- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 3. DOI 10.35630/2024/14/3.337
We present a clinical case of treatment of pseudoaneurysm of the right brachial artery. The cause of the pseudoaneurysm was a gunshot wound to the right shoulder. An aneurysmectomy, endarterectomy, and autovenous prosthetic repair of the right brachial artery were performed. Histological examination revealed thrombotic masses, a fragment of the vessel wall with fibroblast proliferation, hemorrhages, focal hemosiderosis, and moderate lymphocytic infiltration. 6 months after surgery, limb function was completely restored. Autovenous prosthetic repair of a section of the brachial artery with a pseudoaneurysm due to a gunshot wound is an effective surgical method of treatment and restoration of blood flow.
Keywords: gunshot wound, brachial artery, pseudoaneurysm, aneurysmectomy, autovenous prosthetic repair
In the last decade, the number of military conflicts has been increasing, which increases the number of specific diseases associated with gunshot wounds of the great vessels [1-3]. False aneurysms of the upper limb arteries are a fairly rare pathology, so there is no reliable data on the structure of morbidity and the distribution of etiological factors. The literature, as a rule, presents isolated clinical cases [4-7].
Occasional reviews on this topic include only a few dozen published observations: for example, F. Raherinantenaina et al., having analyzed data on pseudoaneurysms of the limb arteries from 1965 to 2015, provide information on 69 cases related to the upper limb arteries published in the English-language literature [8]. As a rule, the etiological factor of the development of false aneurysm is a trauma (civilian, criminal or sports-related) [9-12]. Currently, the importance of iatrogenic aneurysms is also growing, which is explained by the increased number of endovascular interventions [13, 14]. Literary data and the authors’ own experience show that the main reason for the development of brachial artery pseudoaneurysms is undiagnosed vascular trauma due to therapeutic and diagnostic errors. Despite the emergence of modern methods of minimally invasive treatment of aneurysms, open surgery remains the gold standard to date [15, 16]. Anastomotic fistula aneurysms are quite widely represented in the literature and are a typical complication after the formation of a permanent vascular access for dialysis [17-20]. The literature contains descriptions of clinical cases of thromboembolic complications, in particular palmar arch thrombosis with brachial artery pseudoaneurysm [21]. The patient underwent systemic thrombolysis with the drug Actelise, thoracic sympathectomy to open the peripheral blood flow, and then prosthetic repair of the brachial artery with an autogenous vein graft taken from the lower limb.
Thus, the presence of a pseudoaneurysm is an absolute indication for surgery, but questions remain regarding the methods of surgical treatment.
Patient A, born in 1988, was admitted to the clinic with complaints of a pulsating mass in the right shoulder, periodic pain in the right arm aggravated by exertion.
Upon admission, the patient was in satisfactory condition and felt well. Body temperature 36.3 C. Skin of normal color and moisture. No swelling of the lower limbs. Lymph nodes accessible to palpation not enlarged. Breathing in the lungs in all parts, no wheezing. RR 16 b/min. Heart sounds muffled and rhythmic. Hemodynamics stable. The abdomen not swollen, symmetrical, soft, participating in respiratory movements. Peristalsis was audible. Shchetkin-Blumberg's symptom negative. Liver along the edge of the costal arch. Normal stool. The lumbar region not changed. The kidneys not palpable, their palpation painless. The “tapping” symptom negative on both sides. The bladder not identified by palpation or percussion. Diuresis sufficient. Urine without visible pathological impurities. Locally – clinical picture of post-traumatic aneurysm of the right brachial artery.
The patient was a military man who received a shrapnel wound to his arm during combat operations in December 2023. Over time, the above complaints appeared, which forced him to consult a surgeon. Hospitalized for surgical treatment.
Operation: Aneurysmectomy, endarterectomy, autovenous prosthetic repair of the right brachial artery.
The brachial artery aneurysm, and the afferent and efferent portions of the brachial artery were accessed through a 7 cm incision along the inner surface of the right shoulder in the middle third using endotracheal anesthesia. Fig. 1.

Figure 1. Access to the pseudoaneurysm is provided.
The segment for prosthetics was determined. A section of the great saphenous vein was taken for an autovenous prosthesis from two 3 cm incisions along the inner surface of the right thigh. The autograft was prepared for transplantation. The brachial artery was compressed. Aneurysmectomy. Fig. 2 (a, b)
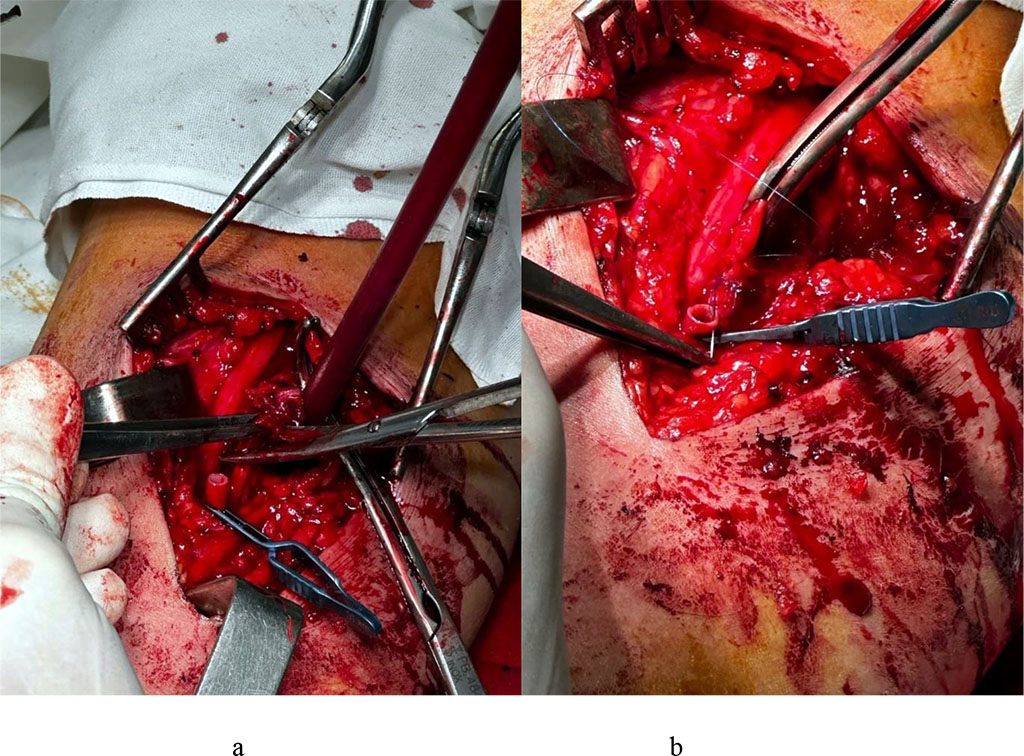
Figure 2. Aneurysmectomy (a), mobilization and endarterectomy of the brachial artery for prosthetic repair.
After careful endarterectomy of the proximal and distal portions of the brachial artery, satisfactory central and retrograde blood flow was obtained. Autovenous prosthetic repair of a section of the brachial artery was performed using a reversed great saphenous vein. Fig. 3 (a, b).
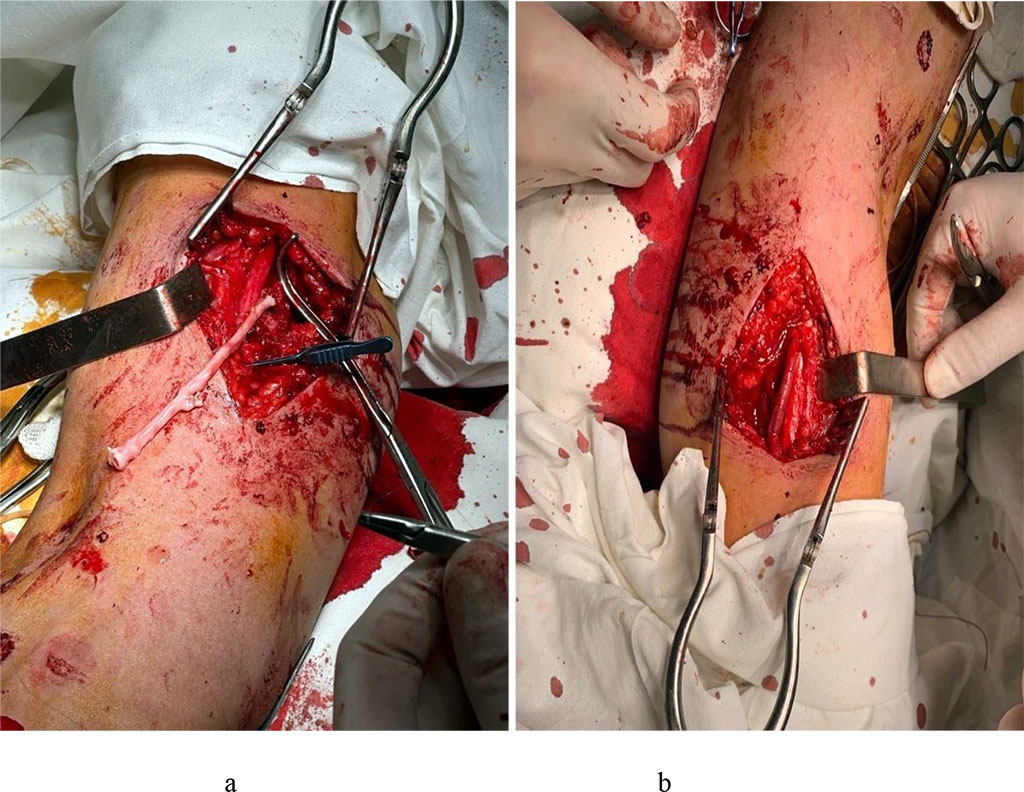
Figure 3. Autovenous prosthetic repair (a). The final appearance of the surgical site – blood flow is restored (b).
The blood flow was restored. The pulsation of the artery and prosthesis was satisfactory. Hemostasis. Drainage of the wound. Layered suture of the wound. Bandage.
The condition at discharge was satisfactory. Body temperature 36.4 C. Hemodynamics stable. The kidney area was painless on palpation. CVA tenderness negative on both sides. The abdomen was soft on palpation and painless in all parts. Diuresis was sufficient. Locally – positive dynamics, postoperative wounds were clean, the sutures were good, the pulse on the right wrist was clear, there was no evidence of complications. Recommended: Clopidogrel 75 mg 1 time per day, Eliquis 2.5 mg 2 times per day, restriction of physical activity for 1 month.
Histological study: Macroscopic description – Fragments of grayish-brown dense elastic tissue with a volume of 2 cm3 two pieces each. Microscopic description (Fig. 4) – thrombotic mass (a), fragment of the vessel wall with fibroblast proliferation (b), hemorrhages, focal hemosiderosis (c), and moderate lymphocytic infiltration (d).
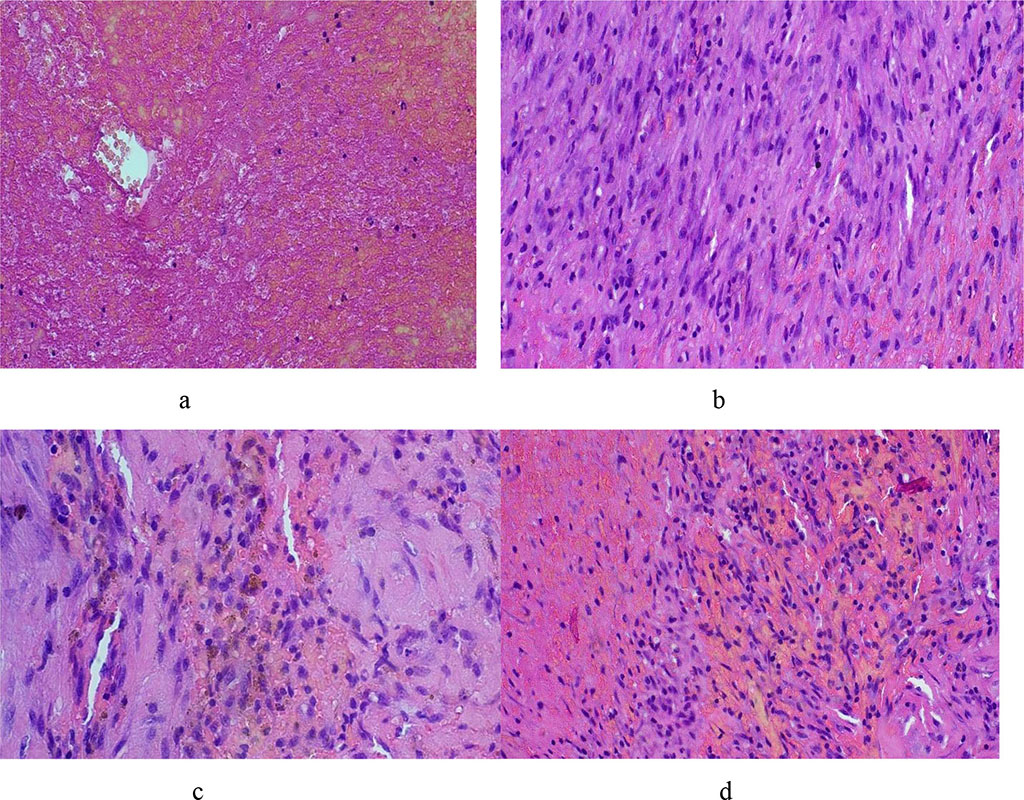
Figure 4. Morphological picture of a pseudoaneurysm – see explanations in the text (hematoxylin-eosin, X100)
Observation by a surgeon at the place of residence. Examined after 6 months. Complete restoration of the limb function.
Autovenous prosthetic repair of a section of the brachial artery with a pseudoaneurysm due to a gunshot wound is an effective surgical method of treatment and restoration of blood flow, especially since X-ray endovascular interventions are not always acceptable in this situation.