- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 3: e1. DOI 10.35630/2199-885X/2022/12/3.20
Aim: Our study aims to investigate the variability patterns involving the size and the shape of the thoracic intervertebral foramina. Materials: The study was carried out on 120 CT scans of thoracic spine of adult males (aged 21-40) without any degenerative dystrophic change. Results: In the lateral projection, the counter-lateral dimensions (vertical and horizontal diameters) and the shape of the intervertebral foramina were detected. Following values were calculated: amplitude (Min-Max), arithmetic mean (M), mean error (m), standard deviation (SD).The nature of changes affecting the size of the intervertebral foramina was also identified with increase in the cervical-lumbar direction, as well as four types of intervertebral foramina – oval, rounded, four-sided, three-sided. The extensiveness of the various shapes differs and varies depending on the foramen’s topographic location.
Keywords: thoracic spine, intervertebral foramen.
The thoracic spine has certain features that make it different from other regions. First, it is relatively stable in contrast to the mobile cervical and lumbar sections; second – this is the longest section; third – the spinal canal has minimal dimensions at this level, and four – the thoracic spine is part of the chest, which, if taken in combination with the sternum and ribs, will add to its strength; this, on the one hand, will take a significant traumatic agent to inflict damage, whereas on the other hand, a significant agent will lead to complex and combined injuries [2, 8, 9].
Treating such patients is a complex and relevant issue faced by traumatology and orthopedics, and often requires high-tech assistance, advanced equipment, and highly qualified staff [4, 12, 14]. It had not been until the development of special advanced techniques and corrective-stabilizing structures in vertebrology that patients belonging to the respective category could get comprehensive assistance followed by due rehabilitation [11, 13]. Relevant scientific literature offers not enough information regarding the anatomy of intervertebral foramina, the topographic, individual and typological variability, and the nature of the connection and correlation between the shape and the morpho-topometric features [1, 5, 6, 10]. A decrease in the intervertebral foramen size may play a role in case of the neurovascular component compression, e.g., when dealing with a herniated disc, osteochondrosis, scoliosis on the deformity concave side, or an injured thoracic spine [4, 8]. A growth in the number of the thoracic spine endoscopic and minimally invasive interventions, as well as the possibilities offered by 3D modeling [3, 7] requires detailed data on the thoracic spine morphology in general, and on the anatomy of intervertebral foramina in particular [1, 5].
Aim of the study – to investigate the variability patterns affecting the size and the shape of intervertebral foramina in mature persons without degenerative dystrophic changes involving the thoracic spine.
The study relied on 120 CT scans of thoracic spine of adult men aged 21-40 without signs of degenerative dystrophic changes. The images were obtained from the archive of the Research Institute of Traumatology, Orthopedics and Neurosurgery of the Saratov State Medical University (Saratov, Russia). The lateral projection of the CT scans was used to identify counter-lateral dimensions (vertical and horizontal diameters) and the shape of the intervertebral foramina (IVF). If there were no statistically significant bilateral differences in the foramen sizes, the values of the left foramina were registered.
The variational-statistical processing of the obtained data was carried out parametrically. Therefore, when checking the distribution normality based on the Shapiro-Wilk criterion, the distribution was close to normal. The following values were calculated – amplitude (Min-Max), arithmetic mean (M), mean error (m), standard deviation (SD). The significance of the differences was identified through the Student’s t-test. The differences were considered statistically significant at p<0.05 (95% probability threshold). The variability coefficient was determined as Cv%=SD/M×100, where the variability of the features was considered low at Cv% <10%; average – at Cv% within the range of 11 to 30%, and high – above 30%. The extensiveness coefficient was defined as a relative value pointing at how large a separate part was in relation to the entire population studied (occurrence frequency).
The intervertebral foramina sizes as well as the vertical and horizontal diameters increase in the thoracic spine cervical-lumbar direction from 10.4 ± 0.2 to 15.2± 0.3 mm (by 31.6%) and from 5.4± 0.1 to 6.5± 0.2 mm (by 16.9%), respectively. The most convincing (maximum) increase in the foramen size was to be observed at the distal thoracic spine level. The vertical diameter of the Th11-12 foramen increases relative to the Th10-11 foramen by 10.5% (the differences are statistically significant, p= 0.02), the horizontal diameter of the foramen at the same level has a relative increase of 8.3%, which is statistically significant as well, p=0.04 (Table 1).
Table 1. Topographic variability of intervertebral foramina vertical and horizontal diameters
| Foramen | IVF vertical diameter | IVF horizontal diameter | ||||||||||
| Min | Max | M | m | SD | Cv | Min | Max | M | m | SD | Cv | |
| Th1-2 | 6,3 | 15,5 | 10,4 | 0,2 | 1,8 | 17,2 | 3,9 | 8,4 | 5,4 | 0,1 | 1,1 | 17,6 |
| Th2-3 | 7,1 | 14,7 | 10,5 | 0,2 | 1,5 | 14,8 | 3,5 | 7,6 | 5,5 | 0,1 | 1,0 | 17,8 |
| Th3-4 | 4,3 | 14,3 | 10,7 | 0,2 | 1,7 | 16,4 | 4,0 | 9,2 | 5,5 | 0,1 | 1,1 | 18,7 |
| Th4-5 | 7,7 | 15,5 | 11,2 | 0,2 | 1,7 | 15,1 | 3,9 | 7,7 | 5,6 | 0,1 | 0,9 | 15,4 |
| Th5-6 | 8,9 | 18,4 | 12,5 | 0,2 | 1,9 | 15,3 | 3,4 | 8,5 | 5,6 | 0,1 | 1,1 | 19,9 |
| Th6-7 | 7,9 | 19,0 | 12,7 | 0,3 | 2,2 | 17,4 | 2,8 | 9,4 | 5,6 | 0,2 | 1,3 | 22,8 |
| Th7-8 | 7,5 | 17,1 | 12,8 | 0,2 | 1,9 | 14,8 | 3,4 | 8,7 | 5,7 | 0,2 | 1,2 | 21,2 |
| Th8-9 | 6,0 | 17,6 | 12,5 | 0,3 | 2,4 | 19,6 | 2,5 | 8,2 | 5,7 | 0,1 | 1,2 | 20,9 |
| Th9-10 | 7,1 | 17,6 | 12,7 | 0,3 | 2,1 | 16,8 | 3,2 | 7,4 | 5,8 | 0,1 | 0,9 | 17,4 |
| Th10-11 | 8,6 | 20,5 | 13,6 | 0,3 | 2,5 | 18,6 | 3,2 | 8,6 | 6,0 | 0,2 | 1,3 | 22,8 |
| Th11-12 | 8,0 | 19,8 | 15,2 | 0,3 | 2,3 | 15,4 | 3,6 | 9,3 | 6,5 | 0,2 | 1,2 | 18,5 |
Both sizes of IVF feature an average degree of variability, while the horizontal diameter is variable to a slightly greater extent (the variation coefficient falls within the range of 15.4 through 22.8%) if matched against the vertical one (the variation coefficient of 14.8-19.6%).
When identifying the IVF shapes in geometric terms, there were four shapes identified: oval, rounded, four-sided, and three-sided (see Figure 1).
The oval shape was found in 42.4% of the cases (1119 foramina out of 2640). The three-sided shape proved to be the second most common one – 26.6% of the cases (703 cases out of 2640). The four-sided shape was observed in 19.8% of the cases (522 foramina out of 2640), the rounded shape being less common – 11.2% of the cases (296 foramina out of 2640) (Table 2).
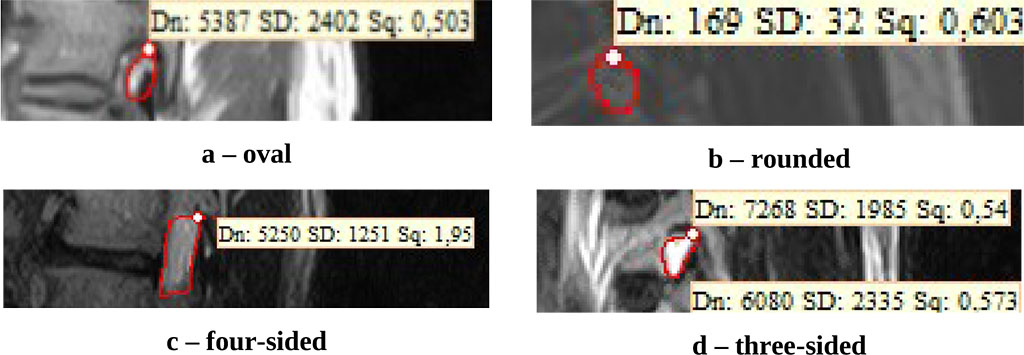
Figure 1. IVF shapes
Table 2. IVF shapes extensiveness depending on location the level
| Foramen | Oval | Rounded | Four-sided | Three-sided | Total | |||||
| Abs. | %% | Abs. | %% | Abs. | %% | Abs. | %% | Abs. | %% | |
| Th1-2 | 63 | 26,3 | 85 | 35,4 | 47 | 19,6 | 45 | 18,8 | 240 | 100 |
| Th2-3 | 91 | 37,9 | 36 | 15,0 | 53 | 22,1 | 60 | 25,0 | 240 | 100 |
| Th3-4 | 66 | 27,5 | 40 | 16,7 | 66 | 27,5 | 68 | 28,3 | 240 | 100 |
| Th4-5 | 87 | 36,3 | 24 | 10,0 | 57 | 23,8 | 72 | 30,0 | 240 | 100 |
| Th5-6 | 93 | 38,8 | 18 | 7,5 | 37 | 15,4 | 92 | 38,3 | 240 | 100 |
| Th6-7 | 87 | 36,3 | 15 | 6,3 | 48 | 20,0 | 90 | 37,5 | 240 | 100 |
| Th7-8 | 112 | 46,7 | 18 | 7,5 | 38 | 15,8 | 72 | 30,0 | 240 | 100 |
| Th8-9 | 106 | 44,2 | 18 | 7,5 | 41 | 17,1 | 75 | 31,3 | 240 | 100 |
| Th9-10 | 123 | 51,3 | 9 | 3,8 | 33 | 13,8 | 75 | 31,3 | 240 | 100 |
| Th10-11 | 147 | 61,3 | 6 | 2,5 | 54 | 22,5 | 33 | 13,8 | 240 | 100 |
| Th11-12 | 144 | 60,0 | 27 | 11,3 | 48 | 20,0 | 21 | 8,8 | 240 | 100 |
| Total | 1119 | 42,4 | 296 | 11,2 | 522 | 19,8 | 703 | 26,6 | 2640 | 100 |
In view of the foramen location level in the thoracic spine, the various IVF shapes featured uneven distribution. Oval-shaped foramina proved more common in the distal part, at the Th7-8 – Th11-12 level (106-147 foramina); rounded shapes, on the contrary, were more common in the proximal part, at the Th1-2 – Th3-4 foramina level (36-85 holes). The three-sided foramina were often noted at the thoracic spine mid-level, in the thoracic kyphosis area (Th4-5 – Th9-10 level) (72-92 foramina). The most uniform distribution was typical of the four-sided IVF shape. Bilateral symmetry of IVF shapes was observed in 86% of the cases (2.270 foramina out of 2.640), with only 14% of the foramina shapes showing no match when comparing the left and the right sides.
Given the above, the size of the intervertebral foramina in the thoracic spine increases along with an increase in the vertebrae massiveness in the cervical-lumbar direction; the vertical diameter of the vertebrae increases most intensively if compared to the horizontal one, which, in turn, features a slightly greater variability.
There were four shapes of intervertebral foramina identified through the thoracic spine (oval, rounded, four-sided, three-sided). The extensiveness of the various shapes differs and varies depending on the foramen topographic location, which, obviously, is due to a change in the direction of the forces that have an effect on the anterior, middle, and posterior spine support columns.