- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 4: e1. DOI 10.35630/2199-885X/2022/12/4.7
When treating patients with COVID-19, prognostic and diagnostic tests to assess the risk of severe disease and adverse outcome are particularly important. The analysis of demographic, clinical, laboratory and instrumental data obtained on ICU admission was performed on a sample of 109 patients to determine potential predictors of lethal outcome. The factors increasing the risk of adverse outcome included age ≥57 years (AUC = 0.777, P < 0.001), hypertension (RR = 3.073, P = 0.033), ARDS (RR = 17.455, P < 0.001), advanced chest CT severity score (HR = 1.569, P = 0.039), severe and critical COVID-19 (RR = 6.964, P = 0.016), neutrophilia (AUC = 0.729, P = 0.005), lymphopenia (AUC = 0.705, P = 0.023), thrombocytopenia (AUC = 0.713, P = 0.018), reduced MCHC (AUC = 0.700, P = 0.026), elevated RDW (AUC = 0.718, P = 0.007), LDH (AUC = 0.891, P = 0.005) and D-dimer (AUC = 0.806, P = 0.029).
Keywords: COVID-19, Mortality, ICU, Predictors
When treating inpatients diagnosed with COVID-19, prognostic and diagnostic tests are particularly important to assess the risk of a severe disease and adverse outcome ant to develop approaches for improving survival. Demographic, clinical, laboratory, and instrumental data on admission should always be taken into consideration [1]. As of May 2022, there are more than six million COVID-19 related deaths worldwide (https://covid19.who.int). Mild presentation occurs in approximately 80% of persons with COVID-19, whereas moderate to severe disease is seen in about 14% of cases, and critical illness was reported in 5% of those infected [2]. Patients with severe manifestations may require admission to an intensive care unit (ICU) [3]. COVID-19 can underlie such critical conditions as severe interstitial pneumonia, acute respiratory distress syndrome, sepsis, pulmonary embolism and directly or indirectly cause cardiovascular and neurological complications [4]. The analysis and identification of predictors of outcome in the ICU will help to assess patients' risks and make appropriate clinical decisions [5]. The aim of the study was to find predictors of fatal outcome in patients with COVID-19 admitted to the ICU.
The study included patients diagnosed with COVID-19 and admitted to the ICU of M.F. Vladimirsky Moscow Regional Clinical Hospital, Moscow Clinical Center for Infectious Diseases "Voronovskoye”, and N.V. Sklifosovsky Scientific Research Institute of Emergency Medicine from April to October 2020.
The study sample, as well as the inclusion and exclusion criteria, have been described in detail previously [6]. The total sample (n=109) consisted of patients discharged from ICU in stable condition (n=90) and patients with fatal outcome (n=19).
Statistical analysis of the data was performed using IBM SPSS Statistics 25.0 software. Risk of adverse outcome in univariate analysis was assessed using relative risk (RR) and its 95% confidence interval for each studied predictor. To assess the performance of various quantitative parameters as predictors, we used ROC analysis with estimation of the AUC (area under curve) value. The cut-off value was chosen based on the optimal sensitivity/specificity ratio according to the results of ROC analysis. To identify the possible influence of various factors on the time of lethal outcome in patients with COVID-19, survival curves were analyzed using the Kaplan-Meier method with the evaluation of the significance of differences in the log-rank test.
Demographic, clinical, and laboratory data considered as potential predictors of fatal outcome in patients with COVID-19 are shown in Table 1.
Table 1. Clinical and laboratory data of patients with COVID-19
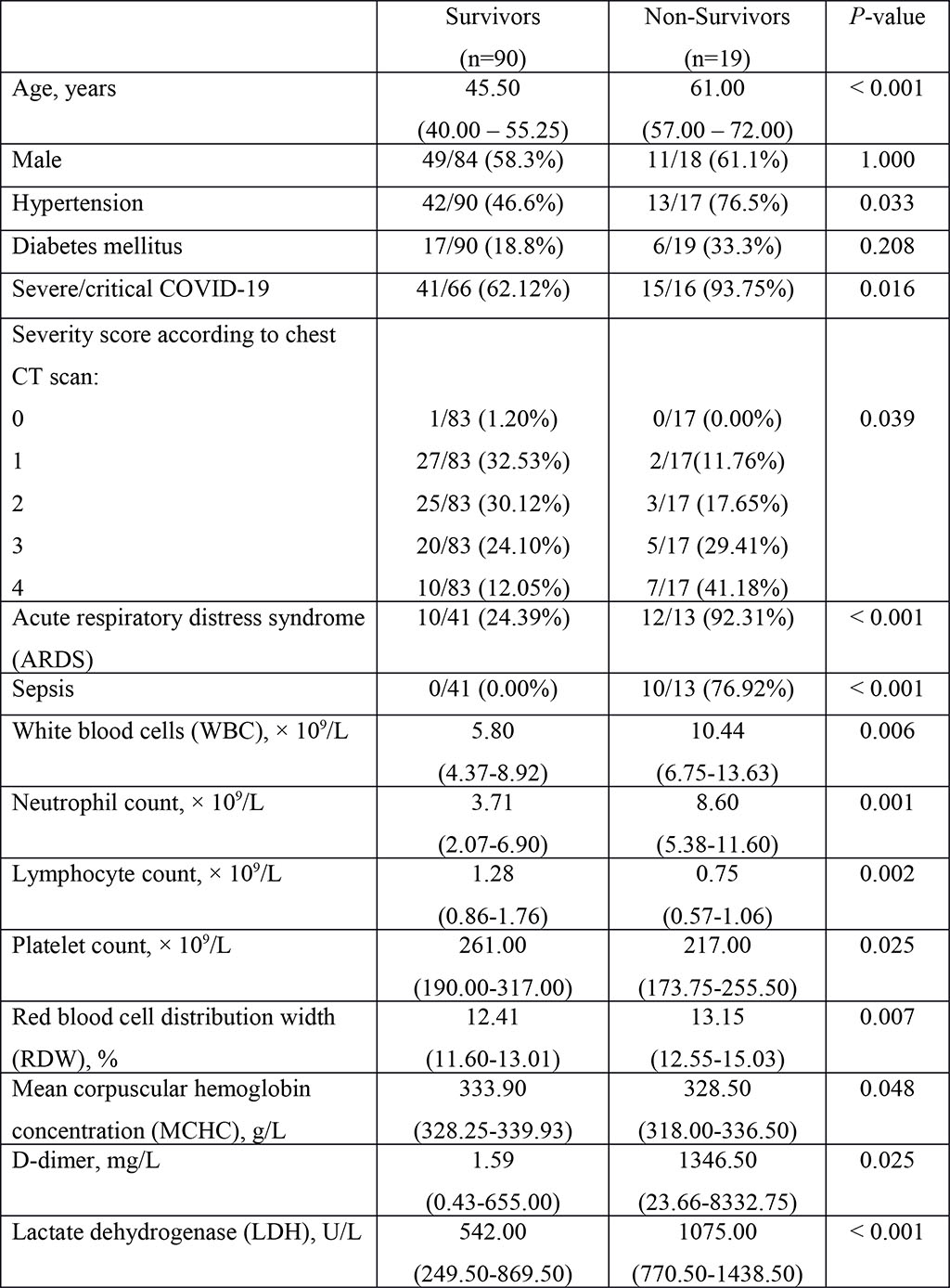
The data are presented as median and interquartile range (25–75th percentiles) or as percentage (%) of total number of patients with available data. P-values comparing survivors and non-survivors were calculated using the two-sided Fisher exact test or Mann-Whitney U test.
Type 2 diabetes mellitus and hypertension were considered when assessing the impact of comorbidities on the risk of adverse outcome in patients with COVID-19. Mortality rate was not associated with the number of comorbidities (Fisher's exact test, P = 0.061) or with history of type 2 diabetes mellitus (Fisher's exact test, P = 0.208). Patients with COVID-19 who had a history of hypertension were significantly (3 times) more likely to have an adverse outcome, with 23.6% of patients with hypertension dying versus 7.7% of patients without a history of hypertension (Fisher exact test, P = 0.033; RR = 3.073 [95% CI: 1.070-8.821]). Patients with COVID-19 who had a severe/critical disease on admission also had a higher risk of adverse outcome (Fisher exact test, P = 0.016; RR = 6.964 [95% CI: 0.971-49.944)]. The proportion of COVID-19 patients who died significantly grew with increasing chest CT severity score (according to the semiquantitative visual scale) (P = 0.039). With each 1-point increment in CT severity score, the risk increased by 56.9% (Cox regression analysis, HR = 1.569 [1.074 - 2.527]). The Kaplan-Meier survival curve analysis for CT severity is shown in Figure 1. Patients with COVID-19 who developed ARDS had more than 15-fold higher risk of mortality (Fisher exact test, P < 0.001; RR = 17.455 [95% CI: 2.443-124.722]), and the risk of adverse outcome increased 14.7-fold if sepsis developed (Fisher exact test, P < 0.001; RR = 14.667 [95% CI: 4.920-43.725]).
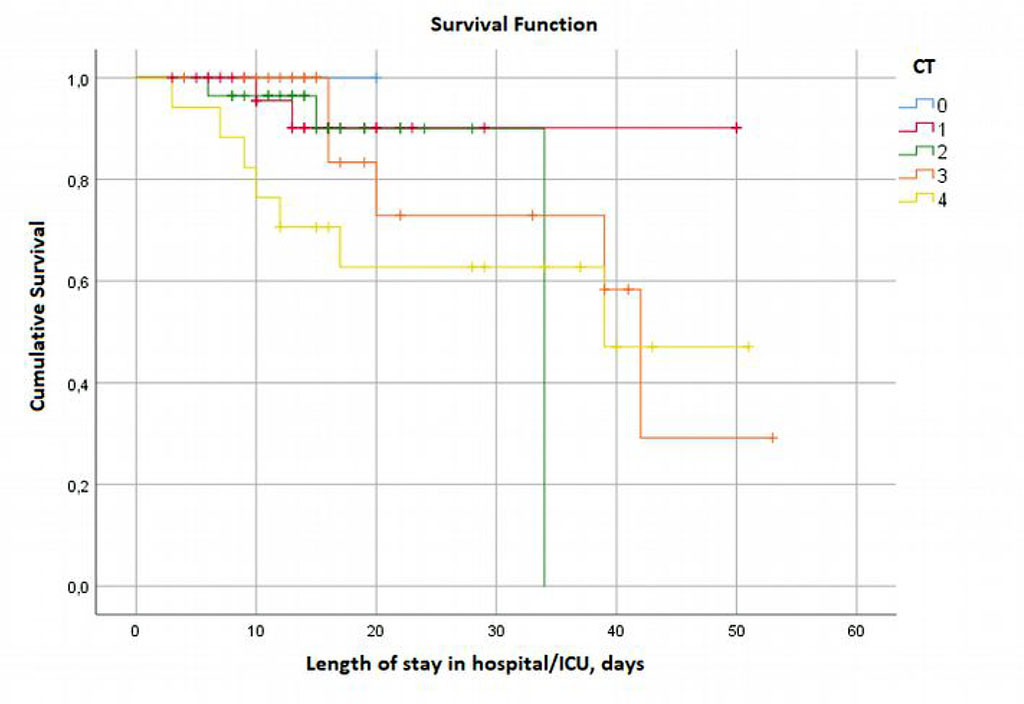
Figure 1. Kaplan–Meier survival curve for CT severity score.
The evaluation of performance of specific factors in predicting lethal outcome was performed only for those parameters that differed significantly between the groups of survivors and non-survivors. The results of ROC analysis for clinical and laboratory data considered as potential predictors of lethal outcome in COVID-19 are shown in Table 2. Patient age on admission was a significant predictor of mortality (AUC = 0.777, P < 0.001). Several laboratory parameters which were elevated on admission to the ICU and showed significant correlation with adverse outcome in ROC analysis included white blood cell count (AUC = 0.679, P = 0.028), neutrophil count (AUC = 0.729, P = 0.005), and RDW (AUC = 0.718, P = 0.007). Reduced lymphocyte count (AUC = 0.705, P = 0.023), platelet count (AUC = 0.713, P = 0.018), and MCHC (AUC = 0.700, P = 0.026), as well as elevated LDH (AUC = 0.891, P = 0.005) and D-dimer (AUC = 0.806, P = 0.029) levels were also significant predictors of lethal outcome.
Table 2. ROC-analysis of mortality predictors in COVID-19 patients
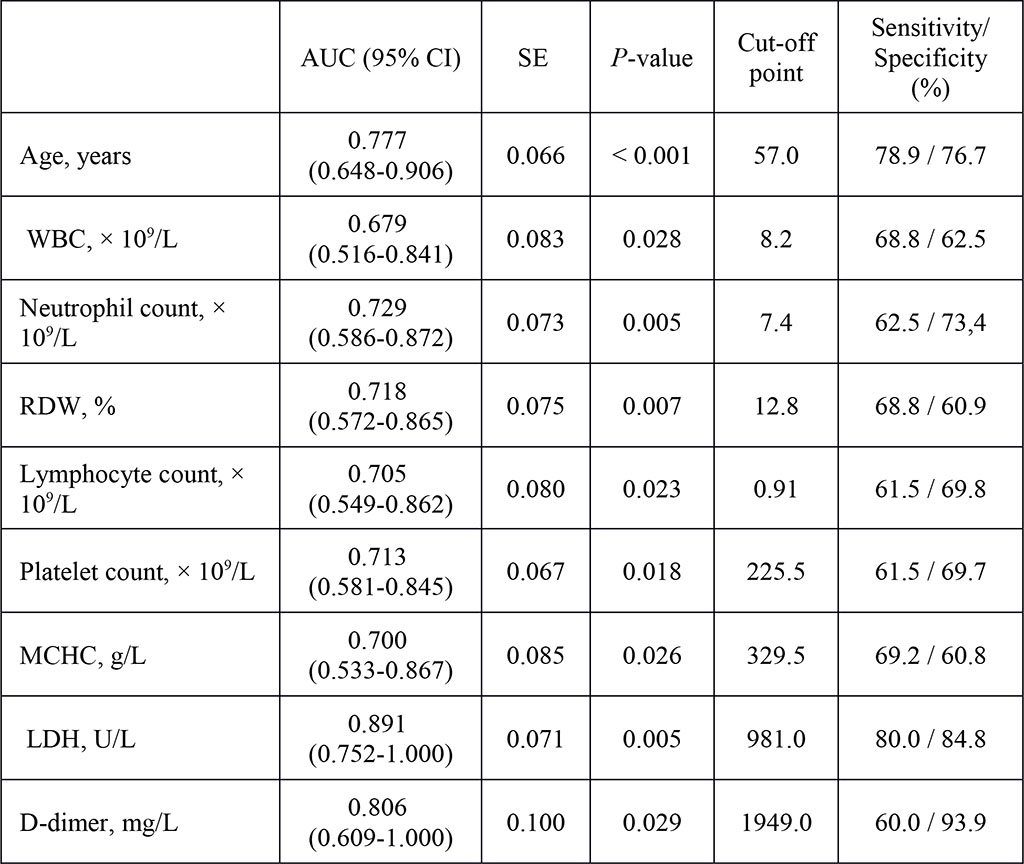
AUC – area under curve; LDH – lactate dehydrogenase; MCHC – mean corpuscular hemoglobin concentration; RDW – red blood cell distribution width; SE – standard error; WBC – white blood cells.
We studied demographic, clinical and laboratory parameters as potential predictors of fatal outcome in COVID-19. All significant predictors are demonstrated in Figure 2. Age and laboratory data obtained upon patient admission were analyzed using ROC-analysis. Notably, the higher the AUC value, the better is the performance of this parameter in predicting the outcome. According to a widely accepted classification, an AUC of less than 0.7 is of low significance, 0.7 to 0.8 is of medium significance, and over 0.8 is of high significance. In our study, the AUC for WBC was less than 0.7; the highest AUC values were found for age (0.777), LDH (0.891), and D-dimer (0.806). A history of hypertension, development of ARDS and sepsis in COVID-19, severe/critical disease, and advanced CT severity increased the risk of death.
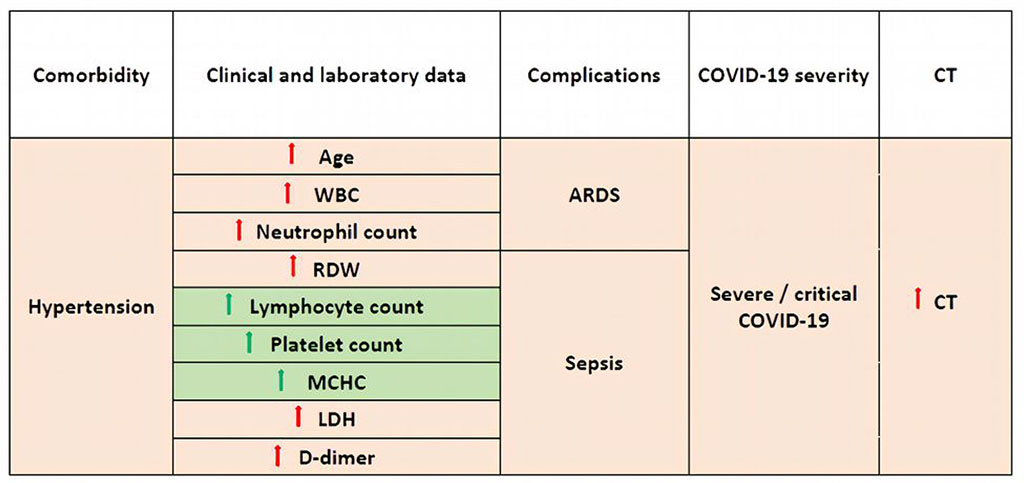
Figure 2. Significant predictors of mortality in COVID-19 patients. Factors increasing the risk of death are marked red, protective factors reducing the risk of death are marked green.
In a multicenter retrospective study involving 1116 patients, C-reactive protein, age, and tachycardia were identified as predictors of COVID-19 mortality; hypertension did not increase the risk of adverse outcome [5]. In our study, the age threshold increasing the risk of mortality was 57 years. Although the association of COVID-19 outcome with age has been repeatedly confirmed [7, 8, 9], the age threshold varies across the studies. Thus, in our study, it was 57 years, while other researchers found it to be 65 years or older [10]. Data from meta-analysis revealed that hypertension was independently of other factors associated with a significantly increased risk of critical COVID-19 (1.82-fold) and in-hospital mortality from COVID-19 (2.17-fold) [11]. More than 60% of patients admitted to ICU with COVID-19 are reported to develop ARDS [12, 13]. According to our data, COVID-19 patients with ARDS had more than 15 times higher risk of fatal outcome than patients without ARDS. Several studies have shown that more than 80% of critically ill patients with COVID-19 suffer from lymphopenia with underlying neutrophilia [14, 15]. Elevated LDH levels are associated with a 6-fold increase in the risk of severe disease and a 16-fold increase in the risk of mortality in patients with COVID-19 [16]. LDH is one of the biomarkers associated with adverse outcomes in other viral infections as well (influenza, adenovirus, respiratory syncytial and other viruses) [17]. B.H. Foy et al. have shown that elevated RDW on hospital admission and during treatment increases the risk of fatal outcome in patients with COVID-19 [18]. Multivariate logistic analysis has demonstrated that elevated RDW on admission was associated with a more than three-fold increase in the risk of adverse outcome in hospitalized patients with COVID-19 [19]. Patients with COVID-19-induced pneumonia demonstrate clotting disorders, elevated fibrinogen and D-dimer levels, often with mild thrombocytopenia and prolonged prothrombin time [20, 21]. According to F. Zhou et al. D-dimer level above 1 μg/mL increases the risk of fatal outcome by more than 18 times [22].
We have revealed potential predictors of fatal outcome and evaluated their performance among patients with COVID-19 hospitalized in the ICU. Age, hypertension, development of ARDS, advanced chest CT severity score, severe and critical COVID-19 disease, neutrophilia, lymphocytopenia, thrombocytopenia, reduced MCHC, elevated RDW, LDH and D-dimer were identified as factors increasing the risk of adverse outcome.
The reported study was funded by RFBR according to the research project 20-04-60352.