- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 3. DOI 10.35630/2024/14/3.338
We present a clinical case that reflects the effectiveness of eversion carotid endarterectomy in a patient with complete blockage of the carotid arteries. A 62 y.o. patient was admitted to the clinic with complaints of dizziness and syncopal events such as “blackouts” when turning his head to the side. Angiography revealed that the right external carotid artery is stenotic up to 85%, the internal one is up to 90%, and the circle of Willis is closed. Endarterectomy was performed from the common carotid, internal carotid and external carotid arteries, with their complete cutting off and subsequent plastic suturing, i.e. formation of a trifurcation anastomosis. As shown in control angiography, the patency of the carotid segment was completely restored, and there was no neurological deficit.
Keywords: eversion carotid endarterectomy, carotid atherosclerosis, transcranial duplex scanning, angiography, neurological deficit
Currently, about 9 million people in the world suffer from cerebrovascular diseases, the main place among which is held by stroke. Each year, cerebral stroke affects 5.6 to 6.6 million people and claims 4.6 million lives. The annual mortality rate from strokes in the Russian Federation is one of the highest in the world (175 cases per 100 thousand) [1-4].
In the last decade, stroke has become the second leading cause of death, second only to coronary heart disease [5, 6]. Carotid arteries affection by the atherosclerotic process causes a high risk of ischemic stroke, which is directly proportional to the degree of stenosis. In the Russian Federation, the incidence of cerebrovascular diseases is increasing everywhere. The mortality rate from this pathology in Russia is 25%, giving way to mortality from acute myocardial infarction, and in 24.3% of all cases, pathological deformation of the internal carotid artery is detected [7-11].
The results of large multicenter studies (NASCET, ECST, ACAS) showed the advantage of carotid endarterectomy (CEA) in asymptomatic and symptomatic patients with a high (70–99%) degree of stenosis of the internal carotid artery (ICA) compared with conservative treatment [12, 13]. Multifocal atherosclerosis simultaneously affecting the carotid arteries, coronary vessels, renal and peripheral arteries is observed in 30-65% of cases. The severity of coronary atherosclerosis, according to the Gensini scale, statistically significantly correlates with the presence of atherosclerotic plaque (AP) in the carotid artery (CA), its location, and IMT (intima–media thickness) above 0.9 mm [14].
Carotid endarterectomy (CEA) is a recognized standard of surgical treatment for patients with carotid artery stenosis. The annual frequency of this operation continues to increase steadily. Although the acceptable quantitative limits of cardiovascular events for the institution in which a given operation is performed are well known, the potential incidence of restenosis in the hospital and long-term periods is often not studied. Restenosis (stenosis greater than 50%) of the internal carotid artery (ICA) remains the main lesion of the carotid arteries. This condition can occur with a frequency of up to 36% in the yearlong postoperative observation period [15, 16].
The purpose of the study was to describe a clinical case reflecting the effectiveness of eversion carotid endarterectomy in a patient with complete blockage of the carotid arteries.
Patient M., 62 y.o., is admitted to the clinic with complaints of dizziness and syncopal events such as “blackouts” when turning his head to the side. The complaints appeared gradually, increasing clinically every year.
Consciousness is clear. No meningeal signs. Cognitive functions are slightly reduced. Symptoms of oral automatism D, S. Right-handed. Emotionally labile. Pupils D=S. The reaction of the pupils to light is lively. Movement of the eyeballs is limited outward. Convergence is weakened. Nystagmus and diplopia are not defined. Slight asymmetry of nasolabial folds. The pharyngeal reflexes are reduced, D=S. Slight deviation of the tongue to the right. The muscle tone of the limbs is increased in 'pyramidal' pattern, D>S. Tendon reflexes are increased in 'pyramidal' pattern, D>S. Babinski and Rossolimo signs D et S, D>S. The Romberg test shows staggering. Coordinating tests: intention tremor and past-pointing D et S. Controls pelvic functions.
EEG records moderate cerebral changes with flattening of biorhythms; irregular sharpened α-rhythm; sharply smoothed zonal differences; reduced activation response; bilaterally synchronous flashes of low-amplitude sharp waves in the background recording when opening and closing the eyes, during hyperventilation, in the background after hyperventilation. No typical epileptiform activity is detected. Fig. 1.
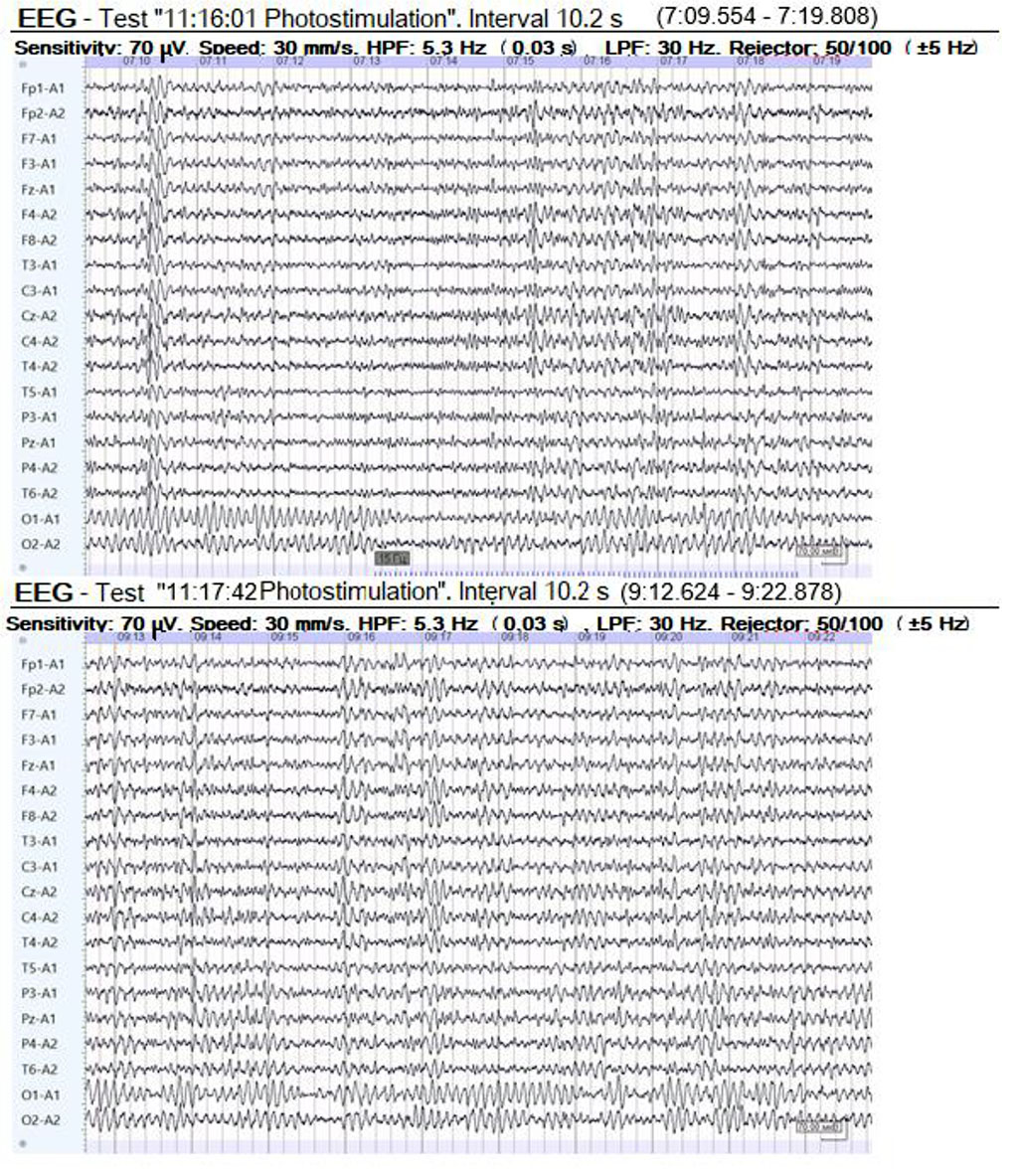
Figure 1. EEG of a patient with 85% stenosis of the right external carotid artery and 90% of the internal carotid artery
CT angiography revealed that the right external carotid artery is stenotic up to 85%, the internal one is up to 90%, and the circle of Willis is closed despite this. Fig. 2.
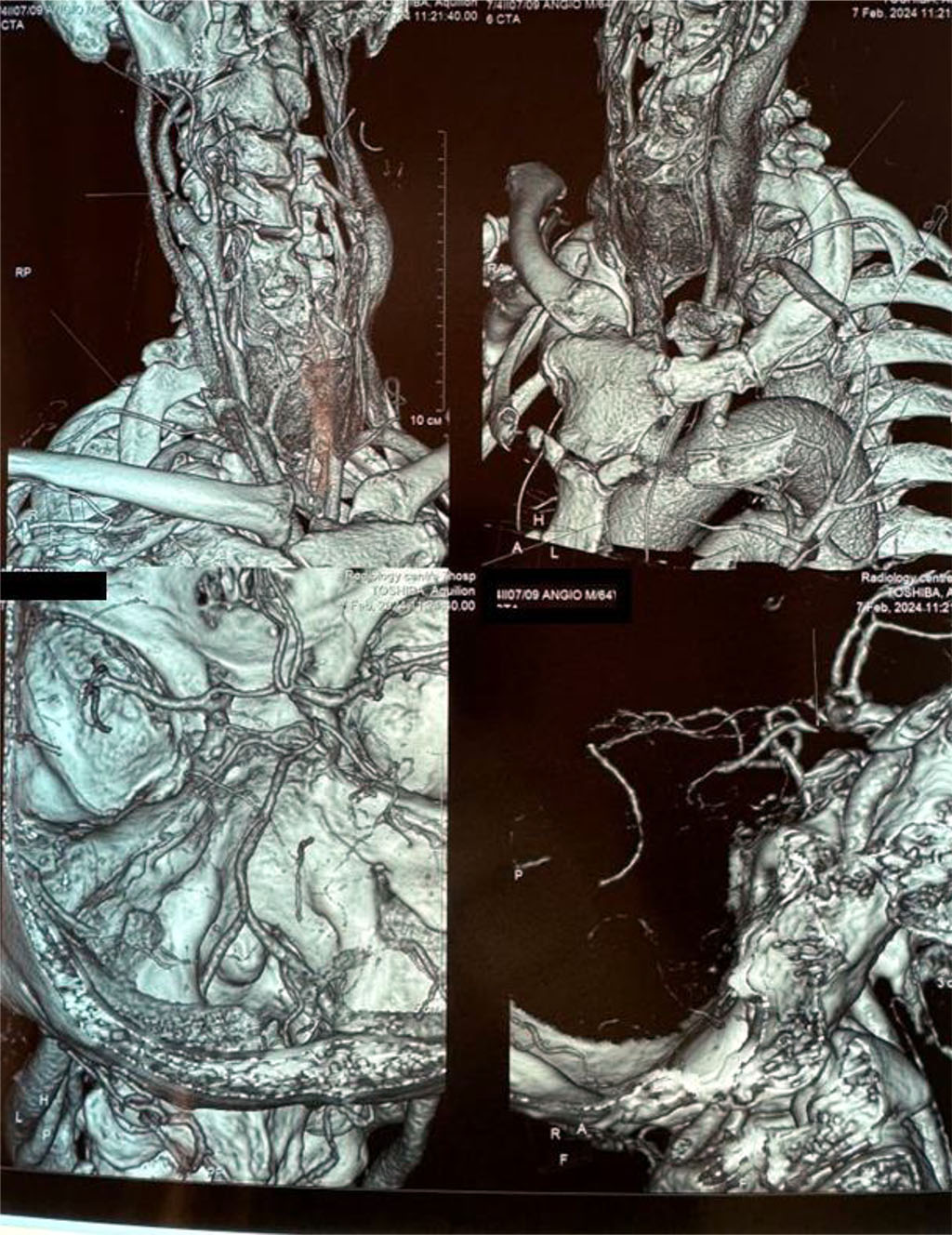
Figure 2. CT angiography (3D reconstruction) in a patient with 85% stenosis of the right external carotid artery and 90% of the internal carotid artery
The position of the patient during the operation: the head end of the operating table is slightly raised, the legs are slightly lowered. A cushion is placed under the patient's back, in the area between the shoulder blades, and the head is positioned so that the face is turned away from the operation site. A skin incision is made behind the earlobe, starting from the lower edge of the mastoid process, along the medial edge of the sternocleidomastoid muscle to the border between the middle and lower thirds of the neck. In the upper corner, the wound may pass through the sensory great auricular nerve, innervating part of the auricle and the posterior part of the parotid region. If possible, we preserve this nerve, but if necessary, it can be dissected. A good reference point to locate the internal carotid artery is the facial vein, which then crosses the wound and drains into the internal jugular vein. With the retrojugular approach, this reference point is absent. This vein must be isolated, sutured, ligated and then dissected. The hypoglossal nerve can pass over the initial part of the internal and external carotid arteries. N. reccurens arises from the glossopharyngeal nerve to form a cervical ring. The common carotid artery is isolated and fixed on a holder. Then 1.0 ml of 2% lidocaine solution is injected into the area of the carotid glomerulus to prevent bradycardia. The superior thyroid artery and then the external carotid artery are isolated and placed on holders one by one. The internal carotid artery is isolated and fixed last. All manipulations in the bifurcation area are performed extremely delicately, in order to avoid trauma and destruction of the atherosclerotic plaque.
To determine the need to use an internal shunt, we measure retrograde blood pressure in the common carotid artery, thereby assessing the linear velocity of blood flow in the middle cerebral artery using transcranial duplex scanning. Before clamping the arteries, the patient is given 5000 units of heparin intravenously. Systolic blood pressure is + 40 mm Hg from initial blood pressure.
First, we clamp the external carotid artery, then the internal carotid artery distal to the plaque + 1.5-2 cm and, finally, the common carotid artery. The clamp on the common carotid artery is placed parallel to the floor so that the side wall of the common carotid artery would be raised when the clamp is moved to a vertical position, which is convenient for subsequent arteriotomy.
After clamping all the arteries, we finally isolate the bifurcation of the common and internal carotid arteries without fear of destruction and fragmentation of the plaque and, consequently, embolism into the intracranial segment of the internal carotid artery.
To perform endarterectomy, we make an incision along the outer surface of the artery from the common carotid artery to the internal carotid artery. The incision should begin 1.5-2.0 cm proximally and end behind the visible edge of the plaque.
Endarterectomy begins from the common carotid artery. It is important not only to separate the plaque from the intima, but also to isolate the inner membrane by cutting the wall surrounding the outer elastic membrane subadventitially. I use a Varady miniphlebectomy dissector to separate the intima. In difficult cases, when the layers of the artery are not sufficiently separated, I use a regular injection needle. Endarterectomy is performed in both directions from the common carotid artery. Sometimes, for convenience, we divide the artery wall from behind with a thin dissector. After dividing the intima and media along the entire circumference of the artery, they are incised in a circle at the proximal corner of the arterial wound. The endarterectomy then goes on distally until the external carotid artery is exposed. To perform endarterectomy, the clamp is removed from the latter, the retainer of the superior thyroid artery is loosened, and the assistant uses forceps to bring the artery closer to the common carotid artery. This maneuver allows the surgeon to perform an endarterectomy from the external carotid artery under direct vision as a variant of eversion endarterectomy. After endarterectomy is completed, we must check the retrograde blood flow and also remove all intimal fragments. In our case, endarterectomy is performed from the common carotid, internal carotid and external carotid arteries, with their complete cutting off and subsequent plastic suturing, i.e. formation of a trifurcation anastomosis.
When performing endarterectomy from the internal carotid artery, it is very important to determine the apex of the plaque. If the apex of the plaque cannot be seen, the artery should be dissected distally and, if necessary, previously mobilized.
An important point of the operation is the completion of excision of the intima of the internal carotid artery. After endarterectomy, we must assure the absence of floating intima. Using a saline + heparin syringe and a large, blunt needle, we inject a powerful stream into the artery wall. Areas of moving intima are immediately visible; in this case, it is necessary to additionally circulate the floating intima or remove part of it. If visibility of this section of the artery is poor, then further dissection of the artery is necessary. In most patients, endarterectomy of the internal carotid artery can be performed, leaving a well-fixed, non-floating intima distally. In patients with severe diabetes mellitus, it is often impossible to complete endarterectomy in this way, and then the intima is fixed in the distal segment of the artery using a fixing suture with Prolen 7/0 thread.
To remove the remaining intima of the endarterectomy area, we use microswabs. Sometimes tweezers or a mosquito clamp are used to remove parts of the intima all the way around the entire circumference of the artery.
When closing the arteriotomic incision, we use a synthetic PTFE patch with a width of no more than 5 mm after applying sutures to prevent the development of an aneurysm in the reconstruction area.
Before suturing, we alternately remove the clamps from the external, internal and common carotid arteries. We rinse the arteries with saline solution with heparin. Then the application and tying of sutures is completed.
The clamps are removed from the artery in a following order: first, the clamp is briefly removed from the internal carotid artery. Once the artery is filled with retrograde blood, the internal carotid artery is re-clamped from the beginning (preferably using a bulldog) along with the patch to prevent embolization. Then the external carotid artery and the common carotid artery are released in the same order. When blood flow is restored, the “possible” blood clot will enter the external carotid artery. A few seconds after restoration of blood flow through the external carotid artery, remove the bulldog from the internal carotid artery. The wound is drained using Redon catheters through a contraincision with a silicone perforated tube no more than 5 mm in diameter. The platysma is sutured with 3/0 Vicryl thread separately with interrupted sutures, and an intradermal suture is placed on the skin with Prolen 5/0 thread.
Neurological status after surgical treatment shows significant positive dynamics. Consciousness is clear. No meningeal signs. Cognitive functions are preserved. Symptoms of oral automatism D, S. Right-handed. Emotional lability not defined. Pupils D=S. The pharyngeal reflexes are alive, D=S. The tongue is in the midline. The muscle tone of the limbs is preserved, D=S. Tendon reflexes are alive, D=S. Babinski and Rossolimo signs D et S, D>S. Romberg test: stable. Successfully passes coordination tests. Controls pelvic functions.
The patient was discharged from the clinic in a satisfactory condition. As shown in control CT angiography, the patency of the carotid segment was completely restored. Fig. 3.
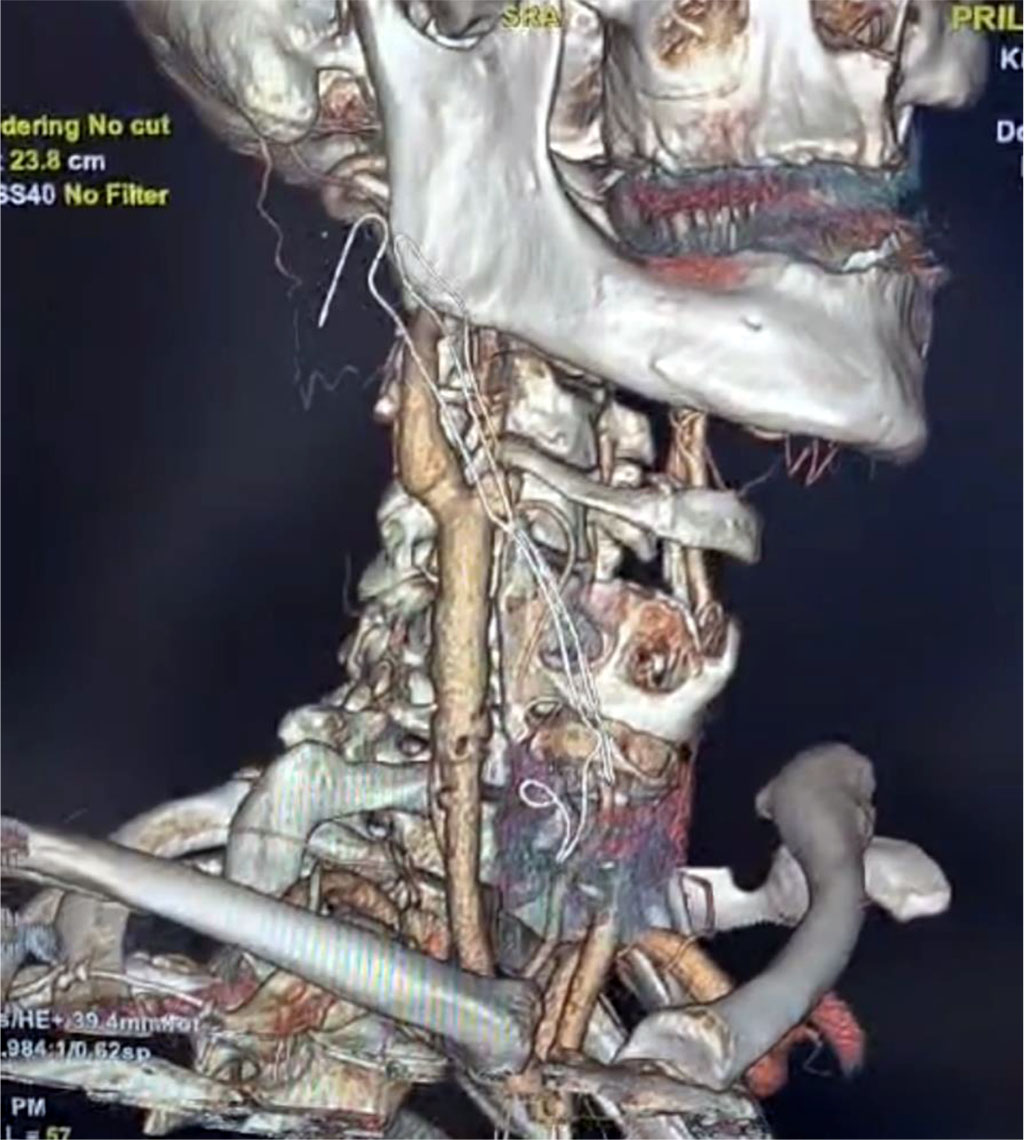
Figure 3. CT angiography (3D reconstruction) 2 weeks after surgery. The carotid segment is completely patent.
Thus, this clinical case demonstrates the positive impact of surgical treatment for completely blocked carotid arteries and positive neurological symptoms.