patients with periodontal diseases associated with connective tissue dysplasia do not allow arriving at immediate and long-term outcomes of periodontal treatment [8,21,52].
The main goal in clinical practice is to ensure the quality and a long-term positive treatment outcome for major dental diseases [2,10-13,20,23,27-29,39,47-51].
The current stage of progress in certain sections of clinical dentistry reveals a significant increase in the role of anthropometric, morphological, radiological, laboratory diagnostic and functional research methods when it comes to solving the most urgent issues. In periodontology, in particular, a combined use of clinical and paraclinical research methods allows objective diagnostics and developing a strategy for comprehensive treatment of impairments affecting periodontal tissue [6,15-17,19,25,31-34,41-43,45].
Collagen structures, as well as the mature Type I collagen VS. immature Type III collagen (I/III) ratio, play a special role when it comes to studying the morphology of periodontal tissues in patients with UCTD. The prevalence of Type III collagen development speaks of incomplete elimination of inflammation, which leaves the maturation of connective tissue incomplete [4,9,35,38,40].
A thorough study of pathomorphological features, as well as the collagen I/III ratio, viewed as an informative biomarker in children with UCTD and periodontal pathology, allows detecting the degree of connective tissue maturity, as well as identifying systemic dysplastic disorders through its remodeling, in order to ensure grounds for personalized management tactics when dealing with this group of patients.
Aim of the study – to investigate the morphological features and the Type I to Type III collagen ratio in children with connective tissue dysplasia syndrome and periodontium issues at the stages of comprehensive dental treatment.
The inclusion criteria for the patients (n=56) in the main group were: age – 12 to 17; orthodontic pathology – abnormal ratio of dental arches (K07.2, distal bite K07.20; ICD-X); abnormal position of teeth (K07.3, crowded teeth K07.30, ICD-X), not involving tooth extraction (Degree I by N.G. Snagina); UCTD syndrome; clinical manifestations of periodontal diseases. The diagnosis was verified subject to the Russian recommendations “Hereditary and multifactorial connective tissue disorders in children. Diagnostic algorithms” (2014). The severity of the dysplastic process was assessed in view of the dysplasia diagnostic criteria of by L.N. Abbakumova (2006) and the scoring scale for assessing the significance of phenotypic signs (Table 1).
Table 1. Score assessment of phenotypic trait significance in assessing the connective tissue dysplasia severity by L. N. Abbakumova (2006)
| Sign | Score | Sign | Score |
| Eye hypertelorism | 1 | Incomplete syndactyly of 1st and 2nd toes | 2 |
| Blue sclera | 1 | Dilated capillaries of skin of face, back | 2 |
| Wide nose bridge | 1 | Scars on skin | 2 |
| Ingrown ear lobes | 1 | High palate | 3 |
| Pigmented spots | 1 | Increased skin extensibility | 3 |
| Asthenic physique | 1 | Pronounced venous skin pattern | 3 |
| Clinodactyly of little fingers | 1 | Easy development of hematomas | 3 |
| Epicanthus | 2 | Hernias | 3 |
| Saddle-shaped nose | 2 | Weakness of abdominal muscles | 3 |
| Protruding ears | 2 | Transverse striation of feet | 3 |
| Asymmetry of nasal septum | 2 | Flat feet | 3 |
| Pallor of skin | 2 | Hallux valgus | 3 |
| “Suede-like” skin | 2 | Hollow foot | 3 |
| Delicate skin | 2 | Eyesight pathology | 4 |
| Wrinkled skin | 2 | Pronounced hypermobility of joints | 4 |
| Flat chest | 2 | Kyphosis | 4 |
| Slight indentation on chest | 2 | Scoliosis | 4 |
| Clavuses | 2 | Keeled thorax | 5 |
| Sandal-shaped slit | 2 | Funnel-shaped deformation of chest | 6 |
The total score in children with a mild degree of UCTD did not exceed 12; in case of a moderate degree of CTD – 13-23, whereas cases with a prominent degree of CTD had a score of 24 or beyond. Details concerning the phenotypic manifestations of UCTD were obtained from the medical records, medical reports of respective experts, anamnestic data (anamnesis morbi, anamnesis vitae). Depending on the phenotypic manifestation severity, the children were divided into two subgroups: Subgroup 1 were children (n=29) with a mild and moderate degree of UCTD; Subgroup 2 included children (n=27) with a prominent degree of UCTD. The comparison group were children (n=32) with physiological occlusion, intact periodontium bearing no signs of CTD. Clinical and morphological studies followed the ethical principles for medical research with human beings involved, as stated by the World Medical Association Declaration of Helsinki (1964, 2000).
The periodontological and hygienic status was assessed relying on the papillary-marginal-alveolar index (PMA) (Schour, Massler 1947) modified by Parma (1960); the sulcus furrow bleeding index (SBI) (Muhlemann-Cowell, 1971); the approximal plaque index (API) (Lange, Plagmann, 1977), and the simplified Green-Vermillion oral hygiene index (OHI-S) (Green, Vermillion, 1964). The diagnosis was set based on the entire set of clinical and radiological signs, subject to the Classification of periodontal diseases (2001).
The biopsy sampling in children of the main group was performed from the gums featuring the most obvious signs of inflammation, prior to, and at the stages of comprehensive dental treatment, whereas in patients with intact periodontium – from the gums at teeth to be removed for orthodontic indications.
Morphological studies were carried out employing standard light microscopy and polarization microscopy. For standard light microscopy, soft tissue biopsies of marginal periodontal were fixed in 10% of buffered formalin, poured into paraffin, with serial histological sections (4-5 microns) prepared and stained with hematoxylin and eosin. Polarization microscopy was employed to compare the distribution of Type I and Type III collagen in the gum connective tissue using the Picro-Sirius Red Stain Kit reagent set (Connective Tissue Stain). The biopsies were fixed in a 10% neutral formalin solution. Further on, the slices (4-5 microns) were immersed for 30 minutes in a Picro Sirius staining solution (0.1% Sirius Red F3BA with picric acid pH 2), washed for 2 minutes in 0.01% N HCl, dehydrated, to be further placed in a synthetic Bio-Mount filling medium (Bio Optica Milano S.P.A.). The visualization of Type I and Type III collagen was done in polarizing light at a lens magnification (×500) with a ZEISS Axiolab 5 microscope and a ZEISS Axiocam 208 color digital video camera. The image processing was performed in the ImageJ 1.47i software (Wayne Rasband National Institutes of Health, USA). When analyzing the color histograms, the ratio of the red pixels (Type I collagen) and the green pixels (Type III collagen) was identified.
The comprehensive dental treatment offered to the patients in the main group included the following stages: Stage 1: conservative (local anti-inflammatory) measures – professional oral hygiene based on the standard method with an AIR-FLOW MASTER PIEZON multifunctional combined device (EMS). To remove the biofilm, water-soluble ultra-fine powder Air-Flow PLUS with bactericidal, antioxidant, angioprotective, antimicrobial effect was used. When finishing the teeth polishing, an angular tip (rotation speed – 5000 rpm) was used, together with Prophylaxe Master (NTI) polishing rubber heads, whereas finishing the approximal surfaces was done with fine-grained Epitex polymer strips (GC) (Fig. 1).

Figure 1. Patient S., 16 y.o. Abnormal ratios of dental arches (K07.2, ICD X); abnormal position of teeth (K07.3, ICD X) associated with CTD syndrome. The oral cavity hygienic status prior to (a) and after (b) AIR-FLOW MASTER PIEZON professional hygiene.
Stage 2: conservative (local anti-inflammatory) treatment – R.O.C.S. Jasmine flower toothpaste, Tonsinal (Saluta-M) mouthwash, CM-1 (Saluta-M) bioresorbable gelatin gum phyto-plates, for 15 days until the clinical symptoms of inflammation disappeared.
Stage 3: pharmacological correction of dysplastic disorders – collagen-preserving treatment (Vitamins B1, B2, B6; folic acid, ascorbic acid); activation of metabolic processes (L-Carnitine); improved microcirculation (Troxevazine, Trental); stimulation of connective tissue synthesis and regeneration (Theraflex ®); regulation of phosphorus-calcium metabolism (Calcium-D3 Nicomed).
Stage 4: orthodontic treatment with ligature braces (metallic – Micro Arch, Generus; sapphire – Inspire Ice; ceramic – Clarity, Clarity Advanced) and cap aligners (Invisalign, Star Smile). When the orthodontic treatment with fixed appliances was complete, a repeated course of conservative anti-inflammatory treatment was performed in order to reduce the prevalence and intensity of periodontal issues.
The value distribution normality was evaluated base on the Shapiro-Wilk W-criterion. The statistical data processing was done with the IBM SPSS Statistics 24.0 software in Windows 10, the differences being statistically significant at p<0.05
The initial level of hygiene indices in the main group (Subgroup 1: OHI-S – 1.81±0.19 and API − 46.4±2.6%; group 2: OHI-S – 2.13±0.27 and API – 51.2±2.1%) points an improper hygiene status of the oral cavity, while the oral hygiene in the comparison group corresponded to the norm indicators (OHI-S − 0.47±0.05 and API − 22.3±0.8%). The periodontal status at the initial examination in children with abnormal occlusion featured average severity of inflammation and gum bleeding (Subgroup 1: PMA – 35.87±1.14% and SBI − 2.19±0.18; Group 2: PMA – 48.61±2.34% and SBI − 2.54±0.26); during that, children with physiological occlusion has an index score of periodontal tissues (PMA − 17.82±0.35% and SBI – 0.42±0.09) within the acceptable values.
Following the completion of the comprehensive complex dental treatment in the main group, there was a significant improvement in the hygiene (Subgroup 1: OHI-S – 0.76±0.08 and API – 26.7±1.2%; Subgroup 2: OHI−S − 1.02±0.13 and API – 29.3±1.5%) and periodontal (Subgroup 1: PMA − 21.61±0.92% and SBI − 1.27±0.09; Subgroup 2: PMA − 29.84±1.09% and SBI − 1.46±0.14) status to be observed, which meant a significant decrease in the plaque biofilm development and a lower intensity of inflammatory and destructive changes in the periodontium. In the comparison group, after the preventive measures were over (OHI-S − 0.35±0.09; API − 19.2± 0.6%; PMA − 13.74±0.28%; SBI – 0.37±0.05), the dynamics in the hygiene level improvement, as well as in the periodontal tissue status – if matched against the initial data – was less prominent.
Figure 2 shows the periodontological status and the morphological picture of the gum tissue in a patient with a physiological bite and clinically healthy periodontium.
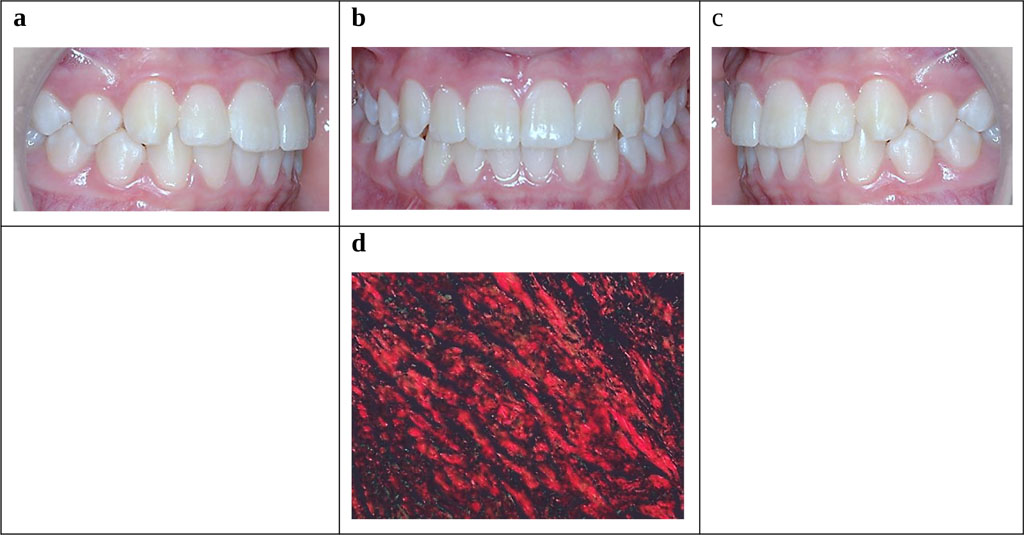
Figure 2. Patient M., 15 y.o. Clinically healthy periodontium and healthy gum (Lang, Bartold, 2018). Occlusal relationship, periodontal tissue status (a-c). Morphology of gum tissues (d) − staining with 0.1% Sirius Red F3BA solution with picric acid (×500).
Figure 3 shows the periodontological status and the occlusal relationships in a patient with abnormal dental arch ratios (K07.2; ICD-X), abnormal teeth position (K07.3; ICD-X) associated with UCTD (moderate degree).
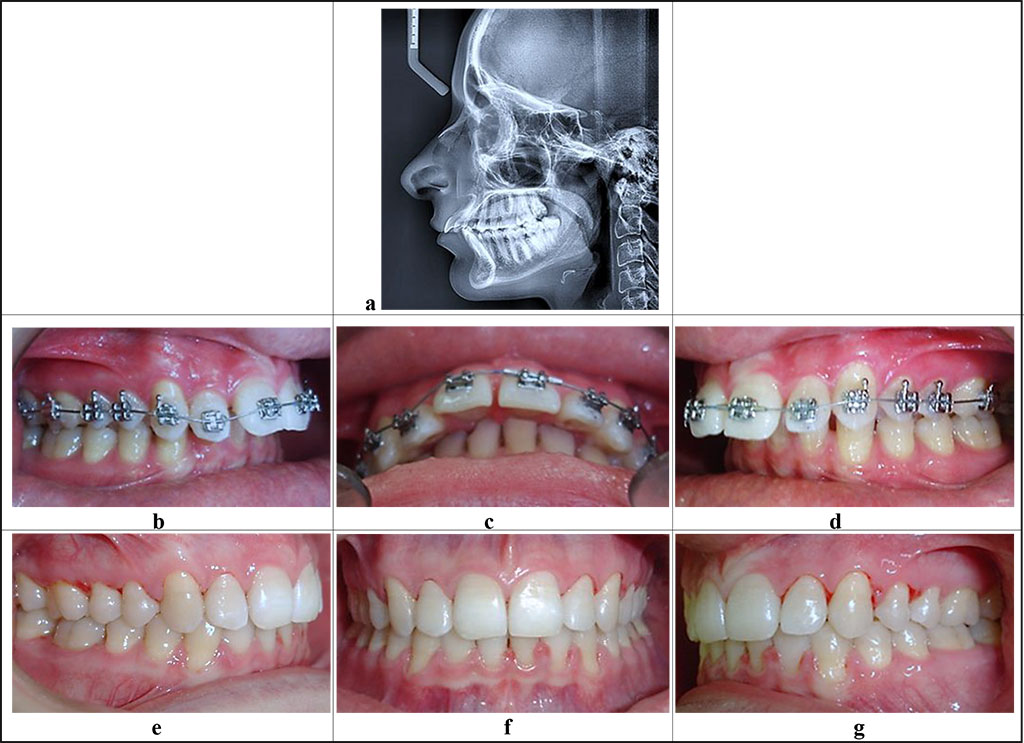
Figure 3. Patient E., 16 y.o. Diagnosis: chronic catarrhal gingivitis, moderate severity (K 05.10). Distal occlusion (closure of first molars and canines, Angle’s Class II; 07.20), protrusion of the upper front teeth. Teleroentgenogram, lateral projection (a), periodontological status and occlusive relationships prior to (b-d) and after (е-g) the orthodontic treatment.
Figure 4 shows the morphological picture of gum tissue in a patient with moderate chronic catarrhal gingivitis (K05.10) and UCTD syndrome.
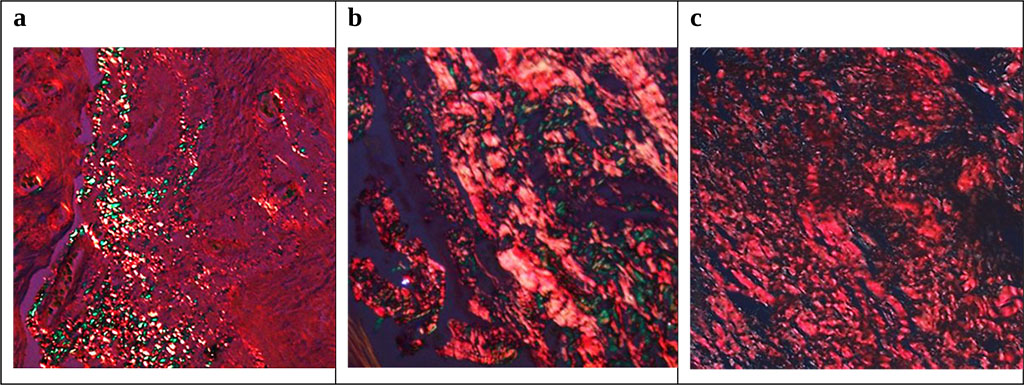
Figure 4. Morphological picture of gum tissue in patient E., 16 y.o., with chronic catarrhal gingivitis, moderate severity (K05.10): a – initial status; b – status after conservative anti-inflammatory therapy; c – status after complex dental treatment. Staining with 0.1% SiriusRed F3 BA solution with picric acid (=500).
Figure 5 shows the periodontological status and occlusal relationships in a patient with abnormal dental arch ratio (K07.2), abnormal position of teeth (K07.3) associated with CTD (severe degree).
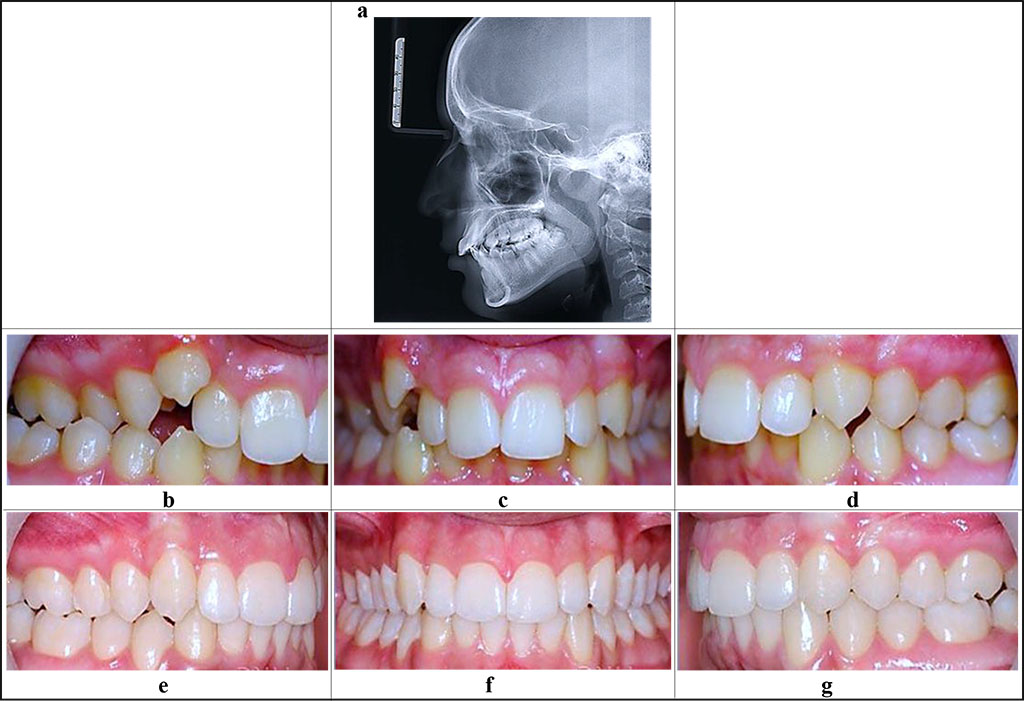
Figure 5. Patient S., 15 y.o. Diagnosis: chronic catarrhal gingivitis, moderate (K 05.10). Deep distal bite (K 07.20), cross bite on the right (K07.25), upper canine dystopia on the right (K07.3). Teleroentgenogram, lateral projection (a), the periodontological status and occlusive relationships before (b-d) and after (е-g) the orthodontic treatment.
Figure 6 shows the morphological picture of gum tissue in a patient with chronic catarrhal gingivitis of moderate severity (K05.10) and UCTD syndrome.
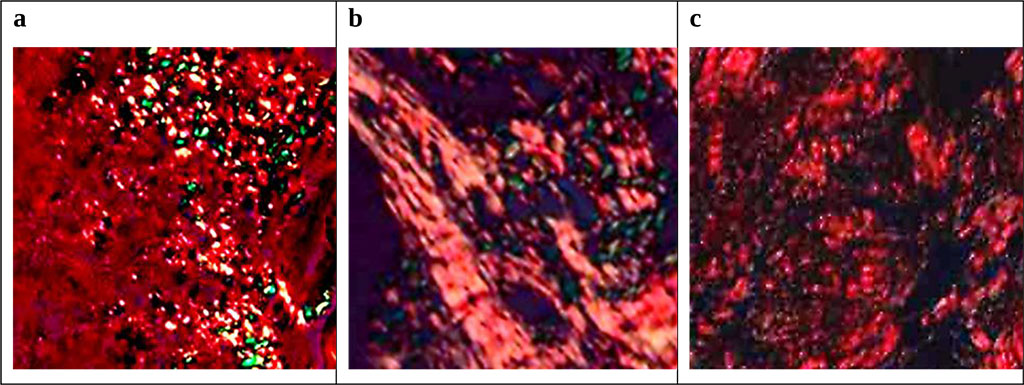
Figure 6. Morphological picture of gum tissue in patient S., 15 y.o., with deep distal bite (K07.20): a – initial status; b – status after conservative anti-inflammatory therapy; c – status following comprehensive dental treatment. Staining with 0.1% SiriusRed F3BA solution with picric acid (=500).
Table 2. Type I / Type III collagen ratio in the groups involved into the study, at the stages of dental treatment, (u), (M ± m)
| Study Groups | |||
| Comparison group | Main group 1st subgroup | Main group 2nd subgroup | |
| The initial state | 2,01 ± 0,09 | 1,63 ± 0,17 ⃰ | 1,41 ± 0,09 ⃰ |
| After conservative anti-inflammatory therapy | − |
1,79 ± 0,13 ⃰ |
1,68 ± 0,12 ⃰ |
| After complex dental treatment | − |
1,86 ± 0,11 ⃰ |
1,71 ± 0,07 ⃰ |
Note: * – statistically meaningful compared to the indicator observed in patients in the comparison group (p<0.05).
The outcomes of polarization microscopy revealed that the collagen I/III ratio in children with physiological occlusion and clinically healthy periodontium disease was 2.01 ± 0.09. The baseline values in children with occlusion issues and inflammatory periodontal pathology associated with CTD were significantly lower: in the cases of mild and moderate CTD – 1.63±0.17; at prominent CTD – 1.41±0.09. Following the first and the second stages of comprehensive dental treatment (local conservative anti-inflammatory therapy), the ratio in question in the Subgroup 1 went up by 9.8% - to 1.68 ± 0.12; in Subgroup 2 – by 19.1% – up to 1.79 ± 0.13. Following the completion of the third and the fourth stages of comprehensive dental treatment (pharmacological correction and orthodontic treatment), the increase in the collagen I/III ratio value in Subgroup 1 was 4.3% – to 1.86 ± 0.11, while in Subgroup2 it was 2.2% – to 1.71± 0.07 (Table 1). Notable is the fact that the main changes in the collagen I/III ratio in both subgroups were observed after the first and the second stages of comprehensive dental treatment, while in patients with a prominent degree of CTD, the growth rate was higher (19.1%) compared to the children with mild and moderate CTD (9.8%). The polarization microscopy data obtained through a comparative analysis of Type I and Type III collagen distribution in the gum connective tissue reveal that the comprehensive dental treatment offered to children with dental pathology associated with CTD promotes a significant increase in the collagen I/III ratio, while the values obtained did not come up to the level registered in children with physiological occlusion and clinically healthy periodontium.
Figure 7 shows the gum biopsy histological preparation in the comparison group.
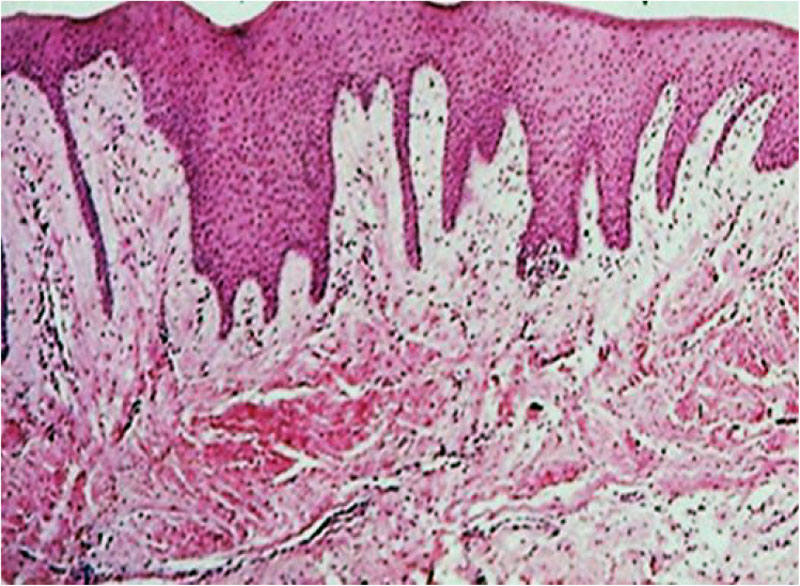
Figure 7. Gum biopsy histological preparation, a patient of the comparison group. Staining with hematoxylin-eosin (×100).
As light microscopy of gum biopsies in children belonging to Subgroup 1 show, following comprehensive dental treatment, the following histological picture was to be observed: the gum tissue was lined with a multilayer flat keratinizing epithelium with pronounced acanthosis (thickening) through proliferation of the basal and the spiny layers, as well as elongated interstitial epithelial processes; dystrophic epithelial changes; edema foci with moderate lympho-macrophage perivascular infiltrates; serous exudate (spongiosis) in the spiny layer intercellular spaces (see Fig. 8).
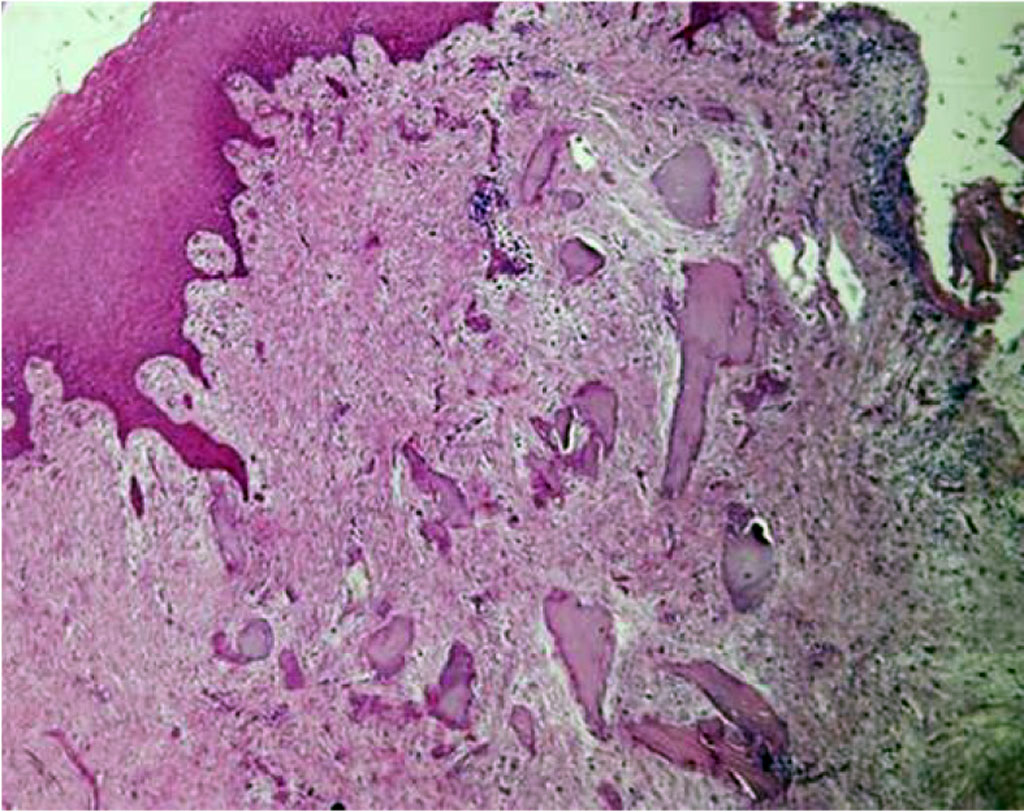
Figure 8. Gum biopsy histological preparation in a patient of Subgroup 1, following comprehensive dental treatment. Staining with hematoxylin-eosin (×100).
The light microscopy of gum biopsies performed in Subgroup 2 Following comprehensive dental treatment revealed the following histological picture: the gum tissue was lined with a multilayer flat keratinizing epithelium with moderate acanthosis and spongiosis; dystrophic epithelial changes; the papillary layer of the dermis contained a significant number of full-blooded capillaries and small focal infiltrates consisting of lymphocytes, macrophages and plasma cells; individual perivascular lympho-macrophage infiltrates (Fig. 9).
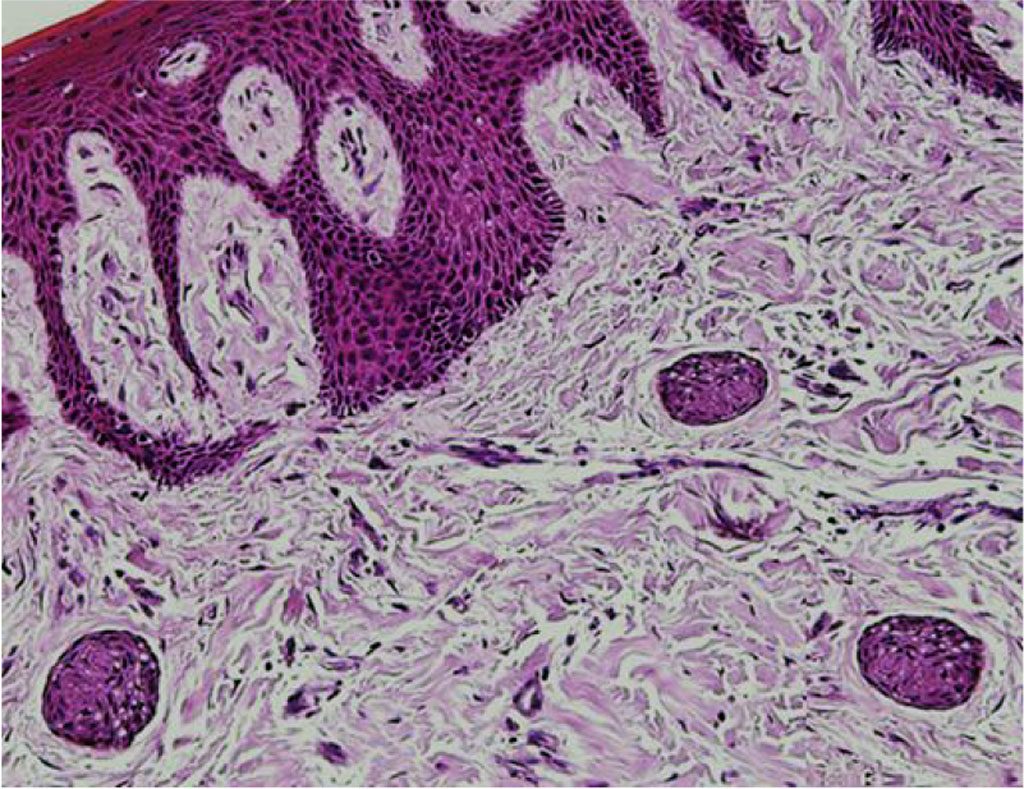
Figure 9. Gum biopsy histological preparation, patient of Subgroup 1, following comprehensive dental treatment. Staining with hematoxylin-eosin (×100).