- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 4. DOI 10.35630/2025/15/4.018
Background: Placenta accreta spectrum (PAS) disorders are characterized by abnormal placental adherence and invasion into the uterine wall. They most commonly occur in women with a history of cesarean deliveries and represent an increasingly common iatrogenic condition in modern obstetrics.
Case presentation: We report the case of a 40-year-old woman with a history of three cesarean sections, admitted at 31 weeks of gestation due to suspected PAS. Imaging confirmed placental invasion at the site of the uterine scar. At 35 weeks, due to the onset of preterm labor, a scheduled cesarean delivery was performed with preoperative placement of ureteral stents and internal iliac artery balloons. Intraoperative hemorrhage necessitated a peripartum hysterectomy. A male neonate was delivered in good condition and required only brief respiratory support.
Conclusion: This case highlights the importance of early diagnosis, imaging surveillance, and multidisciplinary planning in the management of PAS to reduce maternal morbidity. Reducing the rate of cesarean deliveries remains a key preventive strategy.
Keywords: placenta accreta spectrum, caesarean section, pregnancy, hysterectomy
Placenta accreta spectrum disorder (PAS) refers to abnormal placentas with adherence to the myometrium (placenta accreta) and different degrees of invasion into (increta) and through the entire myometrium, sometimes to adjacent pelvic organs (percreta) [1]. Recent evidence indicates that the global incidence of placenta accreta spectrum (PAS) is approximately 0.17 %, equivalent to about one in 600 deliveries, with rates rising in parallel with increasing cesarean delivery trends [2]. PAS occurs frequently as an iatrogenic complication of prior invasive gynecologic procedures, primarily caesarean sections [3]. The constantly rising number of caesarean sections causes an increase in the prevalence of PAS [4]. Incidence of PAS correlates positively with placenta previa, maternal age, multiple births, higher socioeconomic status, hypertension, use of assisted reproductive technology and female fetal sex [5]. It is essential to identify the risk factors and establish the prenatal diagnosis of PAS, as it is the most significant factor affecting outcome [6]. PAS is associated with delivery complications, frequently with a high risk of life-threatening massive obstetric haemorrhage [7]. Early detection of PAS enables one to make a delivery plan taking into account expected complications, which decreases maternal morbidity and mortality [5,8]. The most common problem related to maternal deaths is lack of experience [9]. Therefore, the patients should be hospitalized in regional centers of excellence with multidisciplinary care [10]. We present a case of a 40-year-old woman with PAS to accentuate the importance of early diagnosis and the implementation of the appropriate procedure in this increasingly occurring clinical problem. The aim of this case report is to highlight the clinical course, imaging findings, surgical management, and multidisciplinary coordination in a patient with placenta accreta spectrum after multiple cesarean sections.
In January 2023, a 40-year-old Caucasian patient at 30 weeks + 6 days of gestation was admitted to the Department of Obstetrics and Perinatology, Medical University of Lublin with suspected placenta ingrowth. The patient had been under the proper outpatient antenatal care. During the first trimester ultrasound examination, attention was already drawn to the low position of the placenta with suspected placenta ingrowth. The patient was referred to the hospital for further diagnosis and management.
The patient's previous obstetric history included 3 uncomplicated pregnancies, with term deliveries by caesarean sections. The indication for the first caesarean section was breech presentation. The second and the third caesarean section was performed due to previous operational deliveries. The woman has no addictions and suffers from varicose veins of the lower limbs, but no chronic coexisting diseases. The patient's family history is cancer-laden - her father died of gastric cancer.
In the current pregnancy, the patient attended regular antenatal visits. She did not experience any vaginal bleeding during pregnancy. The patient suffered from microcytic anemia and was started on oral iron supplementation. During hospitalization, hemoglobin level was still as low as 10.1 g/dl and in order to improve blood morphotic parameters she received an iron intravenous infusion. Ultrasound scan showed the placenta located on the posterior wall of the uterus and overlapping the right side of the uterus, partially covering the scar from the previous cesarean section. The border between the placenta and the myometrium was difficult to evaluate, which also indicated suspected placenta ingrowth into the cesarean section scar.
The pelvic MR examination performed showed the placenta located on the posterior wall of the uterus, descending low and partially covering the internal os of the cervix. The probability of the validity of the suspicion of an ingrown placenta was increased by the observation of a prominent uneven border between the placenta and the uterine muscle in the anterior part on the right side with the penetration of small villi of the placenta into the uterine muscle.
During hospitalization, conservative management was administered and fetal well-being was confirmed. The patient was given betamethasone to induce fetal lung maturity.
At 35. weeks of gestation the patient reported irregular uterine contractions. Therefore, the decision was made to terminate the pregnancy with a caesarean section. To minimize the risk of intraoperative complications special measures were taken. In the first instance, the urology team probed the patient's ureters with SJ catheters. Then the interventional radiologists inserted balloon catheters into the internal iliac arteries. The blood was cross-matched and the blood service was alerted. During caesarean section, once the uterus was exposed, the placental vessels were visualized growing through the anterior uterine wall. Placental ingrowth was noted on the right side of the previous uterine scar. After extracting the baby, the placenta was separated, but heavy bleeding was noted. Due to the ingrowth of the placenta and massive obstetric haemorrhage, the decision was made to perform a perinatal hysterectomy. During the operation, the patient was given 2 g of cefazolin, 5 units of oxytocin i.v. and 2 units of red blood cells were transfused.
The patient gave birth to a male neonate weighing 3670g and 56cm long. Apgar scale score at the 1st minute – 8 points, at the 3rd minute – 9 points, at the 5th minute – 8 points, at the 10th minute – 8 points. Due to increasing symptoms of respiratory failure (tachypnoea, respiratory effort), n-CPAP BiPhasic was applied (initially FiO2 30%, later FiO2 21%). The child required respiratory support for 4 hours. After this time, his condition stabilized and no other supportive procedures were required.
Due to a decrease in HGB values from 10.1 g/dl preoperatively to 8.1 g/dl postoperatively, the patient was transfused with another 2 units of red blood cells on the first postoperative day.
On the 10. day after the operation, the patient and her child were discharged in good condition.
The case report timeline is presented in Figure 1.
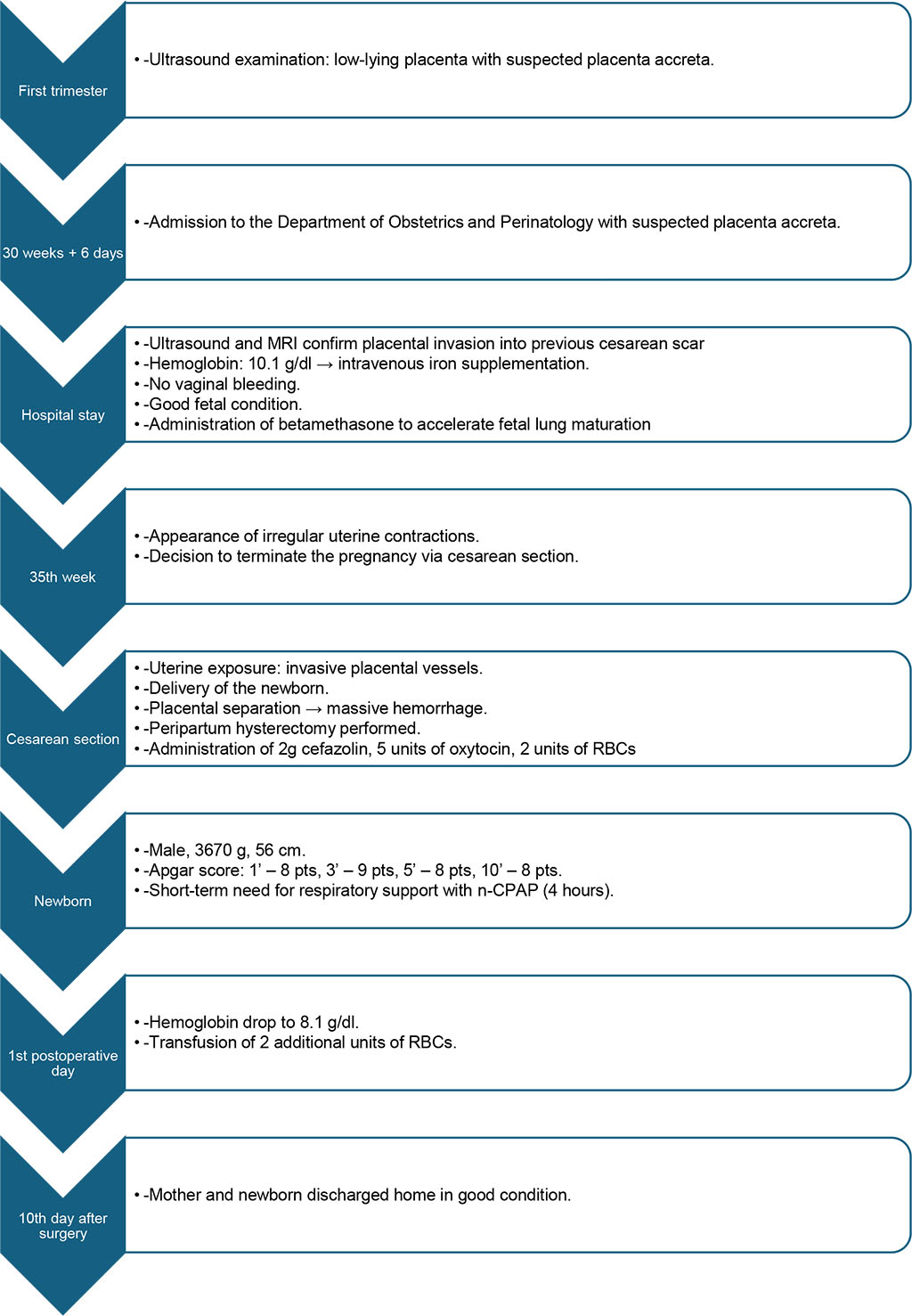
Figure 1. The case report timeline.
Placenta accreta spectrum (PAS) remains a significant clinical challenge in modern obstetrics due to its increasing incidence and associated maternal morbidity. Multiparity, placenta previa and a high number of cesarean deliveries performed are among the main risk factors for placenta accreta spectrum. According to Silver et al. (2006), the estimated risk of placenta accreta spectrum in the presence of placenta previa increases with the number of prior cesarean deliveries: approximately 11 % after one, 40 % after two, and up to 61 % after three cesarean sections [11] (Figure 2).
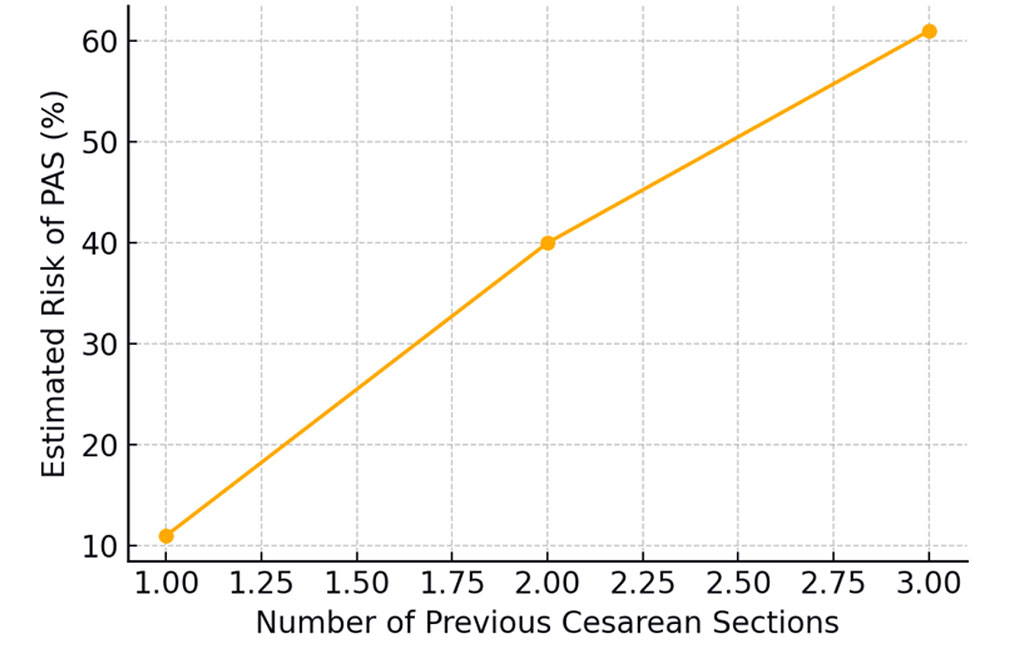
Figure 2. Risk of placenta accreta spectrum (PAS) occurrence depending on the number of previous cesarean sections.
Having considered the fact that the presented patient was 40 years old and had 3 previous cesarean deliveries, a high risk of PAS and obstetric complications could have been expected. As such it seems important to reduce the number of caesarean sections performed, as well as to educate patients about possible complications related to this procedure. This is important given the rising number of caesarean sections in many countries. The rate of caesarean section reported in the United States was 5% in 1970 and 31.9% in 2016 respectively [12].
Doppler ultrasonography and magnetic resonance imaging play a key role in the antenatal diagnosis of PAS, with characteristic ultrasound findings including placental lacunae, loss of the clear zone, thinning of the myometrium, and increased vascularity at the uteroplacental interface. Finberg et al. showed that the positive predictive value of ultrasonography was 78% and the negative predictive value was 94% [13]. However, it should be remembered that the final diagnosis can be confirmed by histopathological examination [14].
The basic treatment of placenta accreta is hysterectomy, however, conservative management of this condition was reported in the literature. Although the conservative method is distinguished by its ability to minimize blood loss and preserve fertility [15], it is noteworthy that, to date, no randomized controlled trials have been conducted to systematically compare the efficacy of both approaches. Additionally, there is a crucial need to discern the patient cohorts that stand to gain the most from this method of treatment.
The management of PAS requires careful planning with an elective caesarean section (where possible) and meticulous preparation for intraoperative complications. The need of peripartum hysterectomy should be considered to reduce the likelihood of massive haemorrhage [16]. Gestational age at delivery is a critical determinant of maternal and fetal outcomes in PAS and should be carefully individualized based on clinical stability and risk of hemorrhage. The presented patient underwent elective cesarean section delivery at 35. weeks of gestation due to the onset of preterm labour. Timely planning is also of paramount importance given the risk of bleeding after 36. weeks of gestation [17]. Antepartum bleeding may lead to maternal life-threatening complications including oligovolemic shock [18]. Appropriate planning of the procedure also requires the availability of blood products on site in the event of haemorrhage. Possible options to reduce maternal blood loss include interventional radiology procedures with internal iliac ligations. Although some studies confirm a reduction in blood loss in patients after iliac artery occlusion [19,20], a randomized controlled trial from 2015 did not indicate other benefits of this method [21]. Such procedures performed in hybrid theatre may prevent unnecessary transport of the patient between the multidisciplinary team of involved clinicians.
Finally, it should be remembered that the key to successful treatment of placenta accreta spectrum is a proper multidisciplinary team of clinicians. It is also a prerequisite in planning the procedure [22]. The patient should be managed by clinicians with experience in the treatment of obstetric complications especially obstetric haemorrhage.
High-quality evidence on the optimal management of PAS remains scarce, as most available data are derived from retrospective cohorts, case series, and individual clinical reports. There is a pressing need for well-designed prospective studies and randomized controlled trials to determine which interventions most effectively reduce maternal blood loss and improve outcomes. The small sample sizes of existing studies limit statistical power and generalizability. Given the increasing incidence and severity of PAS, the development of standardized protocols and robust clinical data is essential to guide evidence-based practice.
Placenta accreta represents a significant clinical challenge resulting from the continuously increasing number of cesarean sections worldwide. Therefore, global efforts should be made to reduce the frequency of these procedures and to provide adequate patient education about the potential complications associated with surgical deliveries. For diagnostic purposes, the use of Doppler ultrasonography and magnetic resonance imaging is essential for the timely identification of PAS and for appropriate preoperative planning.
Regarding management, priority should be given to carefully scheduling the cesarean section and possible hysterectomy at an optimal gestational age to minimize the risk of massive hemorrhage and hypovolemic shock. The procedure must be meticulously planned due to its complexity and the need for interdisciplinary collaboration involving obstetricians, anesthesiologists, radiologists, and urologists. Whenever feasible, performing surgery in a hybrid operating suite can reduce the risks associated with intra-hospital patient transfers during emergency situations.
According to international guidelines (FIGO, SMFM, RCOG), in cases of PAS where hysterectomy is contraindicated or not immediately required, alternative management strategies may be considered. These include performing the cesarean section with an incision away from the placental site and avoiding manual removal of the placenta unless preoperatively agreed upon. In situations where the placenta is left in situ, continuous intraoperative and postoperative monitoring of blood loss and vital signs is mandatory. When available and clinically appropriate, bilateral uterine artery embolization may be performed to limit ongoing hemorrhage.
The presented case illustrates the importance of early prenatal suspicion, appropriate imaging, and coordinated multidisciplinary surgical planning in achieving a favorable outcome despite the presence of multiple risk factors. With timely diagnosis and structured interdisciplinary care, both maternal and neonatal lives can be successfully preserved.
This case report was conducted in accordance with institutional ethical standards and the Declaration of Helsinki. Ethical approval was not required for this type of study in accordance with the policies of Department and Clinic of Obstetrics and Perinatology, Medical University of Lublin. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Conceptualization: Milena Krawczyk
Methodology: Milena Krawczyk
Software: Milena Krawczyk, Katarzyna Zych, Dominika Żyła, Piotr Komasara
Check: Milena Krawczyk, Patrycja Bździuch, Dominika Żyła, Julia Nowakowska
Formal analysis: Milena Krawczyk, Katarzyna Cencelewicz, Piotr Komasara
Investigation: Milena Krawczyk, Patrycja Bździuch, Katarzyna Cencelewicz, Dominika Żyła
Resources: Milena Krawczyk, Katarzyna Cencelewicz, Katarzyna Zych
Data curation: Milena Krawczyk, Patrycja Bździuch, Katarzyna Zych, Julia Nowakowska
Writing - rough preparation: Milena Krawczyk, Katarzyna Zych, Dominika Żyła, Piotr Komasara
Writing - review and editing: Milena Krawczyk, Patrycja Bździuch, Katarzyna Cencelewicz, Julia Nowakowska
Visualization: Milena Krawczyk, Piotr Komasara, Julia Nowakowska
Supervision: Milena Krawczyk
Project administration: Milena Krawczyk
All authors have read and agreed with the published version of the manuscript.
Artificial intelligence tools (e.g., ChatGPT, OpenAI) were used to assist with language editing, structural refinement, and the formulation of selected textual segments (e.g., background synthesis, objectives, conclusions). All AI-assisted content was critically reviewed, fact-checked, and finalized by the authors.