- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
We carried out a single-center study of the effectiveness of polyvalent bacteriophages and oxygenated water for the prevention of SSI. The object was 88 patients who had undergone abdominal surgery for emergency abdominal pathology with a high risk of SSI >30±3% (ACS NSQIP). Phages were administered topically and enterally, while OW only enterally. As a result of the study, it turned out that the combined use of PVBP and OW allows to normalize the induced enteral pathobiome, to reduce pathogen contamination, to enhance the protective capabilities of enterocytes, to stop intestinal failure in the early stages and to reduce the risk of SSI by more than 2 times.
Keywords: bacteriophages, oxygenated water, intestinal decontamination, prevention, surgical infections, surgical site infections
Surgical antibiotic prophylaxis remains the basis of prevention and is one of the most profound, widely used and cost-effective measures to prevent both exogenous and endogenous wound infection. When routine antibiotic prophylaxis was initially introduced in the 1960s - 1980s, infection rates dropped by about 50% to 60% across a wide range of surgical groups. The general assumption that all surgical site infections (SSIs) must necessarily be due to intraoperative contamination led to an expansive use of antibiotics with the idea "the more, the better". Since then, however, the global burden of antimicrobial resistance has increased significantly and is now the leading cause of death worldwide [1].
According to some authors, the endogenous source of infection and the cause of SSI is the intestine, especially in abdominal surgery. Some scientists believe that short-term local or generalized intestinal obstruction occurs during any operations on the abdominal organs. Indeed, the intestinal barrier comprising the luminal microbiota, the mucosal layer, and the physical barrier composed of epithelial and immune cells, plays a special role in health and disease [2-4].
Growth of bacterial multiresistance and the shortage of new antibiotics on the market are becoming a serious public health problem. In this regard, the prophylactic use of phages may be a promising alternative, this is why research in this direction has resumed in many countries. Indeed, phages have several important advantages that contribute to their therapeutic and prophylactic potential: high specificity, rapid inactivation after eradication of the pathogen, the ability to replicate, immune stimulation, the ability to penetrate through the matrix of biofilm infections, inactivity towards human tissues, the possibility of local and oral applications, etc. Recently, intensively developing phage therapy has brought about life-saving therapeutic cases and numerous clinical trials [5–9].
Recent clinical reports have described the therapeutic effects of oxygenated water in a variety of conditions such as obesity, diabetes, liver disease, cancer, and surgical infection. There are previously published scientific papers on the effectiveness of oxygenated water (OW) in anaerobic infection. Probably, one of the effects is the creation of unfavorable conditions for the growth and reproduction of pathogens. The obtained data require further study [10-12].
The purpose of the work was to study the results of the use of polyvalent bacteriophages (PVBP) and OW for the prevention of SSI in abdominal surgery.
The object of the study were patients after emergency open intra-abdominal surgeries performed during the study period in 2019-2022. A total of 88 patients were treated, being divided into two equal comparable groups - the main and comparison groups. The mean age of the patients in the groups ranged from 19 to 82 years. There were 53 men and 35 women.
In the main group, the treatment was supplemented with the use of PVBP and OW. The filtrate of phagolysates of bacteria Staphylococcus, Streptococcus, Proteus (P. vulgaris, P. mirabilis), Pseudomonas aeruginosa, enteropathogenic Escherichia coli, Klebsiella pneumoniae (LS-001049; NPO MICROGEN, Russia) was used as PVBP. All patients of the main group received PVBP orally or through an intestinal tube at a dose of 20 ml 3 times a day. Additionally, after Class III and Class IV operations (according to Altemeir's classification), before suturing the laparotomy wound, it was irrigated with PVBP solution. OW was a specially prepared, purified, natural, abacterial water enriched with oxygen in the amount of 25–30 mg/dm3 (250,000 ppm) with a mineralization of 400–500 mg/dm3. OW was administered orally or through a tube 3 times a day, 200 ml each dose, followed by tube clamping for 60 minutes. PVBP and OW were administered during 5-7 days. Dose-dependent efficacy was not studied in this work. In the comparison group, treatment was carried out in traditional way, without immunization methods. Antibiotic prophylaxis and antibiotic therapy in both groups were carried out in accordance with the current and approved Clinical Guidelines.
For a stratification criterion for inclusion in the study groups, we used the surgical risk calculator ACS NSQIP (2007-2022, American College of Surgeons National Surgical Quality Improvement Program®). We accepted the risk of SSI equal to 30±3% as the inclusion criterion in the study groups. The exclusion criteria were acute disorders of the mesenteric circulation, as well as patients with severe abdominal sepsis and septic shock. Postoperative complications were monitored from days 0 to 30. The severity of the patients' condition was assessed by the Abdominal Cavity Index (ACI according to V.A. Savelyev) and the APACHE II scale. Tab. 1.
Table 1. Stratification of patients by type of nosology and severity of the condition (abs; М±m)
| Nosology/ ACI; APACHE II | Main group (n=44) | Comparison group (n=44) |
| Acute obturation colonic obstruction (tumor) | 12 | 11 |
| Strangulated ventral hernia | 9 | 10 |
| Acute adhesive intestinal obstruction | 10 | 10 |
| Acute appendicitis | 7 | 8 |
| Perforated ulcer of the stomach and duodenum | 6 | 5 |
| ACI | 15,6±1,1 | 15,8±0,9 |
| APACHE II | 14,3±0,8 | 14,7±0,7 |
Isolation and identification of pathogens was carried out using a VITEK 2 Compact 30 4700733 analyzer (France). Colony-forming units (CFU) were determined in 1 ml of small intestine chyme.
To assess the severity of intestinal insufficiency, we dynamically calculated the enteral morphofunctional coefficient (EMFC), which was determined on days 1, 3 and 5 of treatment.
Using the enzyme immunoassay method with the Cobas E411 analyzer (Switzerland), we determined total alkaline phosphatase (U/l), its isoform - intestinal alkaline phosphatase (U/l), as well as their ratio (ALP / IAP, %) in blood serum and intestinal contents. Studies were carried out on days 0-1 and 5.
The Southampton Wound Assessment Scale (SWAS) was used to characterize and stratify the resulting postoperative SSI [14]. According to this scale, all complications are divided into 5 classes (from 0 to V).
Statistical relationships between indicators were assessed using the correlation module "Basic Statistics and Tables STATISTICA 10.0". The method of stratified randomization was used. Student's t test was used to determine the p significance of differences between groups. Differences were considered statistically significant at p≤0.05.
When studying the transluminal enteral pathobiome, it turned out that at the beginning of treatment, the microbial pattern in the main and comparison groups did not differ statistically. The pathobiome was represented by diverse Gram+ and Gram– microflora. A total of 11 major pathogens were identified. We noted threshold exceeding level of contamination due to enteropathogenic strains of Escherichia coli (8.7±0.5×108 CFU per 1 ml), as well as Klebsiella pneumoniae (9.3±0.6×109 CFU per 1 ml). In addition, our attention was drawn to the increased representation of pathogens atypical for the enteric microbiome - Staphylococcus aureus (6.6±0.4×106 CFU per 1 ml) and Staphylococcus saprophyticus (7.4±0.3×107 CFU per 1 ml).
On the day 5 of treatment, the transluminal enteral pathobiome was different in the study groups. There was a tendency towards normalization of the microbial pattern in the main group, which was confirmed by a decrease in the level of contamination by the above pathogens by 1-2 orders of magnitude (p≤0.05). The microbiome was mainly represented by microorganisms typical to the small intestine. We noticed a significant decrease in the representation of pathogens of the Clostridium genus, which in the main group decreased from 8.6±0.4×108 CFU in 1 ml to 4.8×104 CFU in 1 ml (p≤0.05). In the comparison group, on the day 5, the levels of enteral contamination remained high. Fig. 1.
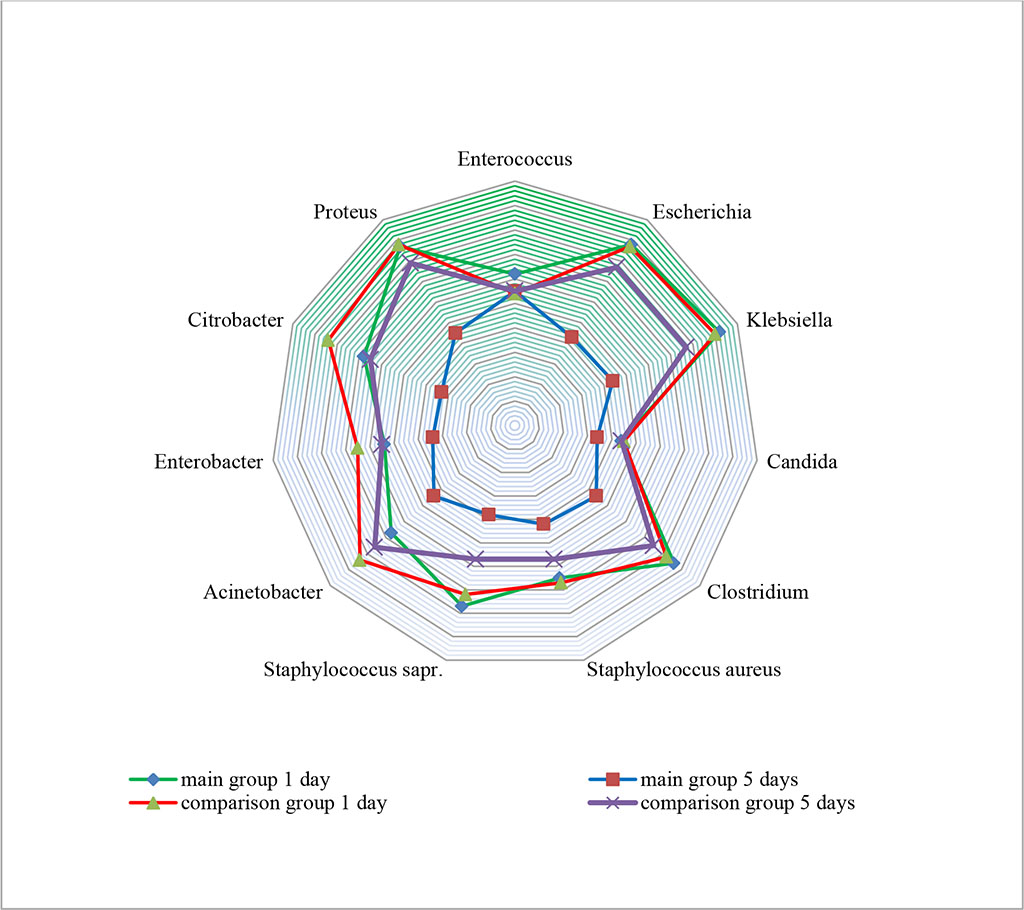
Figure 1. Change in the transluminal enteral pathobiome in study groups (×101-10 CFU in 1 мl)
When studying the markers of enteral insufficiency at the beginning of treatment, it turned out that EMFC values in both groups, on average, corresponded to stage II (subcompensated) intestinal insufficiency and did not differ statistically. In addition, there was a deficiency of the intestinal isoform of alkaline phosphatase, i.e., there was an imbalance in the ALP/IAP ratio with the ALP predominance, which indicated a pronounced inflammation.
On the day 3 of treatment in the main group, the EMFC index obtained as a result of ultrasonographic examination was significantly lower (p≤0.05). In the comparison group, a significant decrease in EMFC was achieved only by the day 5 of treatment. The ALP/IAP ratio reliably returned to normal values by day 5 in the main group (p≤0.05). At the same time, there was no recovery in the IAP level in the comparison group (Tab. 2).
Table 2. Changes in biochemical and instrumental parameters in study groups (M±m; abs.)
| Study groups | Object of study | ALP/IAP (%) | EMFC (points) | |||
| Day 1 | Day 5 | Day 1 | Day 3 | Day 5 | ||
| Main group (n=44) | serum | 0,64±0,28 | 0,41±0,15* | 18,6±0,8 | 6,8±0,4* | 4,6±0,2 |
| chyme | 6,03±0,16 | 3,06±0,11* | ||||
| Comparison group (n=44) | serum | 0,68±0,18 | 0,58±0,14 | 19,1±0,24 | 14,2±0,8 | 8,8±0,7* |
| chyme | 6,11±0,24 | 5,21±0,18 | ||||
* - values at p≤0.05
When analyzing postoperative complications in the form of SSI, it turned out that deep or severe wound infection, accompanied by tissue destruction (class V), was presented in 1 case in the main group: intra-abdominal abscess. At the same time, in the comparison group, this type of complication was noted in 4 cases: 2 - suppuration of the laparotomic wound with complete eventration, 1 - interloop intra-abdominal abscess, and 1 - intestinal anastomosis suture failure. In total, 6 (13.63%) SSIs were noted in the main group, and 14 (31.81%) in the comparison group (Tab. 3).
Table 3. Postoperative complications in study groups (Southampton wound assessment scale) (abs; %)
| Complication class | Subclass | Main group | Comparison group |
I |
IA | - | - |
| IB | - | - | |
| IC | 1 | 1 | |
II |
IIA | - | - |
| IIB | - | - | |
| IIC | 1 | - | |
| IID | - | - | |
III |
IIIA | 1 | - |
| IIIB | - | 1 | |
| IIIC | - | 1 | |
| IIID | - | 2 | |
IV |
IVA | 1 | 2 |
| IVB | 1 | 3 | |
| V | 1 | 4 | |
| Total | 6 (13,63%) | 14 (31,81%) | |
Microbiological examination of pathogens showed that in all cases of SSI class V, a mixed infection was detected. There were 2 cases of microbial associations of Escherichia coli + Acinetobacter, 2 cases of Staphylococcus aureus + Citobacter, 1 case of Staphylococcus epidermidis + Enterobacter cloacae.
On average, the duration of treatment in the ICU was 2.6 days in the main group, and 3.9 days in the comparison group. The total average bed-day was 8.9 days in the main group, and 13.7 days in the comparison group. Lethal cases in the comparison group - 2, main - 1.
Thus, the prophylactic use of PVBP and OW made it possible to adjust the enteral pathobiome, as well as the level of pathogen contamination of the small intestine. We associate the decrease in the level of contamination by Clostridium isolates with the effects of the OW. Of course, studying water - the most common substance on earth - is not an easy task. There are previously published scientific works on the effectiveness of OW in anaerobic infections [15]. Probably, one of the effects of OW is the creation of unfavorable conditions for the growth and reproduction of obligate anaerobes. The number of SSI in the main group decreased by more than 2 times. Taking into account the results of the research, there is an urgent need for the development and clinical application of new phages, in particular against Citobacter and Acinetobacter.
The results suggest that the prophylactic use of PVBP and OW may represent an approach to preserve intestinal barrier function, block the entry of pro-inflammatory triggers into the portal system, and prevent intestinal systemic inflammation-induced microbial translocation. Complex interactions of bacteriophages, oxygenated agents and pathogens against the background of immunological deficiency are difficult to model and study, however, in our opinion, further multicenter studies and meta-analyses will be a promising direction in the fight against SSI.
Enteral and local application of PVBP and enteral use of OW in emergency abdominal surgery allows to normalize the induced enteral pathobiome, to reduce pathogen contamination and to arrest intestinal insufficiency at an earlier time and reducing the risk of SSI by more than 2 times.