- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Insufficient blood flow to the proximal femur causes osteonecrosis of the femoral head, which is known as femoral head avascular necrosis (AVN). The underlying pathogenesis is unclear, risk factors are likely to influence microcirculation somewhat, but this has not been confirmed by research. In more than 75% of cases, avascular necrosis affects the femoral head.
Methods: From August 2019 to March 2022, 4 patients with FBAN were analyzed retrospectively. The findings seen in the hip MRI radiographs of the patients were reported radiologically as FBAN. It was staged with the Ficat and Arlet classifications. Visual analog scale (VAS) was used in the current clinics of the patients.
Results: Patients with severe back, hip, and leg pain whose clinic and radiology do not match with lumbar pathology should plan a hip MRI. Because of this, it may be misleading for people with severe radiculopathy, and this radiculopathy may not even be real. The pain is really coming from the hip, but it is often felt in the lumbosacral region and the buttocks. This makes it easy to make the wrong diagnosis.
Keywords: Avascular necrosis, Low Back Pain, MRI, femur
Osteonecrosis of the femoral head resulting from insufficient blood flow to the proximal femur is known as avascular necrosis of the femoral head (AVN). The underlying pathogenesis is unclear, risk factors likely to influence microcirculation somewhat, but this has not been confirmed by research (5). The femoral head is affected by avascular necrosis in over 75% of cases (9).
The purpose of this paper is to provide clinicians with clinical and radiological clues that may facilitate the identification of femoral head avascular necrosis.
From August 2019 to March 2022, patients with radiculopathy who came to the neurosurgery clinic were examined. The patients applied with the complaint of radiculopathy.
Hip problems were considered because of clinical and radiological incompatibility. An investigation has been made for this.
After our investigations, they were diagnosed with Femoral head avascular necrosis (AVN). This study is observational all patient examined for clinical, radiological and prognostic factors of the patients were examined.
Each patient filled out a baseline questionnaire with a visual analog scale (VAS) (10). The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were followed when writing this paper (12).
The typical VAS is 100 mm in length. When measured with a 1 mm precision, this produces a 101-point scale that looks like this: 0, 1,..., 100. In this article, VAS was measured in millimeters and ranged from 0 to 100. On a line running from left to right (left: no pain, right: severe pain), the patients were prompted to identify their level of discomfort.
All four patients were male, and the mean age was 54.5 years. None of the patients had undergone spinal surgery. One patient had hip surgery. The other patient was offered hip surgery, but the patient refused. Four male patients were smokers. Two patients also had hypertension. One patient also had ankylosing spondylitis. One patient was an alcoholic. The mean follow-up period of the patients was 1.75 years. VAS scores were measured at the patient's admission to the clinic, at 6 months, and at 1 year.
We present four individuals who had femoral head osteonecrosis and complained of leg discomfort and low back pain. All four patients were male.
The first patient was a 53-year-old man. It was found that he had hip and leg pain for one week, which did not go away despite the drugs he was using, and was now unable to move. He had undergone cervical disc surgery before, and his VAS score was 90 mm. Lumbar MR images showed protrusion. Due to severe foot pain, a hip MRI was requested as a further examination. In his history, it was determined that he had walked 20 kilometers without stopping during a trip abroad one day before the onset of pain, and he started the next day with this pain. In his neurological examination, he had no motor deficit and could not stand on his left foot due to pain. There was no lumbar or hip tenderness. Since the patient's lumbar MRI images are not compatible with the patient's clinical condition; the patient was re-examined with an MRI of the hip as an additional examination. The MRI of the hips revealed that the right hip had stage 2 avascular necrosis and the left hip had stage 3 avascular necrosis. (Figure 1).
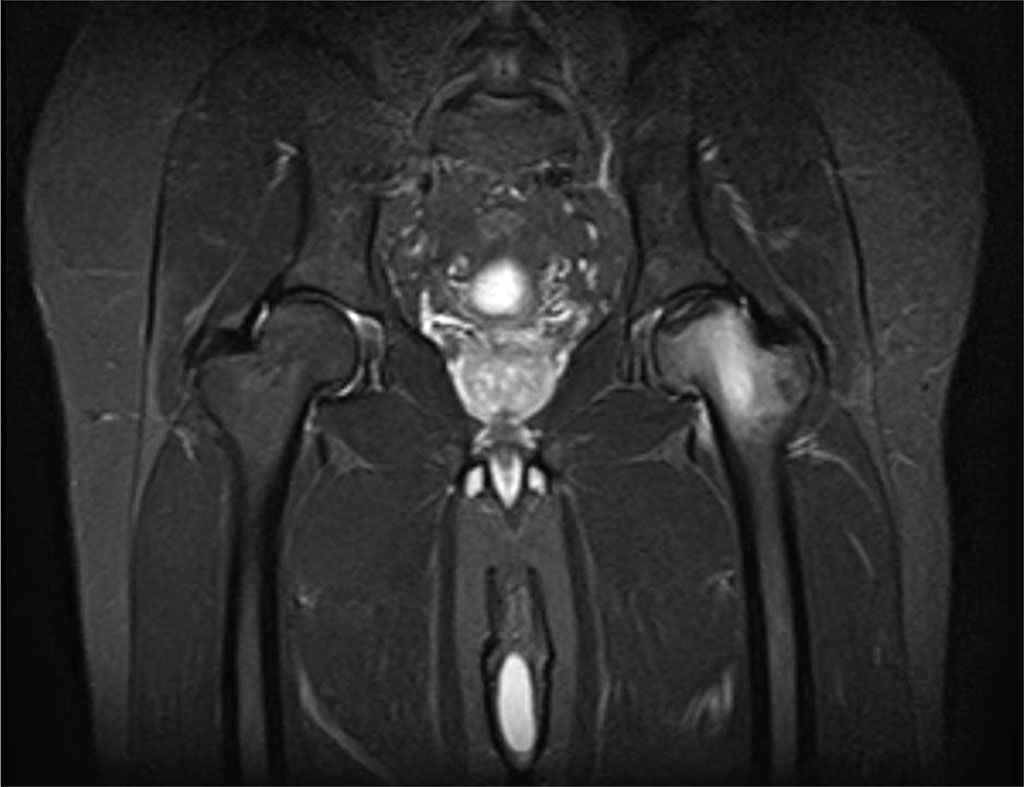
Figure 1. Findings in a 53-year-old man with stage 3 avascular necrosis of the left hip.
The patient was evaluated at the Orthopedics and Traumatology Department, and left hip arthroplasty was performed. The patient's complaints disappeared immediately after surgery and he had no problems in his follow-up. The patient has a 3-year follow-up
The second patient, a 49 year old male patient, has intermittent low back pain for 15 years. The patient has had chronic alcohol use for a long time. He has a history of hypertension and diabetes. The patient endured pain in his left hip for the past four years. Lumbar disc surgery was recommended to this patient because he had discopathy in the lumbar MRI findings in another center, but the patient did not accept it. Lumbar MRI report: L3-4 annulus bulging. L4-5 left medio-lateral subligamentous HNP. Retrolisthesis at L5-S1 level and associated pseudo-hernia appearance and right medio-lateral protrusion (Figure 2).
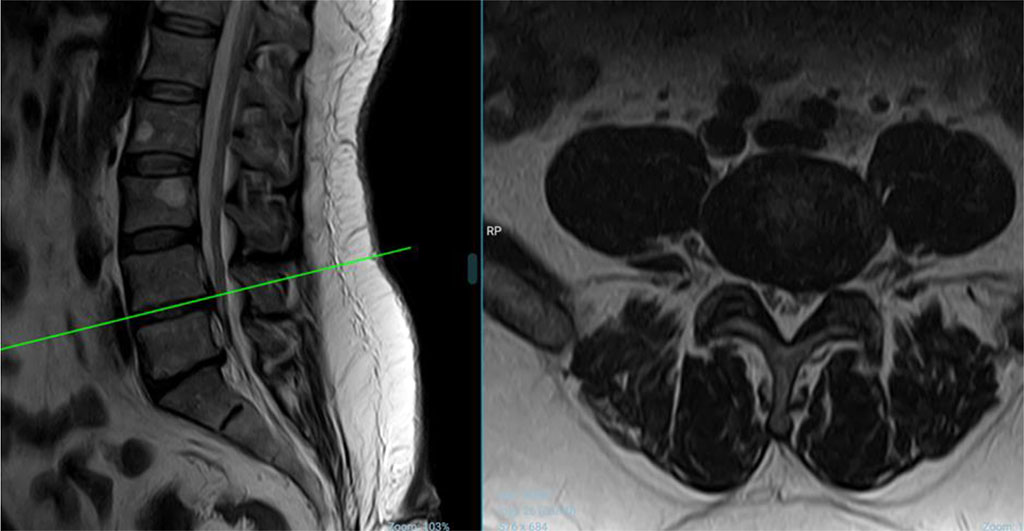
Figure 2. The second patient's lumbar MRI (Sagittal and Axial) picture
Hip MRI was performed and the problem was detected. The pain intensified after standing up for the last 1 month and hip MRI revealed findings related to stage 2 avascular necrosis in the right hip and stage 3 avascular necrosis in the left hip (Figure 3).
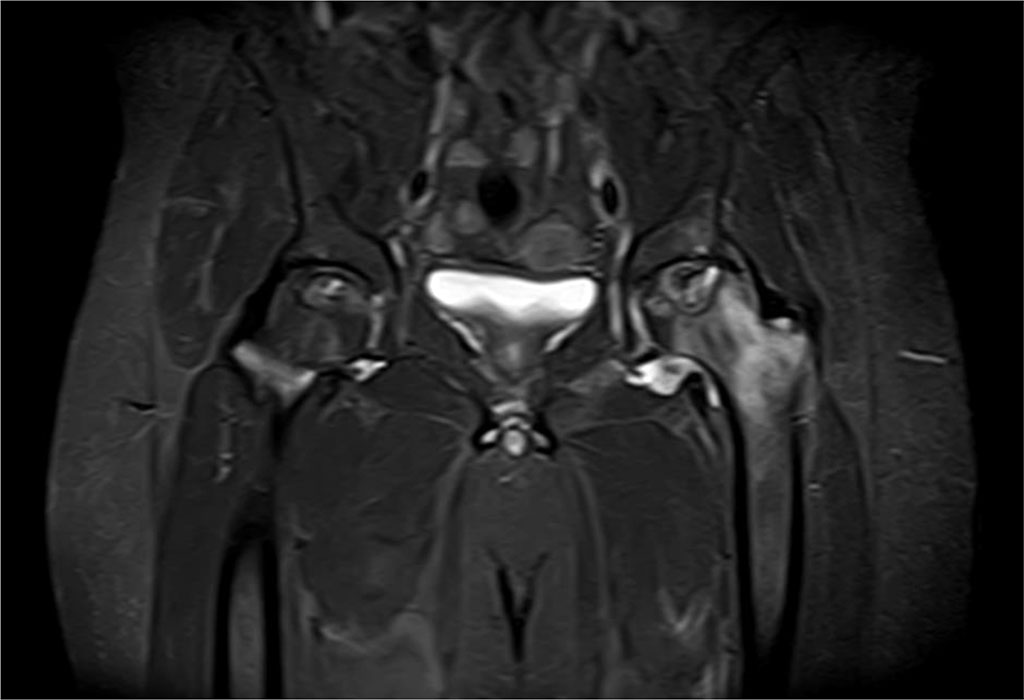
Figure 3. Findings in a 50-year-old male patient with stage 3 avascular necrosis of the left
Surgery was recommended to the patient, but the patient refused. This patient has a 1-year follow-up.
The third patient is a 51 year old male patient. The patient, who was diagnosed with ankylosing spondylitis for more than 20 years ago and used salazopyrin, indomethacin, and glucocorticoids. He stopped treatment 1-2 years ago and had irregular drug use. He had right hip pain 1 month ago and right hip direct X-ray, lumbar MRI, knee MRI were taken for this pain. When the patient stands up, there is severe hip pain and this pain goes up to the knee. There is no conflict. He has trouble standing on his feet from the pain. In the hip MRI, findings related to stage 3 avascular necrosis in the right hip and stage 2 avascular necrosis in the left hip were detected. The patient was offered surgery, but he refused. This patient has a 2-year follow-up.
The fourth patient, a 65-year-old man with significant left leg pain, had protrusion discovered in his lumbar MRI, and upon reevaluation, a hip MRI was ordered due to the patient's worsening inguinal discomfort. Findings related to stage 1 avascular necrosis in the right hip and stage 3 avascular necrosis were detected in the left hip. The patient will be followed up with in a year.
Surgery was recommended for four patients as a result of orthopedic consultation. However, except for the first patient, the others did not accept the operation. The first patient underwent hip surgery and reported less pain (VAS: 0 mm) afterward, and two months later, he was able to resume his normal activities. Since the other three patients have not had hip surgery yet, their pain continues and their participation in active life has decreased.
Femoral head avascular necrosis (AVN) is osteonecrosis of the femoral head due to insufficient blood supply of the proximal femur. Many factors are responsible for the etiology. Impaired subchondral microcirculation is likely a common pathway in pathophysiology (6, 11). Microcirculation is likely to be affected in some way by risk factors, but this has not been fully proven by research (5). Fractures, dislocations, chronic steroid use, chronic alcohol use, coagulation disorders, and congenital causes can induce necrosis. Our patients also had these risk factors.These risk factors are compatible with the literature.
While more than 80% of atraumatic cases are associated with the use of glucocorticoids and excessive alcohol intake, the most common cause is a femoral neck fracture or dislocation of the femoral head from the acetabulum. There was no femoral neck fracture or dislocation of the femoral head from the acetabulum in our patients.
These injuries may restrict blood flow to the femoral head, causing avascular necrosis. 10% to 25% of hip dislocations and 15% to 50% of femoral neck fractures result in osteonecrosis. (1).
Avascular necrosis affects the femoral head in over 75% of instances (9). Femoral head osteonecrosis is commonly misdiagnosed as lumbar disc herniation, hip synovitis, hip osteoarthritis, and rheumatoid arthritis. The patient's history of corticosteroid use or alcohol misuse, as well as magnetic resonance imaging (MRI) examination at the time of the initial diagnosis, may protect against misdiagnosis (6). MRI has revolutionized the diagnosis and evaluation of early cases and is the gold standard. MRI remains the gold standard for detecting pre-collapse lesions and permits differentiation from conditions such as AVN, transitional osteopenia of the femoral head, and bone contusions. MRI has a sensitivity and specificity of approximately 99 percent (8). Computed tomography is not routinely recommended. Bone scintigraphy has low sensitivity and is recommended when MRI is contraindicated.
Ficat and Arlet discovered avascular necrosis of the femoral head (AVN) in 1964, before MRI was invented. In 1985, it was changed and published to include pre-radiographic stages that needed invasive testing. Subsequently, the classification system was modified to include MRI findings, patient symptoms, a revised description of radiographic findings, and the exclusion of the invasive diagnostic procedures originally described (Table 1, Table 2) (3, 4).
Table 1. Ficat-Arlet Staging for AVN hip
| Stage 0 | Silent hip (Pre-clinical and Pre-radiographic) |
| Stage I | Suggestive clinically (Pre-radiographic) |
| Stage IIA | Sclerosis or Subchondral cysts (Pre-collapse) |
| Stage IIB | Subchondral fracture/crescent sign (Transition) |
| Stage III | Segmental flattening and Sphericity loss/out of round appearance (Collapse) |
| Stage IV | Space loss, Secondary osteoarthritis – may involve acetabulum (Advanced arthritis) |
Table 2. Age, Sex, VAS score, Ficat - Arlet Classification and Follow-up time
| Admission | 6. month | 1. year | Ficat and Arlet Classifications | Follow-up Time | ||||
| No | Age | Sex | VAS | VAS | VAS | Right Hip | Left Hip | (year) |
| 1 | 53 | Male | 90 | 10 | 0 | 2 | 3 | 3 |
| 2 | 49 | Male | 85 | 80 | 80 | 2 | 3 | 1 |
| 3 | 51 | Male | 90 | 85 | 75 | 3 | 2 | 2 |
| 4 | 65 | Male | 90 | 85 | 90 | 1 | 3 | 1 |
AVN may be asymptomatic in the early stages. Clinically, the most common symptom is deep pain in the groin, and range of motion becomes limited. Weight gain makes symptoms worse, and rest makes them better. Hip MRI examination was not routinely planned for any of the patients. Our patients first applied to our clinic for lumbar pathology. Although each of the patients had lumbar pathology, these radiological findings were not compatible with the patient's clinic. For these reasons, hip MRI examination was planned for each of the patients.
Deceptive low back and hip pain, especially at night, is often the main subjective symptom of femoral head necrosis (7). Depending on the stage and progression of the disease, avascular osteonecrosis (AVN) may be treated with both conservative and surgical procedures (2). In this period, especially, the limitation of internal rotation and abduction creates an objective symptom. Co-locations of pain only in the lumbosacral region and hip often lead to misdiagnosis.
Patients with severe back-hip-leg pain whose clinical and radiographic findings are inconsistent with lumbar pathology should be scheduled for a hip MRI.
Thanks to Dr. Birol Özkal, Associate Professor of the Department of Neurosurgery at Alanya Education and Research Hospital, Alanya Alaaddin Keykubat University, who generously offered his assistance in producing the clinical data for the paper.