- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
The described clinical example illustrates the rare association of psoriasis with basal cell and squamous cell carcinoma. This clinical case may be of interest to dermatologists and oncologists. It illustrates the neglect of the process in view of the late treatment of the patient.
The rising incidence rates of skin cancer are caused by exposure to UVB procedures and increasing with age, which emphasizes the importance of thorough dermatological screening among patients with psoriasis and histological examination of old psoriatic plaques. Alertness for the early detection of skin tumors is relevant not only among medical workers, but also among the population.
Keyword: psoriasis, basal cell carcinoma, squamous cell carcinoma, multiple foci.
Psoriasis is a disease affecting from 3 to 4% of the population, making it a serious global problem. According to various authors, the disease occupies 3rd place in the skin pathology [1].
Psoriasis is a chronic, recurrent, genetically determined and multifactorial disease with acute skin symptoms, based on inherited disorders of epidermal keratinization caused by hyperproliferation and impaired keratinocyte differentiation that occurs under the influence of endogenous and exogenous factors [1, 2].
The coexistence of several diseases (comorbidity) in the combination with the underlying disease is observed [3]. Compared with the general population, patients with psoriasis are at an increased risk of concomitant diseases such as arthritis, coronary heart disease, diabetes, hypertension and oncological diseases [4, 5]. The risk to develop concomitant diseases in psoriasis patients increases with age. Almost half of psoriasis patients aged 65 or more have at least three concomitant diseases, and 2/3 of these patients have 2 or more concomitant diseases [1].
Patient S., 82 years old, went to the dermatologist with complaints of skin rashes on the upper body and limbs. Some rashes were painful.
Anamnesis of the disease: The patient has suffered from psoriasis for 30 years. He underwent light therapy sessions and was regularly treated on an outpatient basis with various drugs, mainly for the external use. The patient refused inpatient treatment. He had experienced the last disease exacerbation during several months and applied topical corticosteroids without seeking medical help for the last seven years.
Anamnesis of the life: The patient had viral hepatitis. There is no previous history of syphilis, operations and injuries. The history of allergic reactions is unremarkable. Heredity for skin and oncological diseases is not burdened. He previously lived in Kazakhstan and was repeatedly exposed to solar insolation, including sunburns. He had no occupational hazards and was not exposed to ionizing radiation. At present, the patient is examined with the following diagnoses: hypertension of the second degree, arterial hypertension of the second degree, chronic heart failure (IIA), multifocal atherosclerosis, femoral artery stenosis (40% on the left femoral artery and 45% on the right femoral artery), stenosis of coronary arteries (40% on the right coronary artery and 55% on the left coronary artery), anterior tibial artery occlusion, post-thrombotic syndrome of the right lower limb, chronic venous insufficiency of the second degree, obliterating arteriosclerosis of lower limb arteries, сhronic arterial insufficiency (I), mixed nephropathy, dyscirculatory encephalopathy (I), subcompensated type I diabetes, hypertensive retinopathy, presbyopia, chronic cholecystopancreatitis, remission, obesity (I). The patient received medical treatment for the concomitant diseases.
The pathological skin process is common, appeared on the skin of the upper body, upper and lower limbs. There are scattered lenticular, nummular papules, pink-red plaques (up to 10 cm in diameter) with gray and yellow patches. Some plaques have bleeding nodes (from 2 to 6 cm in diameter), covered with crusts, horny masses and warty growths (See Figures 1, 2, 3, 4). Peripheral lymph nodes are enlarged in the area of armpits and groin (up to 0,5 cm); they are soft and painless. In addition, there are multiple hyperpigmented lesions (0,3-2 cm in diameter), rounded and brown (from light to dark brown) with scattered dark red spots (0,3-0,5 cm in diameter) and lenticular brown flat papules.

Figure 1. Spots, plaques, nodes on the skin of the upper limbs, chest, abdomen

Figure 2. Spots, plaques, nodes on the skin of the right shoulder and chest

Figure 3. Spots, plaques, nodes on the skin of the back

Figure 4. Spots, plaques, nodes on the skin of the lumbar
The diagnostic dermoscopy corresponds to basal-cell carcinoma (multiple atypical blood vessels are visible) and squamous cell carcinoma (hairpin and linearblood vessels, whitish ring-shaped areas are visible) (Figure 5).
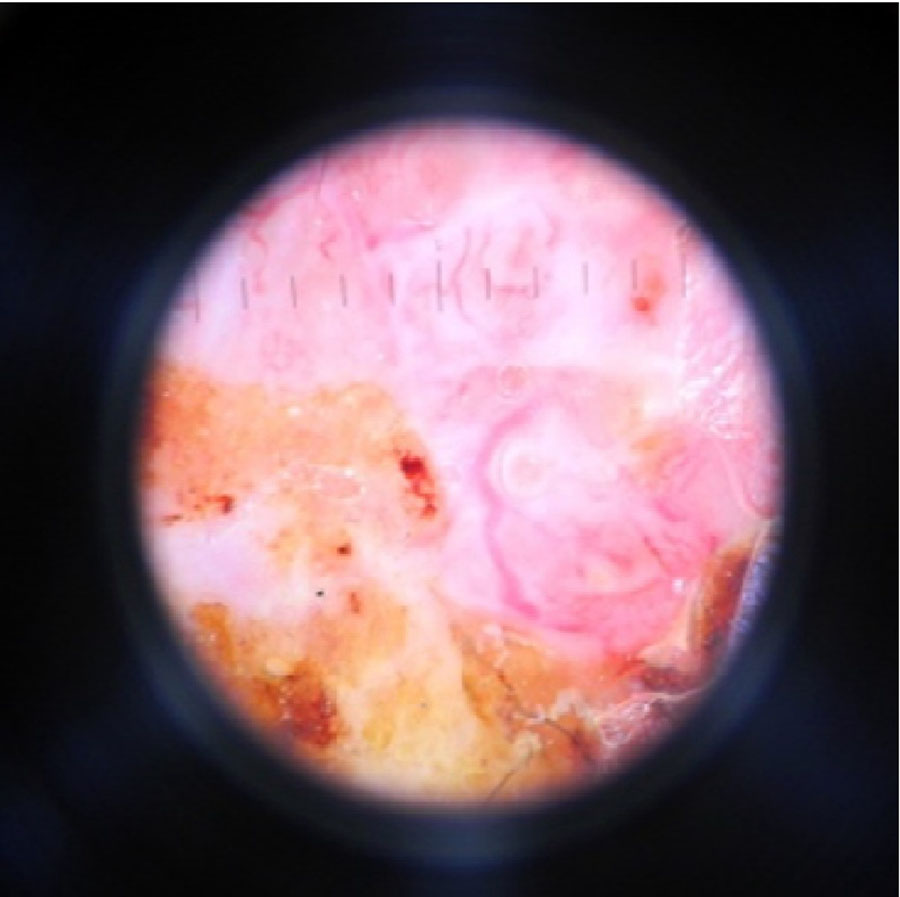
Figure 5. Dermatoscopic picture of basal cell skin cancer in patient C. (Heine Delta 20, eyepiece-10, immersion, non-polarized mode)
General test. Blood analysis: leukocytes 9,45*109 /L, red blood cells 4,95*1012 /L, platelets 254*109 /L, hemoglobin 136 g/L, erythrocyte sedimentation rate 50 mm/h, band neutrophils 6%, segmented neutrophils 84%, eosinophils 0%, monocytes 2%, lymphocytes 8%.
Biochemical blood analysis is without marked changes.
Chest Х-ray is without “fresh" focal-infiltrative changes.
The histological skin examination of the right breast, the left chest and the left shoulder defines lobulation with mild diskeratosis, keratinization of individual cells and acantolysis of lobules. There are alveolar and glandular structures with single or stratified epithelium. The gaps are filled with desquamated acantholytic cells, partially or fully keratinized. Cellular atypia is with distinguished squamous differentiation, enlarged hyperchromatic nuclei. Tissue atypia is with the stratified squamous epithelium, loss of intercellular bridges. The histological skin examination corresponds to squamous cell carcinoma.
The results of the histological skin examination of the left thigh and lumbar: the presence of epithelial cells with dark nuclei, the absence of intercellular bridges, tissue stroma with bundles; retention gaps visualized between the parenchyma and stroma. The histological skin examination corresponds to basal cell carcinoma.
In order to determine treatment, the patient was referred to an oncologist. Surgical tumor treatment was performed on the chest, the left shoulder, the left thigh, and the lumbar.
It has not been possible to find the association of psoriasis with the risk of developing cancer yet [1, 4]. Some similarities were found between the pathogenesis of psoriasis and cancer: changes in cell membranes, abnormalities in the cyclic adenosine monophosphate (adenylate cyclase), and the influence of retroviruses [1].
Factors increasing the risk of cancer in psoriasis have been identified: some similar pathogenetic mechanisms of these diseases, the use of various external agents in the treatment of psoriasis, some of which are potential carcinogens, immunosuppressive therapy, photochemotherapy (European patients who received more than 250 sessions of PUVA therapy have a 14 times higher risk of squamous cell carcinoma [5, 6, 7].
Numerous studies have revealed a link between psoriasis and certain types of cancer, including lymphoma, visceral cancer and skin cancers [5]. The increased risk of malignant tumors associated with psoriasis may be due to the immunosuppressive therapy. The risk of developing lymphomas and non-melanoma skin cancer is possible with psoriasis as well [1, 2, 7, 8, 9, 10]. The risk of developing melanoma skin cancer does not exceed that in the population [9]. Also, some researchers do not exclude a possible link between the psoriasis severity and cancer risk [10].
Several possible catalysts for carcinogenesis can be identified in our patient: living in the climatic zone with active insolation and multiple phototherapy procedures.
The poor prognosis is due to the late diagnosis of the pathological process. The described clinical example illustrates the rare association of psoriasis with multiple localizations of squamous and basal cell skin cancers.
This clinical case may be of interest to dermatologists and oncologists. It illustrates the neglect of the process in view of the late treatment of the patient.
The rising incidence rates of skin cancer are caused by exposure to UVB procedures and increasing with age, which emphasizes the importance of thorough dermatological screening among patients with psoriasis and histological examination of old psoriatic plaques. Alertness for the early detection of skin tumors is relevant not only among medical workers, but also among the population.
The authors confirm that they have received all relevant forms of patient consent to publication his images and other clinical information. Patients understand that their names and initials will not be published, and appropriate efforts will be made to hide their identity, but anonymity cannot be guaranteed.