- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 4: e1. DOI 10.35630/2199-885X/2022/12/4.4
The large amount of papers on studying severe COVID-19 predictors have been published so far, but unfortunately the identified criteria are not universal for different regions of Russia and for the whole world. Therefore, a decision was made to apply routine research methods and compare the criteria previously proposed by other researchers with the criteria identified by us in patients living in Astrakhan Region. The study aimed at searching for and analyzing clinical and laboratory predictors to improve prediction of severe COVID-19 in men and women of different age groups. Materials and methods. Medical records of 361 patients were used as clinical material to conduct a retrospective study. Four groups with sex and age differencies were formed to verify the factors aggravating the course of COVID-19. Examination was performed according to Version 9 of the Temporary Guidelines for Prevention, Diagnosis and Treatment of the Novel Coronavirus Infection (COVID-19). Results. Clinical evidence on admission included unspecific complaints typical of other acute respiratory diseases – generalized weakness, temperature rise over 37.5° C, dyspnea, dry cough, and compressing pain. The spectrum of comorbid diseases includes hypertension, congestive heart failure, coronary heart disease, diabetes mellitus, and obesity. Conclusions. Delayed hospitalization of patients from the day of disease onset due to nonspecific COVID-19 symptoms is one of the unfavorable clinical predictors. Comorbidities that aggravate the course of COVID-19 are consistent with the comorbid conditions identified by other researchers [1,2]. High levels of procalcitonin, D-dimer, brain natriuretic peptide, lactate dehydrogenase and blood creatinine were identified as the most significant predictors of severe COVID-19 on admission, which is also consistent with the findings of other authors. Laboratory parameters like alanine transaminase > 45 u/l and aspartate transaminase > 55 u/l can be used for male patients aged 55 and older, while an increased leukocyte count > 7.4 ×109/l and C-reactive protein > 82 g/l – for female patients aged 55 and older.
Keywords: COVID-19, coronavirus disease, comorbidity, age, severe course predictors, prognosis, gender specificity.
The SARS-CoV-2 2019 (COVID-19) pandemic has been a rapidly evolving global challenge that keeps putting pressure on healthcare systems [3].
The disease is mild or asymptomatic in most patients, but the course of the pathological process in some individuals may become complicated and lead to ITU admission or death. Numerous studies aimed at developing the best possible management tactics for COVID-19 patients, in particular at determining diagnostic criteria for predicting severe course in order to provide timely care for this patient cohort, are being conducted nowadays [1, 2].
Despite numerous papers on studying predictors of severe COVID-19, there are no universal prognostic criteria that would be suitable both for Russian regions and for the whole world. The study compares previously proposed criteria [1, 2, 3] with the criteria identified in the studied cohort of patients living in Astrakhan Region.
To improve prognosis of severe COVID-19 in men and women of different age groups through a search for clinical and laboratory predictors.
A retrospective study in patients with the confirmed COVID-19, hospitalized at the Infectious Disease Departments of Kirov Municipal Clinical Hospital No.3 (Astrakhan, Russia) was carried out in the period from December 17, 2020 to February 28, 2021.
Medical records of 361 patients (mean age – 66.58±12.52 years), admitted to the medical institution on day 7 [5;9] from the disease onset due to deterioration of their health against ineffective outpatient treatment, were used as clinical material of the study. They were admitted to the hospital in compliance with the criteria stipulated by Order No. 198n “On Temporary Procedure of Arranging Work of Healthcare Organizations for Taking Measures to Prevent and Mitigate the Risk of COVID-19 Spread” of the Ministry of Health of Russia dated March 19, 2020. The main symptoms of which are SpO2 ≤ 95%, body temperature ≥ 38°C, RR>22, signs of pneumonia with the prevalence of ground-glass changes in both lungs of more than 25% (if there are chest CT results), comorbidities, the age of 65 and older, a positive COVID-19 test or contact with a COVID-19 patient [1, 2].
Four groups were formed by sex and age differences to verify the factors aggravating the course of COVID-19: group 1 – men aged 55 and older, group 2 – women aged 55 and older, group 3 – men under 55 years of age, and group 4 – women under 55 years of age.
Groups 1 and 2 included 114 men (31.58%) aged 70.04 ± 7.54 years, admitted on illness day 7 [4;9], the average length of stay was 8.5 [7;10] bed days (b/d), and 187 women (51.8%), aged 71.28 ± 8.93, admitted on illness day 6 [4;9], the average length of stay was 9 [8;11] b/d. The age of men and women in groups 1 and 2 did not differ significantly (p=0.100). Both groups were similar in terms of the number of days passed from the disease onset (p=0.129), but differed significantly in the length of stay (p=0.026).
The second pair of groups included 38 men (10.53%) under 55 years of age (44.5±7.36 years), admitted on day 7 [5;11] from the first signs of COVID-19, who stayed in the hospital for 8.5 [7;9.25] b/d, and 22 women (6.09%) under 55 years of age, (46.82 ± 5.2 years), admitted on illness day 7.5 [6;10], who stayed in the hospital for 9 [7;10.25] b/d. The age of men and women in groups 3 and 4 did not differ significantly (p=0.08). Both groups were similar in terms of the number of days from the disease onset (p=0.458) and the length of stay (p=0.32).
During the hospital stay, all the patients underwent a set of laboratory and instrumental examinations and treatment according to Version 9 of the Temporary Guidelines for Prevention, Diagnosis and Treatment of the Novel Coronavirus Infection (COVID-19). Chest CT was carried out with a SOMATOM go. UP scanner, SIMENS Helthineers.
Validity and integrity of the obtained results were confirmed through a sufficient number of observations and the use of universes and valid research methods [1]. Statistical analysis of the data was performed by methods of descriptive, parametric and nonparametric statistics using Microsoft Office Excel and Statistica 14.0 package (StatSoft, USA). Laboratory and instrumental data were presented as a median value with border quartiles [Q1;Q3]; the age was indicated as a mean value and standard deviation M±σ. Student’s t-test was applied to compare independent samples. The significance level for statistical hypothesis testing in the study was p<0.05.
When admitted to the hospital, the patients mainly complained of generalized weakness, temperature rise over 37.5° C, dyspnea, dry cough, and compressing pain, which suggests difficulty in early differential diagnosis of COVID-19 with other acute respiratory diseases.
The study results revealed some reasons accounting for not seeking timely medical care. The main reason was “I thought it was a common acute respiratory infection (ARI), so I self-treated,” – this answer covered 60.4% for both sexes. One-third of respondents (29.2%) thought that the illness would go away on its own, without any treatment, and 10.4% preferred to apply folk remedies at onset of disease. On the one hand, these circumstances indicate the similarity of early indicators of COVID-19 with ARIs and, on the other hand, they show that the patients underestimated their own condition and that the epidemiological alertness was lowered during the pandemic. The same pattern of reasons for not seeking timely medical care is traced by sex [1, 2].
CT results on admission showed that the volume of lump damage in the patients under study (n=361) was 37.12% for CT1 (< 25%), 52.08% for CT2 (25-50%), 9.42% for CT3 (50-75%), 1.11% for CT4 (>75%), and 0.27% for CT0 (no lung parenchyma damage). The average length of hospital stay was 9 [8;11] b/d. 33 patients died (9.14%), including 18 women (4.99%) and 15 men (4.15%).
The following forms of COVID-19 course were identified in group 1 based on CT results and objective evidence: moderate-to-severe – 81.58% (93 patients), severe – 17.54% (20 patients), extremely severe – 0.88% (1 patient); group 2: moderate-to-severe – 83.96% (157 patients), severe – 16.04% (30 patients); group 3: moderate-to-severe – 92.1% (35 patients), severe – 7.9% (3 patients); severe – 16.04% (30 patients); group 4: moderate-to-severe – 100% (22 patients). No significant differences in the volumes of lung damage were identified among the patients of all groups.
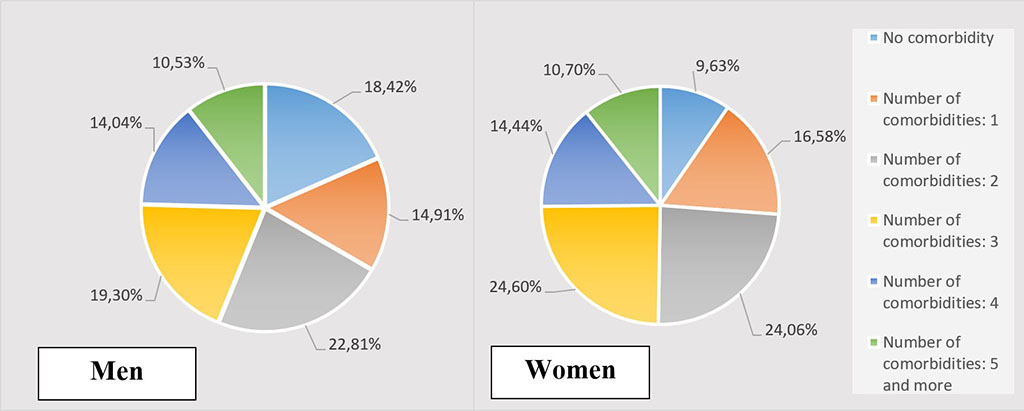
Figure 1. Quantitative ratio of a comorbid background in men and women aged 55 and older
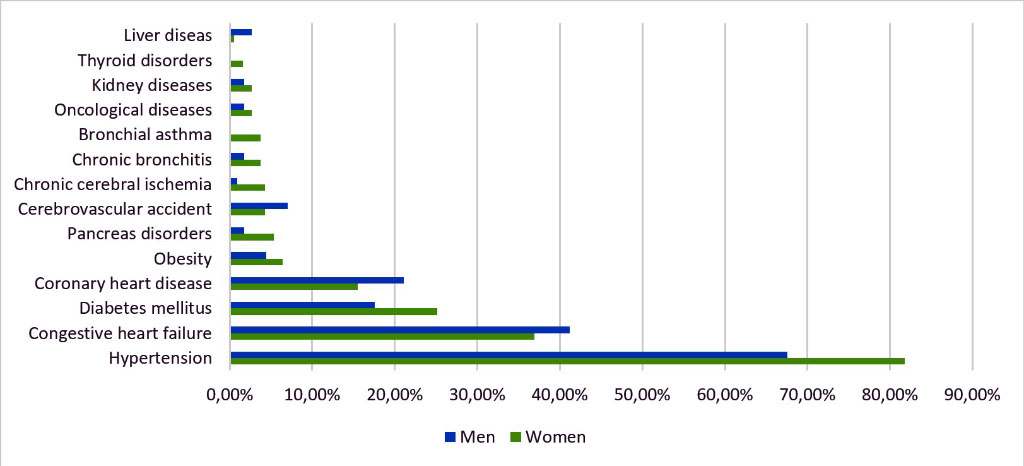
Figure 2. Frequency analysis of comorbidities in COVID-19 patients aged 55 and older
Most of the patients admitted with COVID-19 had comorbidities (83.1%). Patients with comorbidities accounted for 81.58% in group 1 and 90.37% in group 2 (Fig. 1). Hypertension (HT) was the leading co-morbidity (67.54% and 81.82% respectively) in both groups. Next came congestive heart failure (CHF) – 41.23% and 36.9%, respectively, followed by coronary heart disease (CHD) (21.05%) in group 1 and diabetes mellitus (DM) (17.54%) in group 2. Therefore, AH, CHD, IHD and DM were more common in the groups of patients older than 55 years (Fig. 2).
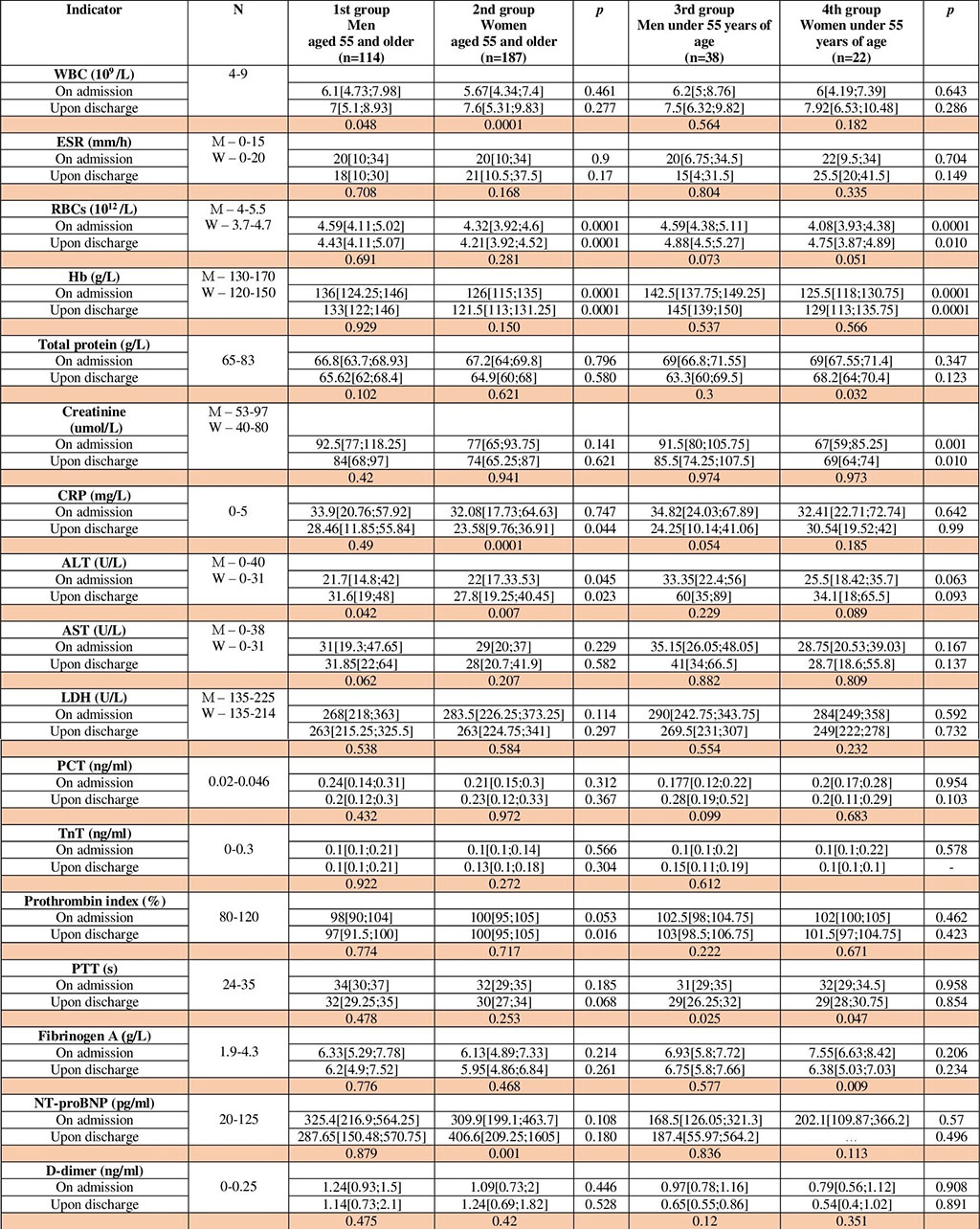
Table 1. Laboratory values of examined groups 1-4.
Comparison of the laboratory values of groups 1 and 2 (Table 1) showed that the level of erythrocytes and hemoglobin in group 1 was significantly higher than in group 2 both on admission (p<0.0001) and upon discharge (p<0.0001), which is consistent with specific traits of the female erythron system.
No significant differences in WBC level and erythrocyte sedimentation rate (ESR) between groups 1 and 2 were found on admission and upon discharge, but there was a tendency to an increase in WBC values within groups 1 and 2 over time (p=0.048 and p<0.001 respectively). In its turn, the level of C-reactive protein (CRP) significantly differed between groups 1 and 2 over time in the course of the treatment (p=0.044), and group 2 demonstrated a highly significant decrease of CRP in women (p<0.0001).
A significant increase in the values of alanine transaminase (ALT) was identified in the men of group 1 against the women of group 2 (p=0.045 and p=0.023 respectively). In the course of the treatment, there was a significant increase in ALT values in groups 1 and 2 (p=0.042 and p=0.007 respectively). The values of aspartate transaminase (AST) values did not change significantly over time.
Despite a significant 4.4-5-fold increase in D-dimer, a 5-10-fold increase in procalcitonin, and a 2-3-fold increase in fibrinogen values, no significant differences were found either between group 1 and 2 or within the groups on admission and upon discharge. The values of activated partial thromboplastin time (aPTT) and prothrombin index (PI) in groups 1 and 2 did not exceed the limits of the reference interval; PI was significantly lower in men upon discharge (p=0.016).
Heart failure is a major cause of death of COVID-19 patients and results from a variety of pathophysiological mechanisms, including as a direct damaging effect of SARS-CoV-2 on cardiomyocytes and endothelial cells. This can be proved by changes in such values as brain natriuretic peptide (NT-proBNP), lactate dehydrogenase (LDH) and troponin T (TnT). NT-proBNP level exceeded the norm by 2.5-3 times in both groups, increasing in the women of group 2 over time (p=0.001). LDH and TnT levels in both groups were above and within the upper limit of the reference values respectively, with no significant differences between groups 1 and 2 over time.
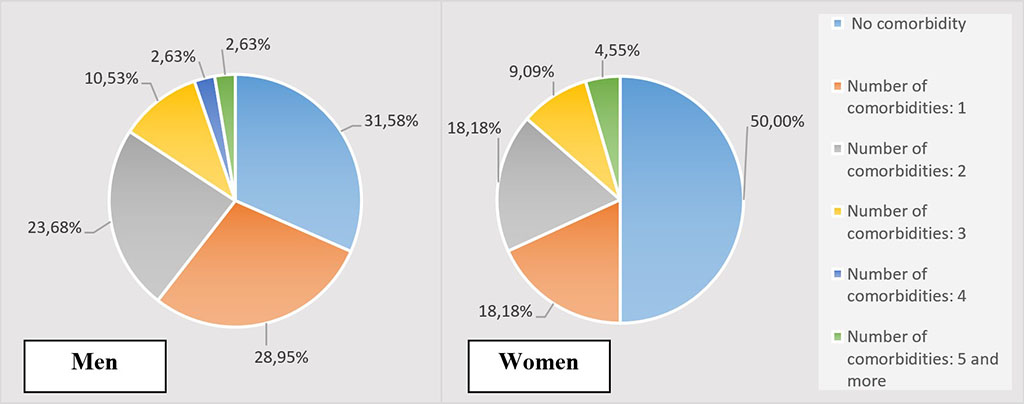
Figure 3. Quantitative ratio of comorbid background in men and women under 55 years of age
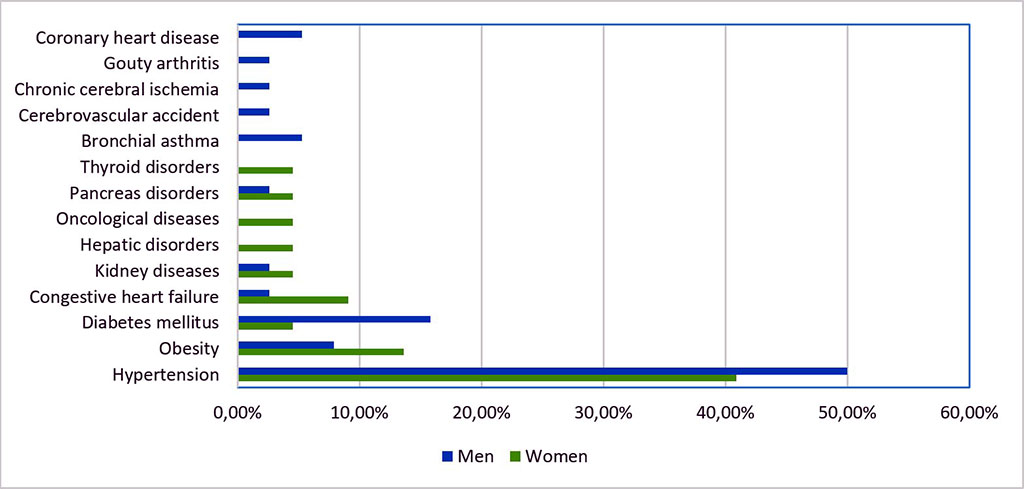
Figure 4. Frequency analysis of comorbidities in COVID-19 patients under 55 years of age
Patients with comorbidities accounted for 68.42% in group 3 and 50% in group 4 (Figure 3). HT prevails in both groups (50% and 40.91% respectively), followed by DM in group 3 (15.79%) and obesity in group 4 (13.64%). The 3rd place is taken by obesity in group 3 (7.89%) and CHF in group 4 (9.1%). Therefore, men and women under 55 years of age were more likely to have a combination of HT, obesity, DM, and CHF (Fig. 4).
There were statistically significant differences in the levels of RBCs (p=0.0001) and Hb (p=0.0001) on admission in groups 3 and 4 (Table 1). A similar picture was observed upon discharge – RBCs (p=0.010) and Hb (p=0.0001), which corresponds to the gender characteristics of erythron functioning. In the course of the COVID-19 treatment, there was a tendency of an increase in RBC count in both men (p=0.073) and women (p=0.051) under the age of 55.
No statistically significant differences in the values of WBCs, ESR and CRP in the groups were identified. Creatinine levels in both groups on admission and over time remained within the reference values, but the level of creatinine in men was significantly higher than in women both on admission and over time (p=0.010 and p=0.001 respectively).
LDH level in both groups exceeded the norm by 1.3 times without significant gender differences. A tendency of an increase in the values of liver transaminases was revealed in both groups in the course of the treatment, being more pronounced in the men of group 3. A fivefold increase in PCT levels was detected in both groups, both on admission and in the course of the treatment, without significant gender differences.
A 2.2-3.9-fold increase in the level of D-dimer, a 1.5-1.7-fold increase in the level of fibrinogen and the absence of deviations in PTI and PLT count at the initial stage of the disease differ COVID-associated coagulopathy from coagulopathies caused by bacterial sepsis and disseminated intravascular coagulation [6, 7] and is a poor prognostic factor for thrombotic complications [8-12]. Despite an increase in the levels of D-dimer and fibrinogen in patients under 55 years of age, a statistically significant decrease is observed only for fibrinogen in the course of the treatment of women (p=0.009). Fibrinogen is a precursor of the primary substrate of fibrin thrombosis and a protein of the acute phase of inflammation. An increased level of this protein is associated, on the one hand, with increased biosynthesis caused by its breakdown products in microthrombus formation, and on the other hand, with the disturbance of its catabolism in the lungs [13, 14].
The values of aPTT and PI as criteria of anticoagulant potential of the hemostasis system in the patient population did not exceed the reference limits [15, 16]. A significant decrease of aPTT in the course of the treatment was recorded both in men and in women (p=0.025 and p=0.047 respectively), which may be caused by specific features of the functional state of the liver.
The level of TnT in both groups remained within the reference limits over time, while NT-proBNP level exceeded the norm by 1.5 times in the whole course of the treatment without significant gender differences. Biomarkers of cardiac dysfunction are crucial for monitoring the progression of myocardial damage in COVID-19 patients. One of the most widely studied biomarkers is TnT which enters the bloodstream with cardiomyocyte damage. Guo et al. [5] reported that an increase in TnT level in the serum of patients with or without prior cardiovascular disease directly correlates with an increase in NT-proBNP level and is considered as an adverse prognostic factor [4, 5].
Comparison of the men of groups 1 and 3 revealed that RBC count, Hb concentration, the levels of ALT, PCT, and PI were significantly higher in patients under 55 years of age than in older patients. On the contrary, the levels of aPTT and D-dimer were significantly higher in patients aged 55 and older than in younger patients. Comparing the patients of groups 2 and 4, one can see that the concentration of fibrinogen on admission was significantly higher in women under 55 years of age, and it significantly decreased in the course of the treatment compared with older women. However, CRP significantly decreased, while NT-proBNP, on the contrary, increased in older women in the course of the treatment.
328 patients (90.86%) were discharged on the condition improved after combined therapy, and the number of deaths was 33 (9.15%). In group 1, 99 men (86.84%) were discharged and 15 (13.16%) died, with the latter having the length of stay of 7 [4;10] b/d and preadmission period of 8 [4;8] b/d. In group 2, 168 women (89.84%) were discharged and 18 (10.16%) died; the length of stay of the latter was 7.5 [4.5;13.5] b/d, and the preadmission period 7 [5.75;9.5] b/d. In the 3rd and 4th groups 38 men (100%) and 22 women (100%) respectively were discharged.
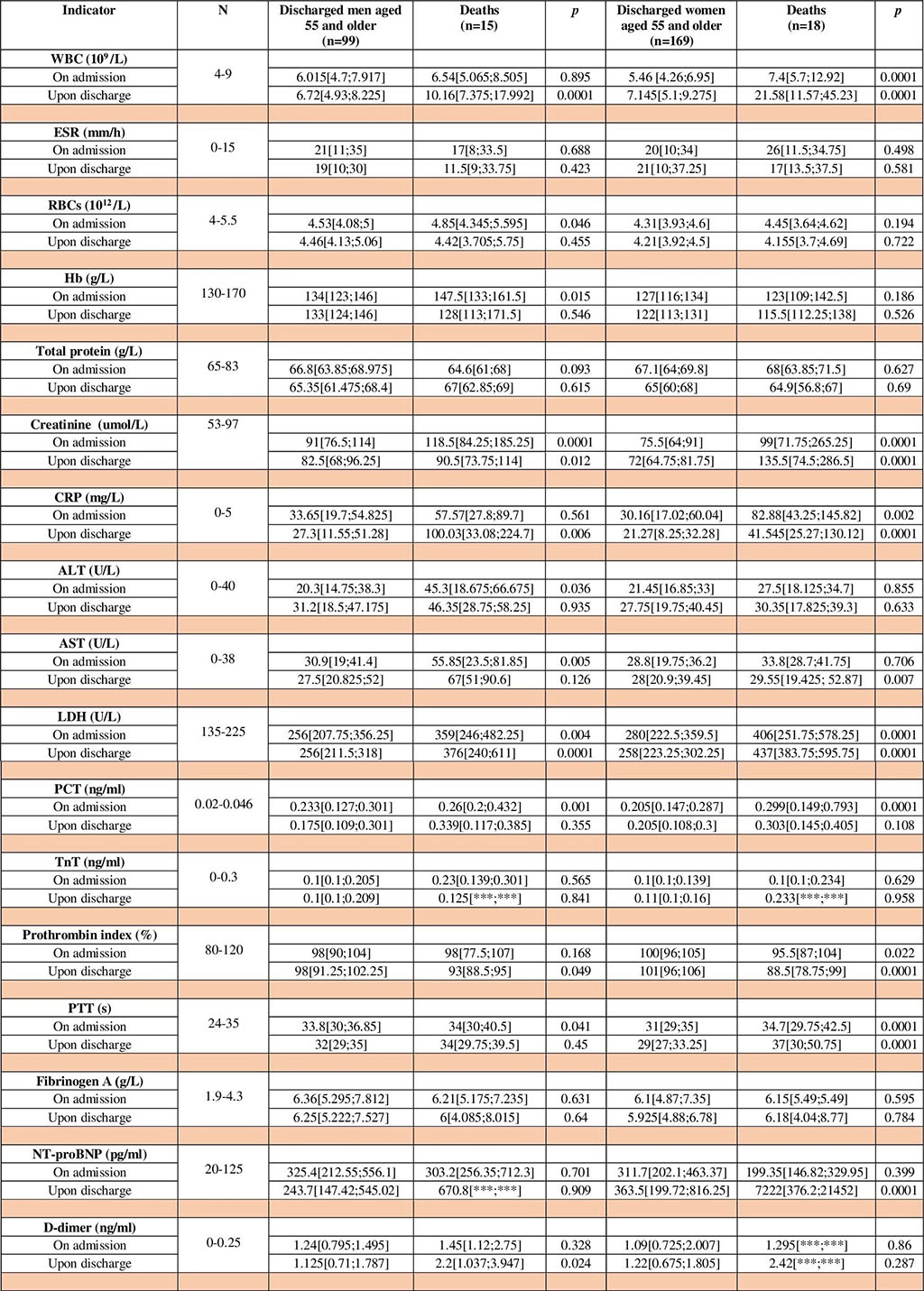
Table 2. Laboratory values of men and women aged 55 and older, discharged and fatal cases
Analysis of the comparative dynamics of the laboratory values in the patients depending on the outcome (Table 2) allowed to make an attempt to specify unfavorable prognosis criteria that are common for men and women, including increased CRP (11-17 times higher than the norm), PCT (6-6.5 times), LDH (1.6-2 times), creatinine (1.2 times), and D-dimer (4.4-5 times) on admission and a dramatic increase in NT-proBNP (5-50 times) in the course of the treatment, particularly in women.
Women older than 55 years have a more pronounced inflammatory response than men, which is confirmed by significantly high values of CRP (p=0.002) and WBC count (p=0.0001), unlike men, who have the prevailing values of cytolysis and liver dysfunction – an increase in ALT (p=0.036) and AST (p=0.005).
Predictors of the adverse outcome in men aged 55 and older include:
Predictors of the adverse outcome in women aged 55 and older include:
It follows from autopsy pathology reports that men died of acute cardiopulmonary failure (ACPF) in 80% of cases, and in 20% of cases – due to cerebral ischemia. Death cases among women, associated with ACPF (39%) and cerebral ischemia (39%), and subsequently with cerebral edema, accounted for 78%; in the remaining 22% of cases, women died of multiple organ failure caused by DIC syndrome, among other things. This may be due to the nature of concomitant pathology in the patients admitted to the hospital. The most frequent comorbidities among COVID-19 death cases were HT – 60.6% of cases, CHF – 36.4%, CHD – 30.3%, and DM – 21.2%. The proportion of the combination of two or more comorbidities was 80% for death cases among men and 94.4% for death cases among women.
Delayed hospitalization of patients from the day of disease onset due to nonspecific COVID-19 symptoms is one of the clinical unfavorable predictive factors. Hypertension, congestive heart failure, coronary heart disease and diabetes mellitus are the most dangerous comorbidities in COVID-19 patients aged 55 and older, which is consistent with the results of other authors’ studies [1, 2].
Increased levels of PCT, D-dimer, NT-proBNP, LDH, and blood creatinine can be used as laboratory predictors of adverse prognosis regardless of sex, which is also consistent with the findings of other authors [2, 4-12]. In addition, it is proposed to take into account the levels of ALT > 45 u/l and AST > 55 u/l in men aged 55 and older, as well as an increased WBC count >7.4 ×109/l and increased CRP > 82 g/l in women aged 55 and older as predictors of unfavorable prognosis.
The results are heterogeneous, so there is a need for further research.
Ilfat Karimov developed the concept and design of the study, collected and processed the material, conducted the study, carried out statistical analysis, drew up the text, visualized the content, and approved the final version of the paper.
Samat Ikhsanov collected and processed the material, conducted the study, carried out statistical analysis, drew up the text, and approved the final version of the paper.
Olga Dyakova edited the study design, edited the text (provided critical revision, making valuable intellectual comments), and approved the final version of the paper.
Alexey Demidov edited the text (provided critical revision, making valuable intellectual comments) and approved the final version of the paper.