- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Aim: To study the influence of macrophages or CD68 positive cells on the processes of proliferation and apoptosis in the respiratory system.
Materials and Methods: Experimental modeling of chronic hypoxic hypoxia in combination with inhalation of natural gas was carried out on 133 outbred male rats. Hypoxia was simulated using special seed chambers and natural gas from the Astrakhanskoye Conventional Gas Field at a concentration of 3 mg/m3. The animals were placed under these conditions four hours a day for five days a week for four months. The animals were removed once a month - after 30, 60, 90 and 120 days. The activity of proliferation and apoptosis processes was studied by immunohistochemical method, followed by analysis of the expression of the proliferation marker Ki67, the apoptosis marker p53. The morphofunctional activity of macrophages was determined by the distribution of CD68 positive cells in structural components of respiratory system and the cytokine content in arterial blood taken from the abdominal aorta, that is, at the exit from lungs.
Results: With the increase of the chronic experiment duration, the formation of two types of multidirectional morphological changes was revealed: thinning and stretching of the interalveolar septa, an increase in the volume of the alveoli in the peripheral parts of the lungs, and thickening of the interalveolar septa due to increased blood supply and edema-swelling in the early stages and proliferation of fibrous connective tissue in later periods; whereas the diameter and volume of the alveoli became smaller. Under chronic hypoxia combined with the action of natural gas, in all studied structures of the respiratory system there was an increase in the activity of CD68 positive cells. This is manifested by an increase in their number and activation of spontaneous and induced production of the pro-inflammatory cytokine TNFα. Besides, in areas of the lungs with changes in the type of atelectasis, an increase in the expression of the proliferation marker Ki67 and the apoptosis marker p53 was revealed. The latter is most likely associated with a deterioration in blood supply and oxygenation of these areas and the migration of leukocyte and fibroblast cells here, followed by their proliferation and formation pulmonary fibrosis. In areas with emphysematous changes, a decrease in the content of Ki67 positive cells was revealed with a simultaneous increase in the number of p53 positive cells.
Conclusion: Thus, it is possible to determine a direct relationship between the increase in the morphofunctional activity of CD68 positive cells and the intensity of proliferation and apoptosis processes in the structural components of the respiratory system under chronic hypoxia combined with natural gas inhalation.
Keywords: respiratory system, emphysema, atelectasis, proliferation, apoptosis, CD68 positive cells, hypoxia.
The research of changes in the structural and functional organization of organs and tissues formed under the influence of both biotic and abiotic environmental factors, including industrial ones, is one of the modern directions of morphological research. The most sensitive to the effects of such factors are the structural components of the respiratory system, since the inhalation route of penetration of toxic substances, antigens and infectious agents is the most common and dangerous [1]. It is not surprising that there is an intensive increase in the incidence of diseases of the respiratory system, especially chronic ones [2]. In addition, it should be taken into account that the course of the co-infection will depend on the initial state of the components of the respiratory system, which has been especially important in the recent years [3-5]. Toxic agents cause damage to any tissue. The epithelium of the bronchi and alveoli of the lungs, however, due to its location, anatomy and physiology, is especially susceptible to the action of toxic substances [6-8]. Regeneration of the damaged bronchial and alveolar epithelial barrier is critical for survival and recovery of both respiratory and metabolic functions of the lung [9-14]. At the same time, cells of the immune system play an important role in the recovery processes [15-17].
In our work, we tried to identify the main aspects of the morphofunctional interactions between the cellular elements of the immune system (CD68-positive cells) and the epithelium of the respiratory part of the respiratory system and airways in normal conditions and in the conditions of an external irritating factor. This model was chosen as an irritating factor in the form of chronic hypoxic hypoxia combined with inhalation of natural gas from Astrakhanskoye Conventional Gas Field (Russia) in a concentration corresponding to the maximum allowable concentration.
The Aim of this research was to study the influence of CD68 positive cells on the processes of proliferation and apoptosis in the respiratory system.
Experimental research was conducted on 133 outbred male rats kept in a vivarium in accordance with the rules and regulations for handling laboratory animals. All manipulations during the experimental study were performed in accordance with the existing standards, as evidenced by the conclusion of the local ethical committee No 3 dated 12/27/2021. The experiment was reproduced using special seed chambers (manufactured by Moscow FF Erisman Research Institute of Occupational Diseases and Occupational Health). The seed chamber had a volume of 200 liters, a standard composition of the air-gas mixture with the addition of natural gas (Astrakhanskoye Conventional Gas Field) at a concentration of 3 mg / m³ through an additional ventilation technical channel. The experiment lasted four months, the breeding of animals was carried out once a month - after 30, 60, 90 and 120 days. Besides, a control group of animals (n=25) was assigned. Individuals of the control group were placed in the chamber in a similar time regime, but with the usual composition of air without gas supply.
For immunohistochemical studies, Menzel-Glaser glasses with Thermo Scientific poly-L-lysine coating were used, which reliably ensured the fixation of sections even after their long stay in a humid chamber (3 days). One part of the preparations was made manually, the other part of the preparations was automated. To perform an immunohistochemical study, paraffin histological sections were made on a LEICA RM 2255 microtome (Germany) 4 µm thick and stained automatically using a Leica Microsystems Bond™ immunohistotainer (Germany). The following panel of monoclonal antibodies was used as primary: Ki-67 (Ready-to-Use, clone Mib 1, Daco, Denmark), CD68 (Ready-to-Use, clone 514H12, Leica Biosystems Bond™, Germany), P53 (Ready-to-Use, clone 7JUL, Leica Biosystems Bond™, Germany. Indirect streptavidin-biotin detection system Leica BOND (Novocastra™, Germany) was used for staining. Evaluation of reaction specificity was performed by staining sections without primary antibodies. Analysis and visualization of the obtained glass preparations was carried out using a Zeiss Axio Scope A1 light microscope (Germany) and a Leica AperioCS2 digital slide scanner with specialized software that allows to control the settings and image capture. Positively stained cells were counted to evaluate the results of the immunohistochemical reaction (CD68 and P53 positive, Ki-67 positive nuclei) in 10 random fields of view that do not intersect with each other, not less than ten layers of a part of the organ for each period of the experiment with a magnification of x400, followed by the calculation of the arithmetic mean. Cytokine tumor necrosis factor alpha was determined using enzyme immunoassay in blood serum and isolated stimulated mononuclear cells from whole blood using rat monoclonal antibodies from BIOSUORCE, Belgium to TNF-α. Statistical processing of the obtained results was carried out by the variational-statistical method using the licensed program "Microsoft Excel" from the MS Office 2016 package in the Windows 10 environment. The obtained data were checked for the normality of the distribution of the studied features by determining the parameters "SKOS" and "EXCESS" in the section "Arguments Functions" of the program "Microsoft Excel". Quantitative data with a normal distribution are presented as M ± σ, where M is the mean value, σ is the standard deviation. To determine the significance of the difference between the mean values, one-way analysis of variance was used. Differences were considered statistically significant at p<0.001.
The full functioning of epithelial tissues is possible only in the condition of their regeneration. The morphological picture of the state of the structures of the respiratory system depending on the duration of natural gas inhalation was assessed, and a comparative assessment of the processes of proliferation and apoptosis was carried out in the corresponding periods of the experiment. It was found that no pronounced morphological changes occur in the first thirty days, which is associated with the activation of adaptive reactions. By the sixtieth day of the experiment, two types of multidirectional changes begin to form in the respiratory section of the lungs. In the first case, the morphological picture is characterized by changes in the type of emphysema - thinning, overstretching of the interalveolar septa with signs of rupture, an increase in the diameter of the alveoli and general airiness of the lungs (Figure 1a).
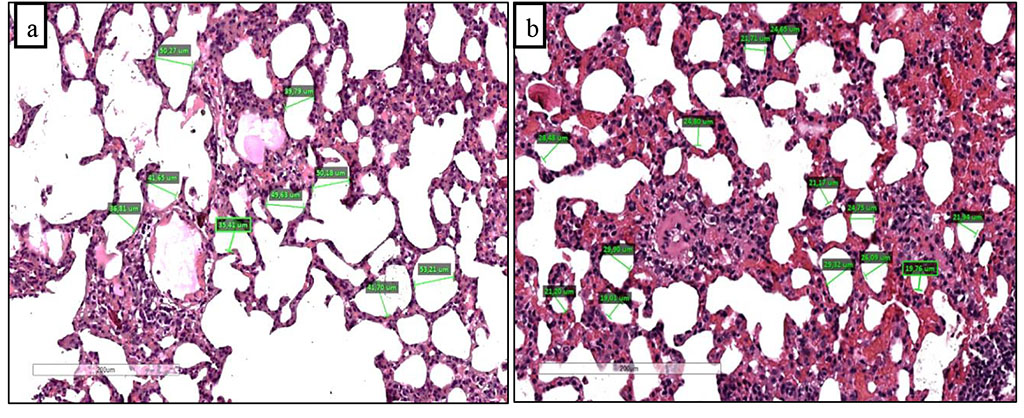
Figure 1. Overstretched and partially damaged alveoli around vessels with edema and perivascular infiltration (a) and thickened interalveolar septa with perivascular edema and infiltration (b) after 60 days of chronic hypoxia with inhalation of natural gas. Staining with hematoxylin and eosin. Zoom. x200.
In the second case, the changes were progressing according to the type of atelectasis - thickening of the interalveolar septa, a decrease in the diameter of the alveoli and the general airiness of the lungs (Figure 1b). The emerging changes gradually increased in accordance with the duration of the experiment. When analyzing changes in the airways, the most pronounced changes were detected on days 90 and 120 in the form of peribronchial infiltrates with changes in the bronchial wall - thickening, deformation. And by 120 days, a significant part of the bronchi was deformed.
Assessing the processes of proliferation and apoptosis in the control group we found a weak immunopositive reaction to Ki-67 (Figure 2a), mainly in the alveolar epithelium. Practically no positive staining for the apoptosis marker p53 was detected. Since the beginning of the experiment, both markers have shown a positive trend.
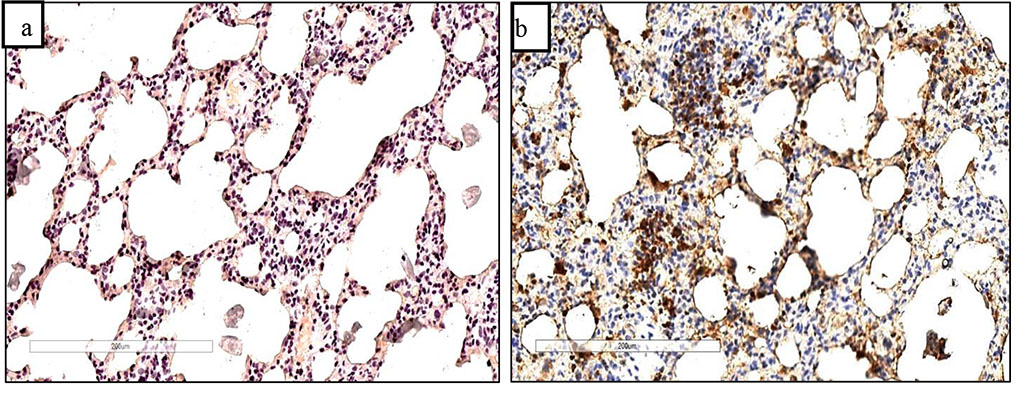
Figure 2. Faint Ki67 staining in the control group of animals (a) and immunopositive staining of Ki67 positive cells in thickened interalveolar septa after 60 days of chronic hypoxia with natural gas inhalation (b). Staining with antibodies to the Ki67 marker. Zoom. ×240.
The maximum increase in the proliferation marker Ki67 was detected on the 60th day of the experiment (Figure 2b), after which its expression in the alveolar structures began to decrease. It indicates a decrease in the regenerative activity of epithelial cells in this area. On the contrary, in the altered areas of the lung tissue surrounding the vessels and bronchi an increase in Ki67 expression was noted, especially in cell infiltrates, which can be associated with the proliferation of cells of leukocyte and fibroblast origin.
The processes of regeneration and recovery directly depend on the additional antigenic and toxic load that macrophages must cope with in the respiratory system. We have evaluated the distribution of CD68 positive cells in the structures of the respiratory system. In the control group of animals, the predominant localization of these cells is the respiratory section of the respiratory system. We believe that alveolar macrophages manifested themselves in this way. Under the action of natural gas, an increase in CD68-positive cells was noted both in the structures of the terminal compartment and in the structures of the airways (Fig. 3a and 3b).
Given that the CD68+ marker is both intracellular, being present on the endosome membrane, and extracellular, participating in cell-cell or cell-pathogen interactions, its organization and location can suggest the degree of activity of a CD68 positive cell. The intake of toxic substances from the outside, the effect of these substances on the structural components of the respiratory system and activated apoptosis lead together to a sharp increase in the activity of macrophages [18], which not only increase their presence in all parts of the respiratory system, but also show increased functional activity [19-21]. This is manifested by increased synthetic activity, expression of biologically active molecules, and production of cytokines [22, 23], including tumor necrosis factor alpha (TNF-α).
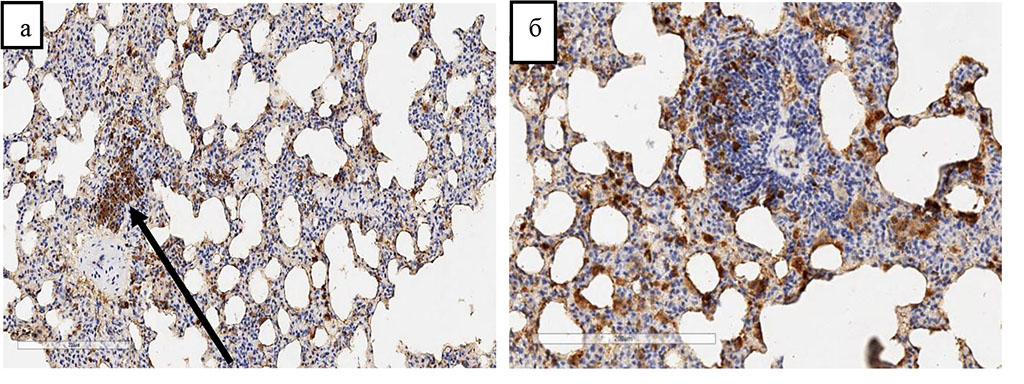
Figure 3. Release of CD68 positive cells from the vascular bed into the perivascular space (indicated by an arrow) after 60 days and an increase in the number of CD68 positive cells in the perivascular space (a) and interalveolar septa after 120 days (b) of chronic hypoxia with inhalation of natural gas. Immunohistochemical staining with antibodies to the CD68 marker. Indirect streptavidin-biotin detection system. Zoom. ×280.
Analyzing biochemical parameters for spontaneous and induced production of TNF-α we revealed changes in the number and distribution of CD68 positive cells. Thus, an increase in the number of CD68 positive cells coincides with an increase in induced production, which shows the reserve capacity of producer cells. However, the decreasing production of TNF-α on days 90 and 120 may indicate a decrease in adaptive and compensatory capabilities, which is consistent with the data of recent morphological studies. Spontaneous production of TNFα increases with the duration of the experiment, which may indicate constant stimulation by antigens, toxic products, and cell decay products. This, in turn, suppresses the regenerative potential of cells and activates proapoptotic mechanisms.
Chronic hypoxic hypoxia in combination with natural gas inhalation causes an increase in the presence and functional activities of macrophage cells. This is expressed by an increase in the expression of the CD68 marker and a corresponding change in the spontaneous and induced production of the pro-inflammatory cytokine TNFγ. It is also possible to determine a direct relationship between the increase in the morphofunctional activity of CD68 positive cells and the intensity of proliferation and apoptosis processes in the structural components of the respiratory system under chronic hypoxia combined with natural gas inhalation.