- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 3: e1. DOI 10.35630/2199-885X/2022/12/3.27
About 9500 neoplasms of the oral mucosa compromised by Covid infection are registered annually in Russia. They have high mortality rates - more than 50%. One of the risk factors for occurrence of malignant neoplasms of the oral mucosa are human papillomaviruses and Epstein-Barr virus, the mechanism of carcinogenesis of which is not fully understood and is still a subject of research. At the same time, the virus-associated pathology tends to grow, increasingly impacting younger people. With good visual accessibility of the oral mucosa, advanced cases of oncopathology (3-4 stages) are observed quite often (67%), preceded by undiagnosed virus-associated processes. The aim of this study is to optimize the early diagnosis of the mucosal virus-associated processes and to prevent malignization. We examined 375 patients of both sexes aged 18 to 65 years with various diseases of the oral mucosa. 18% of them were carriers of human papillomavirus (HPV) and Epstein-Barr. The examination algorithm included a clinical stage (instrumental examination, index assessment, autofluorescent stomatoscopy) and a laboratory stage (liquid cytology, PCR diagnostics of human papillomavirus and Epstein-Barr, and, if EBV was detected, an immunochemical blood test for capsid and nuclear antigens). The results of the study show that pathological changes in the oral mucosa and the red border of the lips associated with viral damage, which manifests itself in the form of hyperkeratosis (40 people - 59%), cheilitis (12 people - 17.6%), long-term non-healing erosive and ulcerative phenomena (9 people - 13.1%), oncopathologies (7 people - 10.3%). Thus, our diagnostic algorithm for examining patients with oral mucosal disorders reduces enables to reduce the risk of oncopathology and its neglected forms.
Keywords: virus-associated pathology, oncopathology, autofluorescence stomatoscopy, HPV, Epstein-Barr virus.
Virus associated pathology accounts for 15% of cases of all malignant neoplasms in the world. Viral infection leads to the development of orally potential disorders predisposed to malignant transformation. The problem of diagnosing the nature of the pathological process is also that viruses can be latent in the host organism for many years and become activated when favorable conditions are created for it [4].
The primary symptomatology of the virus-provoked changes in the oral mucosa, as a rule, does not have specific signs and evident complaints, and the pain syndrome appears in the later stages against the background of lesions of both the superficial and deep layers of the epithelium (erosion, ulcers). In this regard, the course of the associated pathology virus is long, not amenable to standard therapy, has a high tendency to malignancy and impairs the patient's quality of life [2,7,9,10].
Oral cancer ranks sixth among all cancers in the world. In the Russian Federation for 2020 556 thousand people were registered with the first diagnosis of malignant neoplasms, but already in 9 months in 2021, the incidence of cancer has increased up to 791 thousand. Oncological incidence of the oral cavity and the red border of the lips for 2020 reached 13.5 thousand people, of which 9.6 thousand people are men, and 3.9 thousand people are women, and ranks 18th among all cancers. In the coming years, oncologists expect a “surplus of oncology cases” that were not diagnosed during the pandemic. The number of oncological diagnoses made at late stages has significantly increased, which is associated not only with the coronavirus pandemic, but also with late patient referral and insufficient oncological alertness among dentists in primary care [3,6].
More than 100 types of HPV are known and, depending on the oncogenic potential, viruses of high (types 16, 18, 45, 56), medium (types 31, 33, 35, 51, 52, 58) and low (types 6, 11, 42, 43, 44) oncogenic risk. The two highly oncogenic HPV types (16 and 18) account for up to 95% of oral cancers [1,5].
Epstein-Barr virus can infect a variety of cell types, including B cells of the immune system (a type of white blood cell) and mucosal epithelial cells. EBV is a representative of DNA-containing viruses, it has 4 main antigens: early antigen (early antigen - EA), capsid antigen (viral capcide antigen - VCA), membrane antigen (membrane antigen - MA), nuclear antigen (Epstain-Barr Nuclea antigen - EBNA) [8].
Thus, early diagnosis of virus-associated transformations of the oral mucosa is a complex and urgent problem.
The purpose of the study: optimization of early diagnosis of virus-associated processes in the oral mucosa and preventing their malignancy.
A clinical examination of 375 patients of both sexes aged 18 to 65 years with various diseases of the oral mucosa was carried out on the basis of the Department of Dentistry of the Federal State Budgetary Educational Institution of Higher Education "PIMU" of the Ministry of Health of the Russian Federation in the period 2020-2022.
Research methods: clinical, autofluorescent stomatoscopy, liquid cytology, PCR diagnostics of human papillomaviruses and Epstein-Barr virus, immunochemical blood test for Epstein-Barr virus antigens, analytical.
In order to visualize the pathological process, all patients underwent an autofluorescence study using the AFS apparatus (Polyronic LLC, registration certificate No. FSR 2011/10669) with a wavelength of ≈ 400 nm. The principle of the method is that the light, lingering in the surface layers of the COP at a depth of 4-19 mm, is visualized through a light filter as a green glow of varying intensity, depending on its normal structure. The obtained optical images allow to determine the pathological process present on the oral mucosa. So it is known that during inflammation, “extinguishing of luminescence” occurs, foci of hyper- and parakeratosis are determined by foci of light (white) luminescence, and in dysplasia and malignant transformation, a center of loss of fluorescence is detected, defined as a “dark spot”.
In order to confirm the diagnosis, material was taken for liquid cytology. The positive aspect of this technique is its minimally invasiveness, organ preservation and the ability to carry out morphological in vivo diagnostics of the pathological process of ORS. The sensitivity of this method is 95%, while the traditional cytological analysis is only 40-60%. The cytological study was carried out at the National Center for Clinical Morphological Diagnostics LLC (St. Petersburg).
PCR diagnosis of human papillomaviruses and Epstein-Barr virus was carried out at Nizhny Novgorod Regional Center for the Prevention and Control of AIDS (Nizhny Novgorod, Russia), and an immunochemical blood test for Epstein-Barr virus antigens was also carried out there with a positive PCR test. When diagnosing HPV, types of the virus of high and medium oncogenic risk were determined (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59), Jg M was determined for the Epstein-Barr virus (to the capsid antigen) and Jg G (to nuclear antigen).
After the examination, 68 people (14.9% of the total number of those examined) were identified as carriers of the viral infection. A specific feature of the clinical course of pathological processes of the oral mucosa associated with viral pathology is a long-term process (from 6 to 12 months), which is not amenable to standard therapy.
Pathological processes on the oral mucosa and the red border of the lips associated with viral lesions have different manifestations: hyperkeratosis (40 people - 59%), cheilitis (12 people - 17.6%), long-term non-healing erosive and ulcerative phenomena (9 people - 13.1%), oncopathology (7 people - 10.3%).
As a result of PCR diagnostics, human papillomavirus was detected in 21 people, DNA types 45 and 16 were determined. Analysis of the Epstein-Barr virus gave a positive result in 50 patients, the nuclear antigen (Jg G) was determined, which indicates a long stay of the virus in the host organism. Of all identified cases, 3 people had both human papillomavirus and Epstein-Barr virus.
The optical image of papillomatosis of the lateral surface of the tongue is characterized by a light green type of luminescence, with areas of white luminescence. Liquid cytology: reactive changes in the superficial and intermediate layers of the squamous epithelium, parakeratosis of squamous cells, hyperkeratosis, data for squamous intraepithelial lesions were not found. PCR diagnostics: HPV HCR genotyping and quantitative determination of DNA type 45 - 4.4 Ig (copies/10^5cl), type 16 - 6.3 Ig (copies/10^5cl) (Fig. 1a,b).
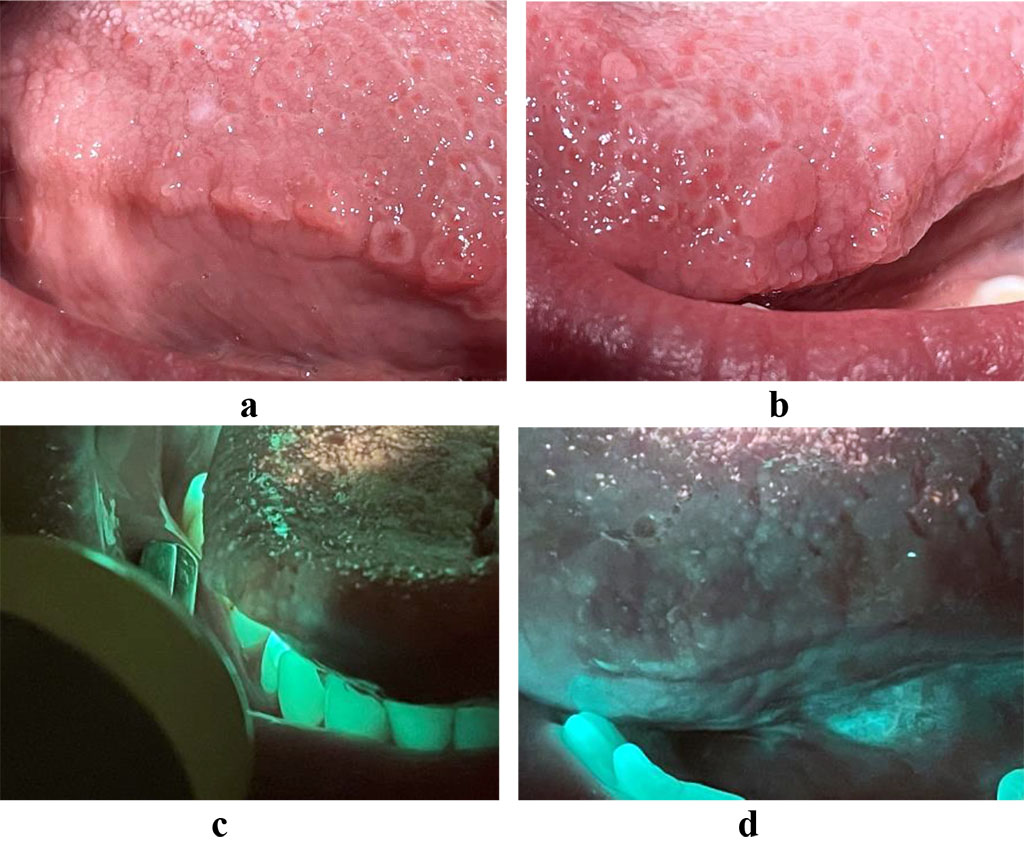
Fig.
1. a, b - papillomatosis of the lateral surface of the tongue
c, d –
optical image of papillomatosis of the lateral surface of the tongue.
The optical image obtained from a patient with hyperkeratosis of the red border of the lips is characterized by a change in color to light green. Liquid cytology showed: squamous epithelium of the superficial and intermediate layers without atypia. Parakeratosis of squamous epithelial cells. The study identified antibodies to the Epstein-Barr virus VCA Jg G (11,810 CP) (pic. 2a,b).
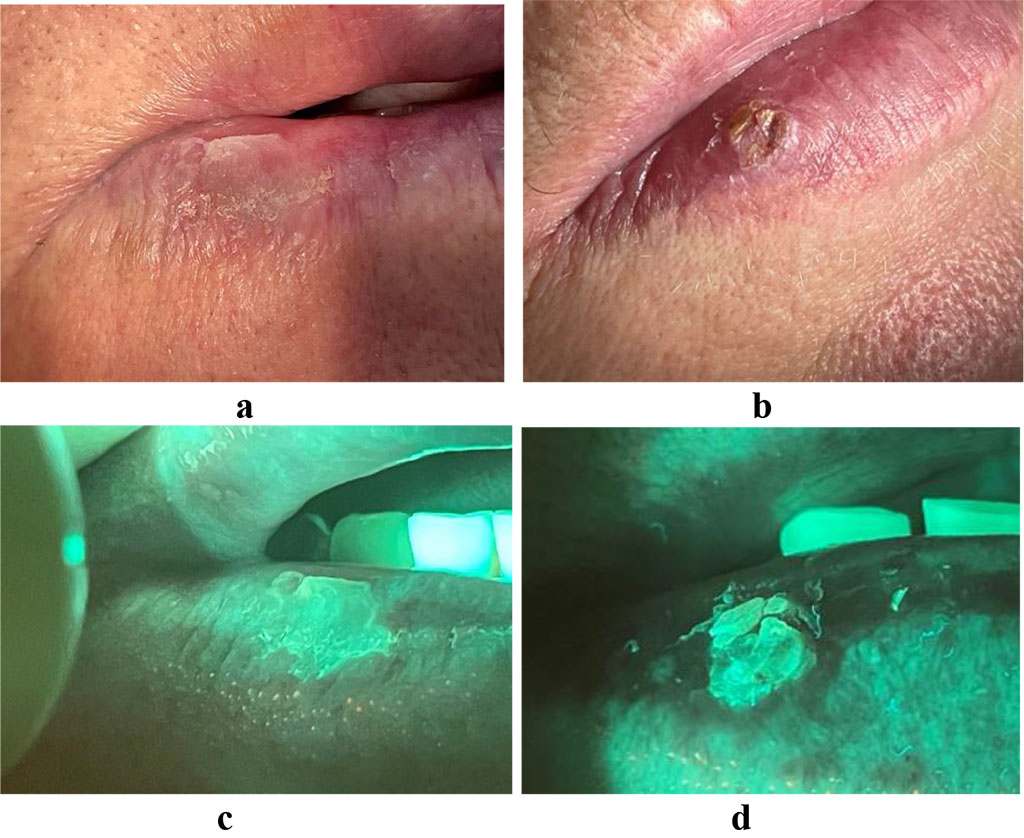
Fig.
2. a, c - hyperkeratosis of the red border of the lower lip
b,
e – optical image of hyperkeratosis of the red border of the lower
lip
In case of a tumor, the optical image is visualized by the loss of luminescence - a “dark spot”. The area of tumor decay with abundant microbial invasion is accompanied by the appearance of a glow in the red spectrum. PCR diagnostics revealed the presence of human papillomavirus strain 18. A biopsy was performed at the NOKOD, confirming squamous cell carcinoma of the oral mucosa. (pic. 3 a, b)
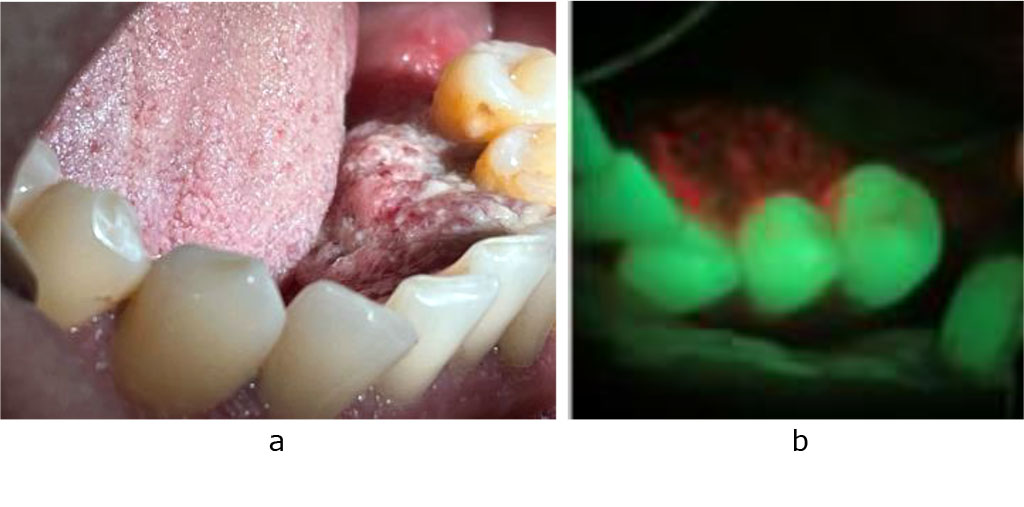
Fig.
3.
a - squamous cell carcinoma of the floor of the mouth
b -
optical image of squamous cell carcinoma of the floor of the mouth
Thus, our study indicates that in the setting of high prevalence of oral mucosa disorders, their viral accompaniment is quite often detected, diagnosed in the laboratory though not clinically confirmed. Since the presence of a viral infection is a risk factor for the pathological process and malignancy, early verification of oncogenic viruses is not only relevant, but also promising. The use of an integrated approach in diagnosis, including a number of step-by-step screening tests: autofluorescence stomatoscopy, PCR diagnosis, liquid cytology and immunochemical blood analysis in patients with pathology of the oral mucosa contributes to the early detection of oncopathology, whereas justifying the use of antiviral drugs in the algorithm of pathogenetic treatment.