- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 3: e1. DOI 10.35630/2199-885X/2022/12/3.25
The results of clinical, photometric, morphometric, radiological and functional studies were employed to develop an advanced methodology for treating patients with dentoalveolar transversal divergent occlusion. The dentoalveolar type of transversal divergent occlusion has been identified as being both an independent nosological issue and can be combined with other issues and deformations affecting dentoalveolar arches. The developed concept for comprehensive rehabilitation of patients with dentoalveolar transversal divergent occlusion complicated by dentition issues has a following algorithm: counseling, diagnosis, splint treatment using a distracting splint, previously completed orthodontic treatment, splint treatment using a stabilizing splint, final orthodontic treatment, aesthetic and functional prosthetics.
Comprehensive rehabilitation offered to patients with dentoalveolar transversal divergent occlusion is aimed at improving the jaw bones position and the occlusion. Thus, it creates multiple fissure-tubercle dentition contacts; stabilizes the lower jaw position; improves position of intra-articular structures. The comprehensive rehabilitation enable eliminating functional disorders, muscle excessive tension and pain symptom. In general, the face profile as well as the occlusal plane horizontal position is improved.
Keywords: abnormal occlusion, transversal divergent occlusion, cone beam computed tomography, magnetic resonance imaging, temporomandibular joint, electromyography, computed gnathography.
According to World Health Organization reports (2005), dentoalveolar issues are rated as one of the most common dental disorders in humans, with the need for orthodontic treatment in wealthy EU countries going beyond 38%. The same indicator in the US and Canada is 35%, Russia accounts for 47% [39,44]. Abnormal occlusion is a growth and development pathology, which affects the dental system and is caused by local, regional and functional etiological factors, as well as by genetic and exogenous causes playing a role through the prenatal, natal and postnatal periods [2,10,19,48].
In most cases, occlusive disorders result from the interaction of several factors, and there is no way to identify any specific etiology [7,9,22,33,47]. Occlusion issues come along with a deformed occlusal plane, altered movements of the lower jaw, disturbed (improper) functioning of the masticatory muscles and of the temporomandibular joints [1,5,13,23,43].
Clinical types of dental issues (dentoalveolar, gnathic, combined) have different etiology and pathogenesis, as well as they differ in terms of morphological, functional and aesthetic features [38,50]. Dentoalveolar types of occlusion issues are due to a mismatch between the size of the upper and lower temporary molar crowns, incomplete eruption of the lower first permanent molars, disproportion in the size of the dental arch segments, deformation affecting the dentition in different directions, dentition deviated shape and size, while combined with the apical base size issues [3,37,49].
Dental arches featuring pathological shape and size occur through different periods of ontogenesis, both in case of congenital and acquired maxillofacial pathology [15,16,41]. When analyzing the size and the shape of dental arches, the methods employed typically include biometric study of jaw cast models, head and face morphometric evaluation, and X-ray [6,25-31,56].
During that, dentoalveolar anomalies of occlusal relationships account for the most common issues faced by clinical orthodontics, while there have been numerous treatment methods proposed to help patients of different ages, such methods aimed at changing the shape and size of dental arches, along with creating proper antagonist contacts. However, there have also been certain specific issues identified related to periodontal tissues in case of anomalies and deformations, and their change through the course of treatment [32,35,40,55]. Experts believe, however, that there are many factors that have an effect on the shape and size of dental arches, including the craniofacial specifics, sex and race [12,20,34,52].
One of the pathological occlusion varieties is the occlusal plane divergence, which is typically due to the rotation of the jaws. There have been advanced methods presented that can be employed to analyze the occlusal plane, as well as the location of teeth has been shown in relation to the said plane, both in case of physiological and pathological occlusion, relying on data obtained through an X-ray examination [11,36].
Most of the works, both by national and foreign experts focus on analyzing the rotation of the jaws in the sagittal direction, and contain data related to typical changes in the teleroentgenogram parameters in the lateral projection with changes in angles reflecting the position of the jaws in the craniofacial structure [4,21,24]. As for the occlusal plane, it is defined as a straight line connecting the inter-incisal point with the most distal occlusal point of the molars [8,14,45].
Experts also note, though, that building such a sagittal occlusal line reflects the true position of the occlusal plane, mainly with different types of physiological occlusion. In pathological occlusal relationships, which are due to abnormal or deformed dental arches, both the anterior and the posterior points of teleroentgenograms are displaced [46,53].
Given that, there have been methods proposed for identifying the occlusal plane location in the sagittal direction, while relying on relatively stable anatomical landmarks that reveal no dependence on the deformation of the dental arches anterior and lateral segments [17,18]. Changes in the location azimuth of the pathological occlusal plane regarding other horizontals in the transversal direction can be seen in works by researchers focusing on various types of cross occlusion (gnathic, articular and dentoalveolar) [54]. There are also specific features of the mandibular joint pointed out, which occur in case of various occlusal relationships and at different sizes of the face gnathic part [42,51].
The available literature offered us no information concerning the specific features of the occlusal plane location in patients with the dentoalveolar transversal divergent occlusion, in case of which relatively correct occlusal antagonist relationship is to be observed. However, there is an occlusal plane divergence in the transversal direction to be noted, which serves a good explanation to the purpose of this study.
Aim of study: to develop a concept and an algorithm for the stages of diagnosis and orthodontic treatment to be offered in patients with dentoalveolar transversal divergent occlusion.
A pilot stratified study has been held, which implies the examination of the temporomandibular joint (TMJ) digital photographic images, cone-beam computed tomograms (CBCT) and magnetic resonance tomograms (MRI). 6 patients aged 18-25 underwent electromyograms of masticatory muscles and computer gnathograms in order to obtain preliminary data concerning the specifics of diagnosis and the choice of methods for the treatment of transversal divergent occlusion. Following the requirements of the Ethical principles for medical research involving human subjects (World Medical Association Declaration of Helsinki, 1964), voluntary informed consent was obtained from each participant prior to the research.
The photometric protocol was performed with the natural head position (NHP) relying on the method by Moorrees and Kean (1950) and D.M. Sarver (2000). Images with the mouth slightly open with the lips at rest were made to assess the upper incisors exposure, which is a starting point for orthodontic treatment planning. Full-face photographs with a natural smile allowed visualizing the patient’s natural smile aesthetics. There was also evaluation made as to the match between the upper and lower jaw cosmetic center and the face midline, the smile width and the length of the cheek corridors, the exposure of the incisors and gums through smiling, the gingival edge symmetry and the rise of the upper lip red border. Full-face occlusal photographs of dentition, right and left, in the conventional position of the lower jaw were taken to observe visual changes affecting the occlusal correlations at the orthodontic correction stages the patient goes through.
When analyzing the occlusal plane azimuth, a spatula was used to be applied to the antimeres at the canines and premolars area, as well as the angle of divergence to the ocular (eye-pupil) horizontal was identified, both visually and through a photostatic examination. In the images, a median vertical (the aesthetic center line) was drawn in a direct projection, which ran through the n (nasion) point perpendicular to the eye-pupil horizontal, the latter considered a relatively stable reference point for the face area. The aesthetic vertical and the occlusal plane intersection point was taken as the divergence point.
The occlusal plane horizontal was designed from the forecasted occlusal point in the middle of the distance from the subnasal sn (subnasale) point to the supramental sm (supramentale) one. A horizontal line, running perpendicular to the aesthetic center line, was drawn from the designed occlusal point (typically coinciding with the inter-incisal point). And then this was used as a mark for detecting front teeth deviation, which might be observed as located either above and/or below the line in question. The obtained lines allowed identifying the pathological occlusal plane divergence angle in the transversal direction, as well as they served as a criterion for evaluating how effective the offered treatment was.
Through the stage of diagnostics and treatment plan development, all the patients went through cone-beam computed tomography head examination in the conventional occlusion, performed using a Planmeca ProMax ® 3D Mid (Planmeca) device. The CBCT helped identify the position and the condition of the teeth, along with the occlusal plane deformation, the bone tissue level, and asymmetry of the jaws, the shape of their heads, as well as the length and the shape of the lower jaw branches (Fig.1).
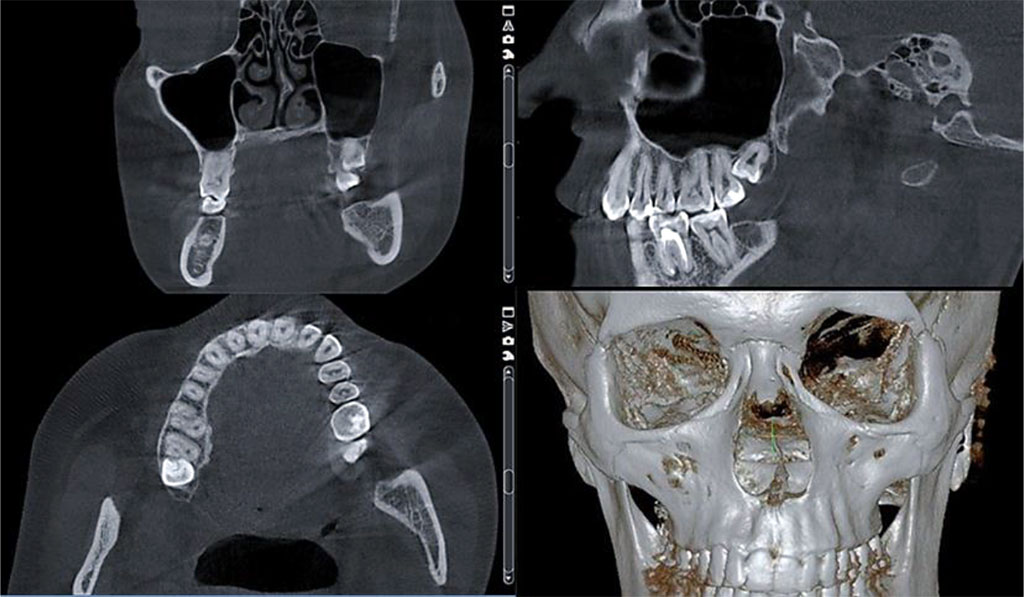
Fig. 1. Dentition CBCT, case of dentoalveolar transversal divergent occlusion
To ensure a reliable analysis of the left and right TMJ bone structures in the conventional occlusion, an assessment was carried out in the oblique coronary and in the oblique sagittal projections, aimed at studying the following: the mandibular heads position and symmetry; the articular cavity shape; the articular cavity width and depth values; the articular tubercle prominence; the mandibular heads shape; the X-ray joint gap in all parts; the height of the mandibular heads location in relation to the articular surface; the cortical plate integrity (Fig.2).
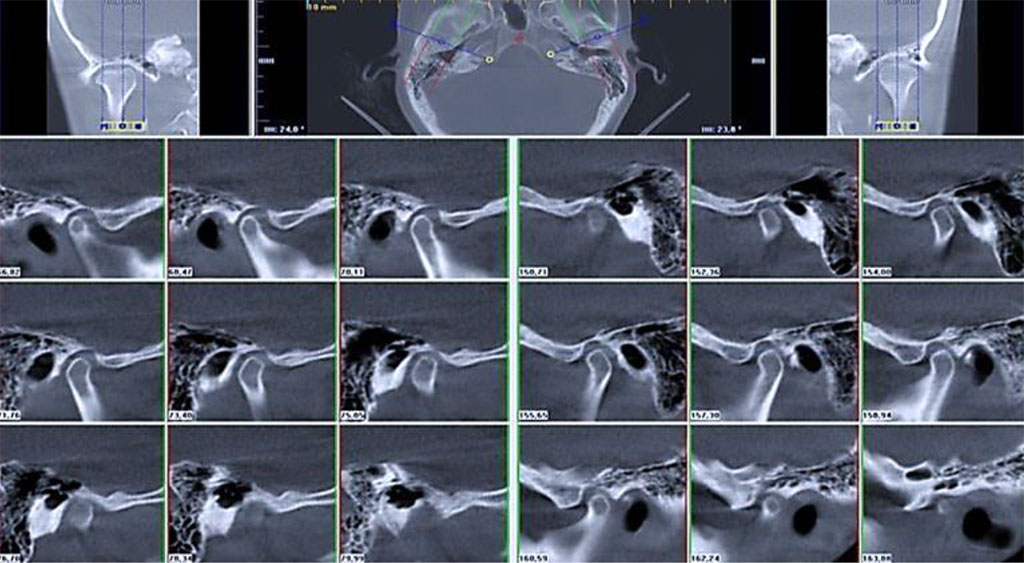
Fig. 2. Layered TMJ CBCT, 0.5 mm increment
In order to assess the severity of the TMJ intraarticular pathology, magnetic resonance imaging (MRI) was performed relying on the Ya.L. Manakova method (2010). The MRI was done using an open-type APERTO ("Hitachi") tomographic machine with a magnetic field value of 0.4 Tl. The obtained images were in the oblique sagittal and oblique coronary projections, the slice being 3 mm thick. Besides, both planes of the MRIs were used to evaluate the shape, the size, the structure of the spongy substance and the mandibular head cortical layer thickness, the position of the mandibular head in the temporal bone mandibular fossa, as well as the status featured by the lateral pterygoid muscles. The severity of the identified disorders was classified subject to the Wilkes International Classification (1989), in view of the modified Helkimo clinical index (Fig.3).
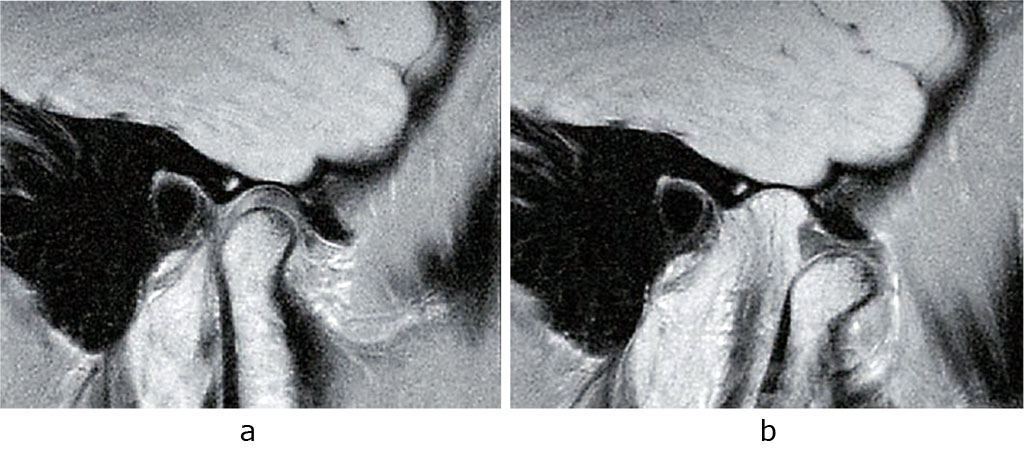
Fig. 3. TMJ MRI in the oblique sagittal projection; mouth closed (a) and open (b).
The study implied performing electromyography and computer gnathography (kinesiography) using the Myotronics K7 diagnostic machine (USA). To assess the masticatory muscle biopotentials and identify their physiological state at rest (Fig.4a) as well as at maximum compression (Fig.4b), surface electromyography of temporal muscles (right – RTA; left – LTA), true masticatory muscles (right – RMM; left – LMM), sternocleidomastoid muscles (right – RTR; left – LTR), biconvex muscles (right – RDA; left – LDA) was done. Kinesiography included assessing the amplitude and designing a three-dimensional graphical representation of the lower jaw conventional movement trajectory, as well as investigating the trajectory nature in terms of opening and closing the mouth (Fig.4 c, d).
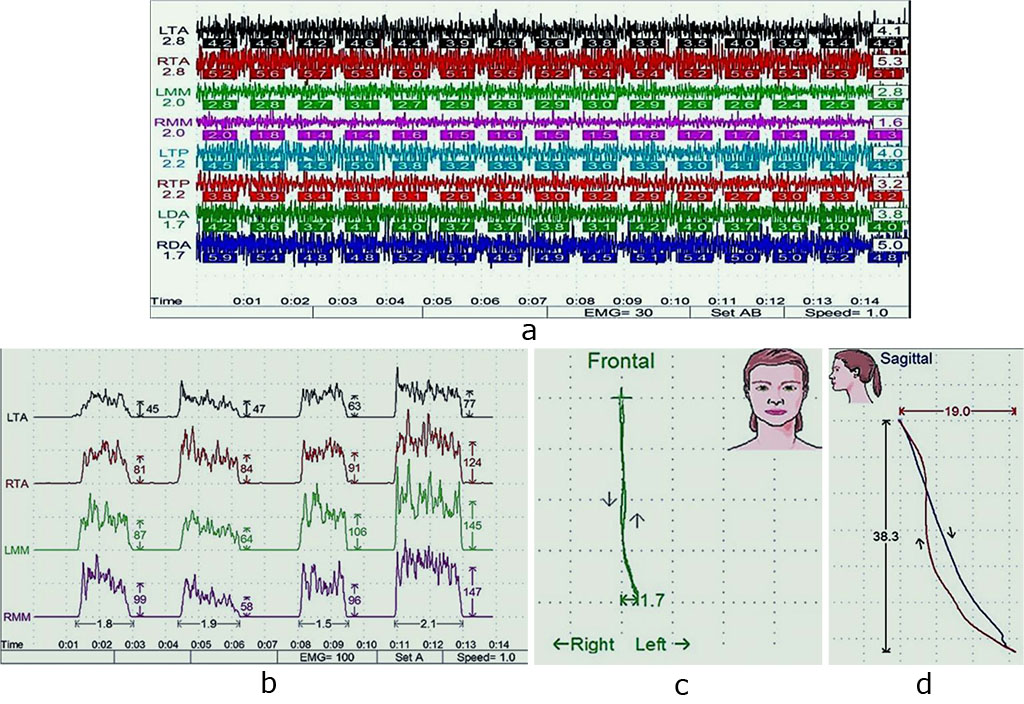
Fig. 4. Masticatory muscles electromyogram, physiological rest (a) and maximum compression (b); lower jaw movement kinesiogram, transversal (c) and sagittal (d) planes.
During electromyography, the lead bipolar electrodes were placed on the skin surface in the motor points projection so that the muscle fibers could match the electrodes longitudinal axes. During kinesiography, there was a magnetic sensor installed at the lower jaw incisors, and the sensor then transmitted data concerning the lower jaw movements (mouth opening and closing; side movements) to a sensor frame, which was attached to the patient’s head. In order to evaluate the outcomes, functional studies were held 6 months following splint and orthodontic treatment.
Patients with dentoalveolar transversal divergent occlusion typically feature a proper closure of antagonists with the lower teeth overlapped by the upper ones. At the same time, pathological occlusal plane is deviated 4 to 10 degrees from the occlusal horizon.
In the course of the orthodontic treatment, all the patients showed improved occlusal relationship, stabilized lower jaw position, improved position of the TMJ inner structures, reduced intensity of functional disorders and lower tension in the masticatory muscles, improved aesthetic profile of the face, and a better position of the transversal occlusal plane.
The clinical example offered here shows an analysis of the diagnostics and treatment effectiveness observed in patient V., 23 y.o., who complained of aesthetic issues, improper teeth closure, troubles experienced when opening the mouth, pains and clicks in both TMJs when opening the mouth, the masticatory muscles rapid fatigue and soreness even at rest, which would intensify while chewing solid food. Setting a final diagnosis required a comprehensive diagnostic examination, namely, lateral-projection orthopantomogram (OPTG) and teleroentgenogram (TRG) examination; TMJ CT and MRI; examination of jaw cast models plastered into an articulator; examination of face photos taken in various projections; functional examination.
A thorough comprehensive examination and photostatic analysis revealed that the divergence angle shaped by the pathologically located transversal occlusal plane deviating from the aesthetic horizon was 6 degrees. There was deep incisive occlusion to be observed. The occlusal plane divergence point was located at the vertical aesthetic center line and coincided with the inter-incisal line (Fig. 5).
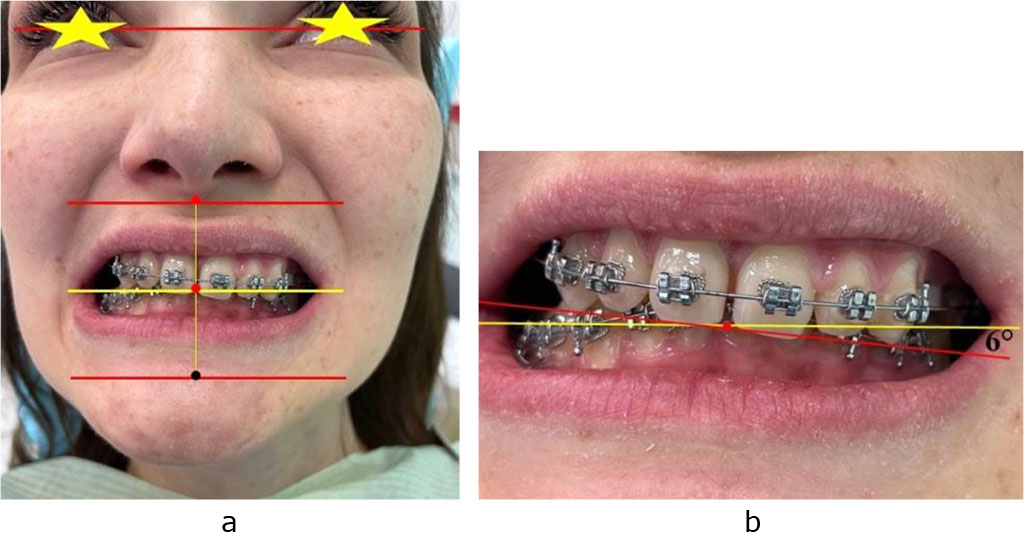
Figure 5. Occlusal relationships (a) and the occlusal plane divergence angle (b) in patient V., 23 y.o., featuring dentoalveolar transversal divergent occlusion
The TMJ computed tomography showed normal anatomy of the condylar process; displaced lower jaw articular heads (down and forward) at closed dentition in the conventional position of the lower jaw (Fig.6).
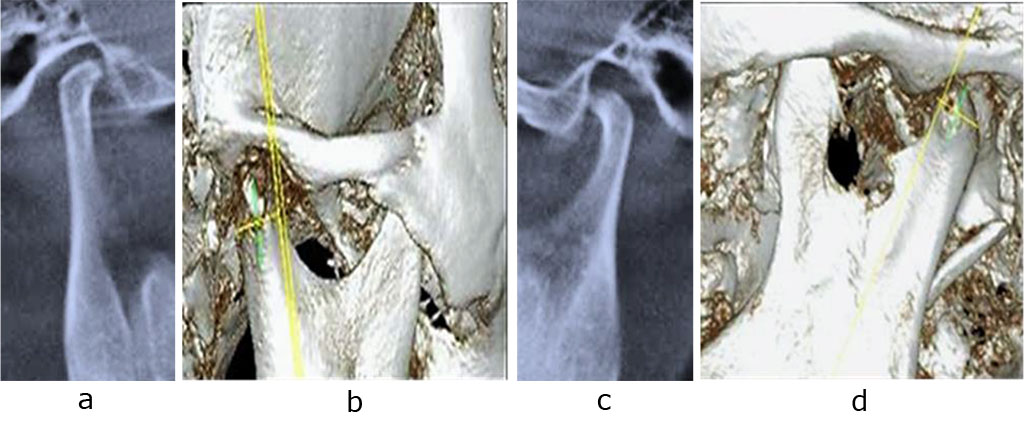
Fig. 6. Patient V., CBCT, right (a, b) and left (c, d) TMJ, mouth closed; prior to orthodontic treatment
A bilateral examination of the TMJ MRI in the oblique sagittal projection (mouth closed) revealed a partial ventral displacement of the right TMJ degeneratively altered disc with reposition, as well as a complete displacement of the left TMJ degeneratively altered disc with no reduction. Following the Wilkes International classification (1989), the TMJ issue on the right belonged to Stage 2 (minor alteration), on the left – to Stage 3 (moderate alteration) (Fig.7).
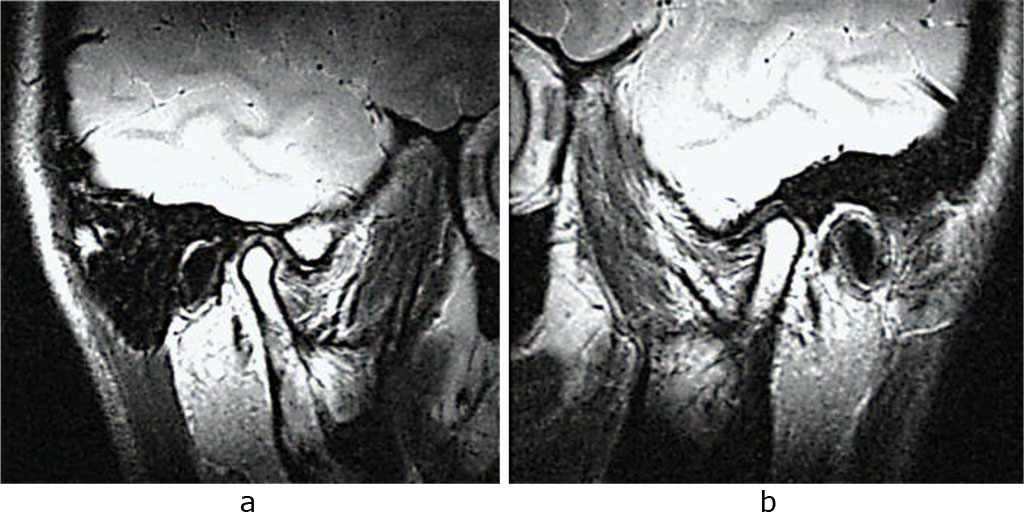
Fig. 7. Patient V., MRI, right (a) and left (b) TMJ, oblique sagittal projection; prior to orthodontic treatment
Electromyography data showed that closed teeth were associated with an increased tension in the masticatory area (Fig. 8a). The lower jaw movement kinesiography revealed the following: the lower jaw deviation in the transversal plane (lower jaw displacement at mouth opening, 2.3 mm to the right and 3.8 mm to the left); mismatch in the lower jaw sagittal plane movement trajectories at mouth opening and closing; signs of asymmetric tone in the temporal and masticatory muscles; clicks through the middle stage of mouth opening (Fig. 8b, c).
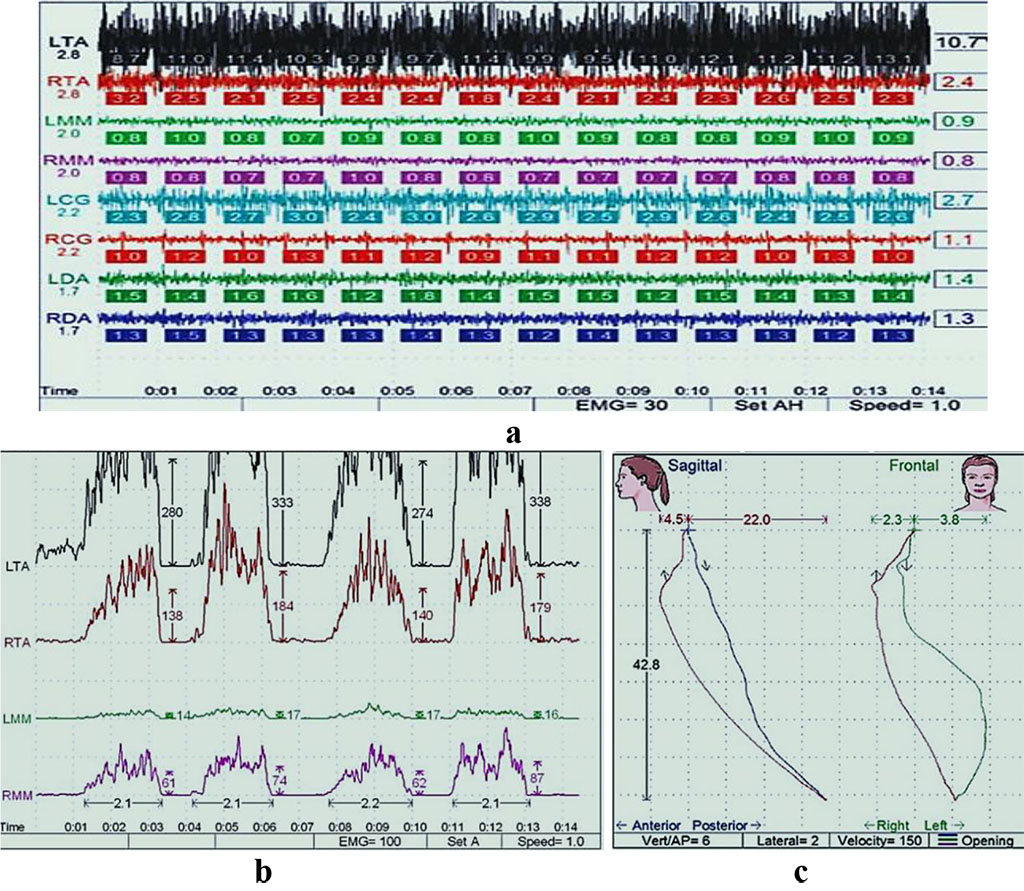
Fig. 8. Patient V., electromyogram of the masticatory muscles at physiological rest (a) and at maximum compression (b), kinesiograms of the lower jaw movements in the transversal and sagittal (c) planes
Subject to the objectives and the plan for the orthodontic treatment offered to patient V. suffering from transversal divergent occlusion, the first stage of the treatment implied designing a digital model of a therapeutic and diagnostic distracting splint positioner with a bite pad, all this in order to prevent the lower jaw displacement, to recover coordinated muscle contraction, to reduce masticatory tension, and improve the incisor overlap. The wearing mode was 6 months, 22 hrs per day, taking the appliance off when having meals or oral cavity cleaning procedures (Fig. 9).
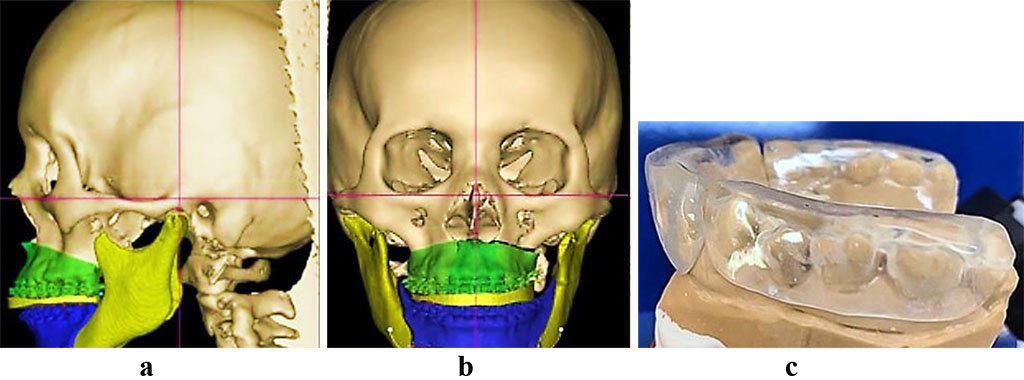
Fig. 9. Patient V., CBCT digital model and 3D rendering, profile (a) and full face (b) with a distracting splint. Distracting splint positioner on lower jaw cast model (c).
The 6 months of the splint treatment therapy offered the following results: a match achieved between the central ratio and the central occlusion; a stabilized lower jaw position (Fig. 10); improved inner structures and pathological processes, both in the right and left TMJ (Fig. 11).
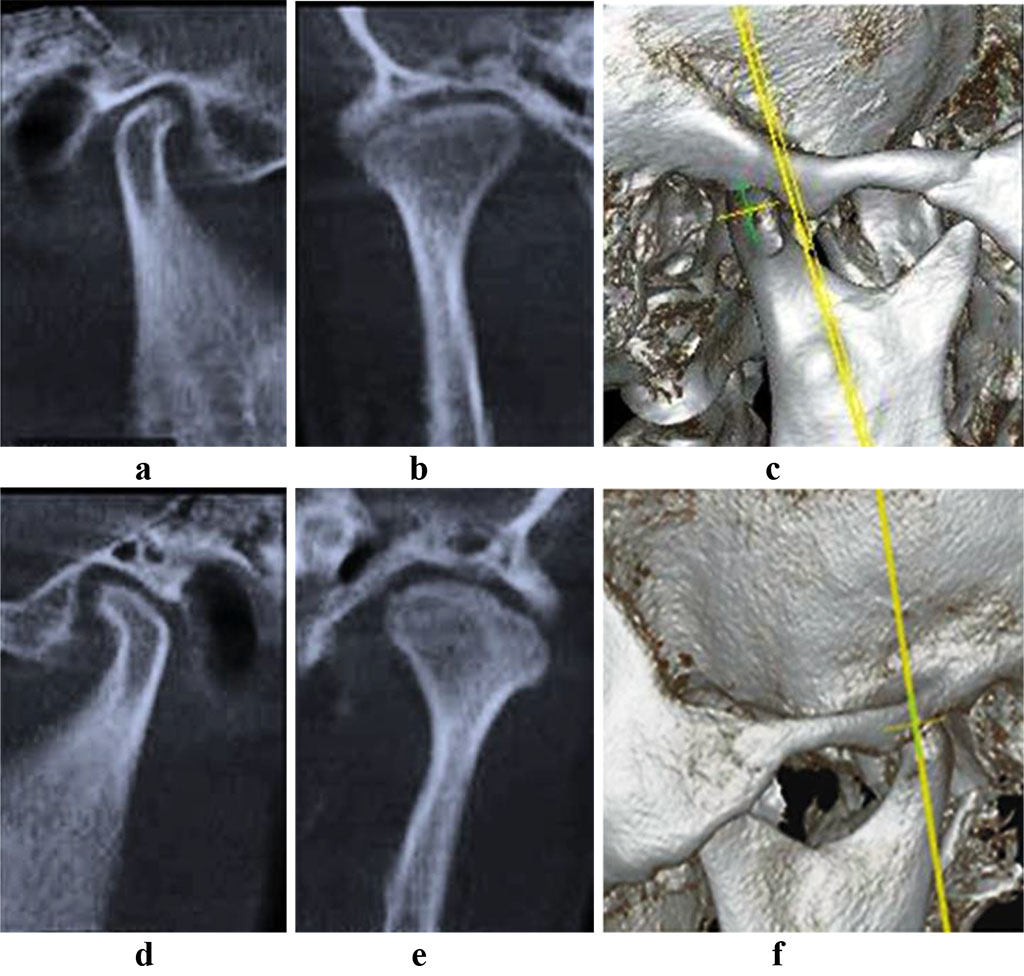
Fig. 10. Patient V., CBCT, right (a-c) and left (d-f) TMJ, mouth closed; following splint treatment
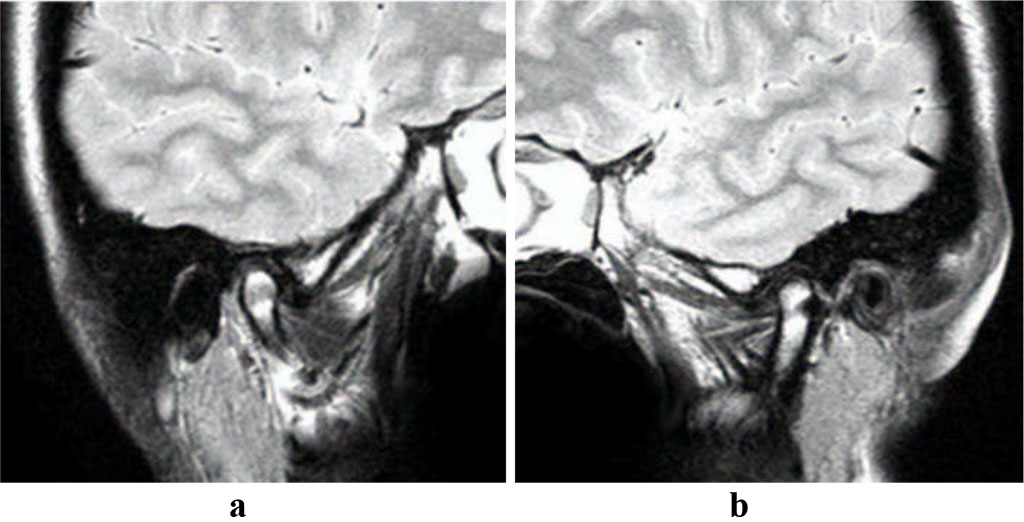
Fig. 11. Patient V., MRI, right (a) and left (b) TMJ, oblique sagittal projection; following splint treatment
Electromyography results showed that after the 6 months of the splint treatment therapy, there was a significant decrease in the muscles bioelectric activity observed at closing teeth, which was indicative of a recovered position of the lower jaw, improved occlusion, recovered neuromuscular balance, improved muscle tension, aligned asymmetry of muscle contraction, as well as an improved position of the lower jaw heads in the articular depressions (Fig. 12a). Kinesiography revealed an improved trajectory of the lower jaw movement in the transversal plane (a 3.3 mm deviation of the lower jaw position at opening the mouth) and in the sagittal plane. Once the functional disorders were removed through a distracting splint positioner, patient V. reported the absence of pain and excessive tension in the masticatory muscles; a lower intensity in the TMJ clicks; a lower level of fatigue in the masticatory muscles under stress; comfort feeling when closing of teeth; an improved TMJ function, and a significant decrease in the level of abnormal sounds in the TMJ.
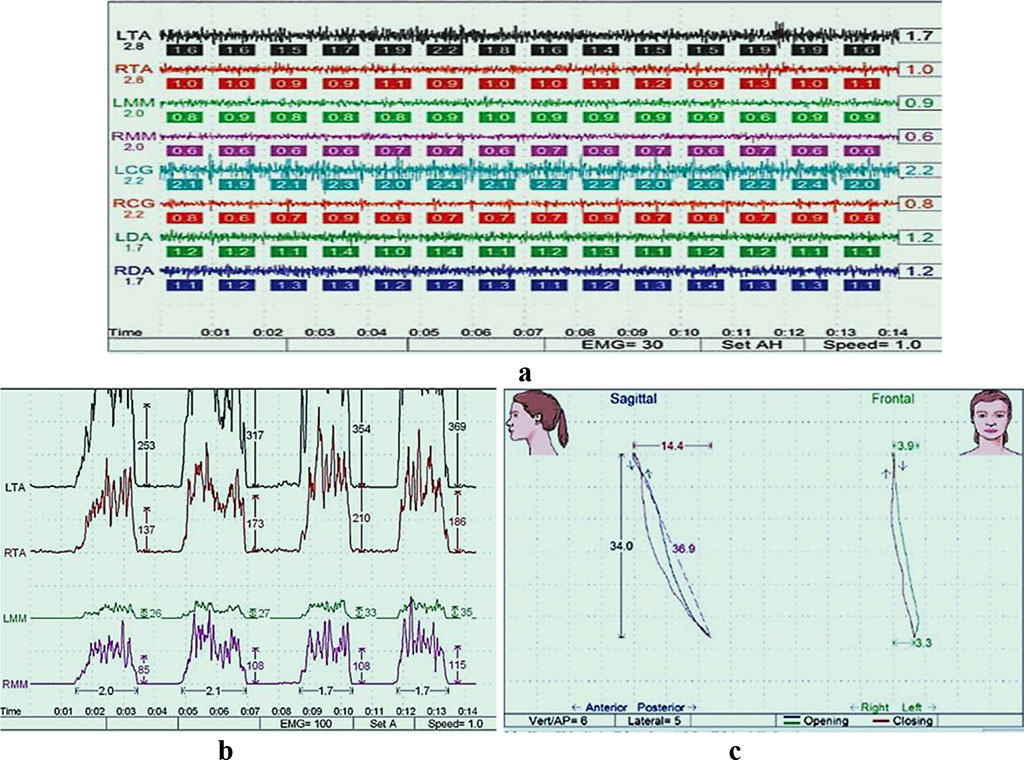
Fig. 12. Patient V., masticatory muscles electromyogram, at physiological rest (a) and through maximum compression (b), kinesiograms of the lower jaw movement, transversal and sagittal (c) planes, following splint treatment
The second stage of the orthodontic treatment offered to patients with transversal divergent occlusion involved the correction of the dentition shape and of certain teeth position, which was done through fixing the braces on the upper and lower jaw with elastic rods installed on the left in order to move the teeth vertically (Fig. 13).
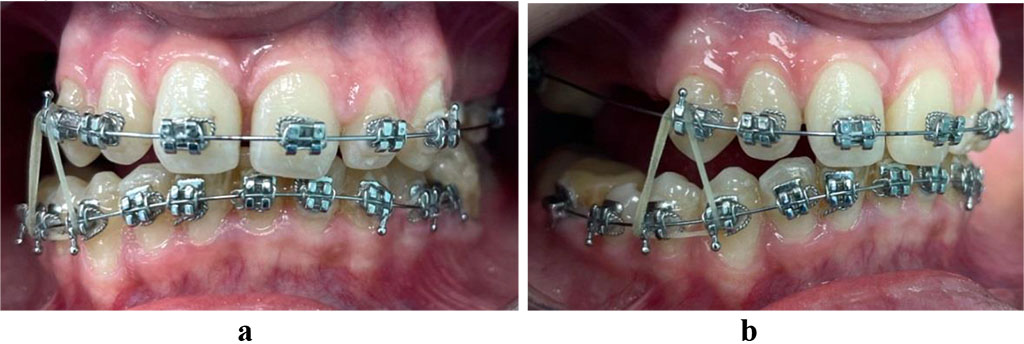
Fig. 13. Patient V., intermaxillary elastics applied on the right (a, b) when treating dentoalveolar transversal divergent occlusion
2 months following the load application, there was some improvement observed involving the occlusal plane location in the transversal direction, which stood almost parallel to the eye-pupil horizontal, as well as corrected dentition shape and improved position of certain individual teeth, which pointed at the effectiveness of the diagnostic measures and the treatment employed (Fig. 14).
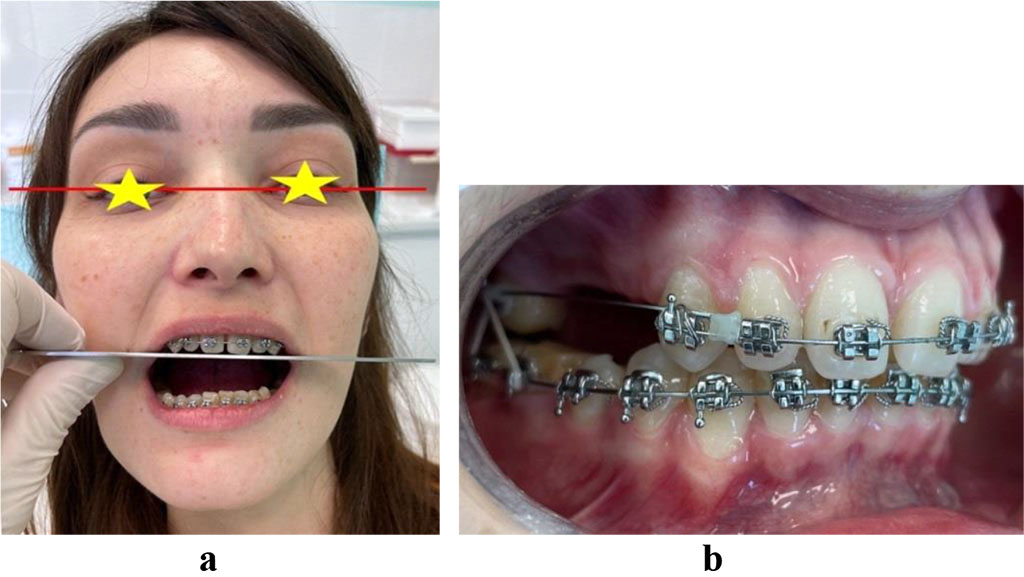
Fig. 14. Patient V., occlusal plane changed azimuth, face photo (a) and oral cavity (b) through the treatment of dentoalveolar transversal divergent occlusion
The third stage of the orthodontic treatment carried in patients with transversal divergent occlusion included splint based treatment using an occlusal stabilizing splint thus aiming to maintain the central ratio that had been achieved, as well as to maintain the chewing function and relieve the TMJ of occlusal load (Fig. 15).

Fig. 15. Lower jaw occlusal stabilizing splint
The above shows that when dealing with transversal divergent occlusion, it is advisable control the occlusal plane inclination azimuth up until it comes to be parallel to the main – relatively stable – anatomical reference points, namely the orbital or eye-pupil horizontal.