- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 3: e1. DOI 10.35630/2199-885X/2022/12/3.19
The article presents a clinical case of a rare variant of scarring alopecia - Folliculitis decalvans. It is known that pregnancy provokes or worsens the course of many skin diseases. The given clinical case clearly shows that pregnancy has become a trigger for the development of folliculitis decalvans at the site of a former injury. The article describes the characteristic clinical manifestations of Folliculitis decalvans and its trichoscopic criteria, as well as a review of studies dealing with various methods of the treatment. Any methods of systemic treatment of folliculitis decalvans are undesirable or prohibited during pregnancy, so topical treatment with drugs with proven effectiveness is the option of choice for this category of patients.
Keywords: folliculitis decalvans, scarring alopecia, pregnancy, tufted hairs
Folliculitis decalvans (FD) is a primary scarring alopecia that is based on chronic neutrophilic inflammation of the hair follicle. In terms of frequency of occurrence, FD is the third most common primary scarring alopecia, behind lichen planus and discoid lupus erythematosus. The first episode usually occurs at the age of 30-40 years, more often in men, however, among patients with FD 50 years and older, it is more predominant in women [10].
Folliculitis decalvans is a chronic inflammatory disease of the scalp, characterized by the presence of pustules, crusts, "tufted" hairs ("tufted hairs" - more than 5 hair shafts, emerging from one opening of the hair follicle) and perifollicular hyperkeratosis, which results in the formation of foci of scarring alopecia on the scalp [8, 10].
The etiopathogenesis of the disease is not definitively established. However, a significant component of etiopathogenesis is probably the colonization of Staphylococcus aureus in the focus of inflammation, since this microorganism is often detected during microbiological examination of pustules [10]. According to a culture study of pustules on the scalp of 32 patients with FD, conducted by Miguel-Gomez L. et al., 72% have S. aureus, 3% have S. epidermidis, and the rest of the examined cultures were negative. Presence of S.aureus in the nasal mucosa. may affect the recurrence rate of Folliculitis decalvans. Culture study of nasal discharge was performed in 10 patients, with S. aureus was detected in 4 subjects, the rest were negative [1].
Triggers for the occurrence of FD may include: family history, stressful situations, scalp injuries, pregnancy, and reduced resistance of the body, due to diabetes mellitus, chronic nephritis and other immunosuppressive factors. The relationship between FD and comorbidities has been studied by many researchers. According to the data of Miguel-Gomez L. et al., who examined 60 patients suffering from DF, 65% of patients at the time of diagnosis did not have concomitant diseases, the rest were found to have: arterial hypertension, pollinosis, obesity, etc., 48% - had concomitant dermatological diseases: androgenetic alopecia, atopic dermatitis, seborrheic dermatitis, psoriasis, etc. [1].
The most reasonable mechanism of pathogenesis of FD is a combination of a trigger factor and a disruption between the "local" immune response and the microbiome (colonization of Staphylococcus aureus), which in turn leads to increased migration of neutrophilic cells to the epidermis around the hair follicles and directly to the dermis. Neutrophils can enter the follicle and cause damage to its epithelium (through phagocytosis S. aureus triggers a chronic inflammatory process). As a result, FD leads to lichenoid inflammation with subsequent skin atrophy and, as a result, scarring alopecia. Histological examination reveals an infiltrate consisting mostly of neutrophilic cells in the early stages of FD, and perifollicular dermal fibrosis in the later stages [10].
Over a background of gestation, a number of changes occur aimed at preserving pregnancy and preventing fetal rejection. These include, first of all, the enhanced of humoral immunity and the production of Th2-cytokines (IL-4, IL-10). Under the influence of IL-10, high levels of estrogens and PGE2, cellular immunity and the production of Th1 cytokines (IL-2, IFN-γ, IL-12) are inhibited. Additionally, the inhibition of cellular immune response and the development of physiological immunosuppression in turn leads to increased levels of progesterone, cortisol, and chorionic gonadotropin [11, 12].
Clinical signs of FD are: a focus of scarring alopecia on the scalp with tufted (more than 5 hair rods from one follicle) hair growth, the presence of follicular pustules and crusts. The focus of scarring alopecia is usually single, however, multiple foci may be present in some cases. Patients complain of painful sensations in the area of the alopecia focus (trichodynia), burning sensation, itching, bleeding when pustules and crusts are damaged [8]. According to a study by Miguel-Gomez L. et al., 42 patients (70%) complained of pruritus, and 28 patients (46.6%) were affected by trichodynia. Pustules and crusts were detected in 42 patients (70%), seborrhea - in 23 (38.3%), "tufted hair" - in 51 (85%), erythema - in 44 (73.3%), perifollicular hyperkeratosis — in 34 (56.6%), facial papules - in 2 patients (3.3%) [1].
The diagnostic methods used for FD are: physical examination, trichoscopy, diagnostic biopsy of the affected skin area followed by morphological examination for differential diagnosis with other scarring and non-scarring alopecia, and bacteriological culture study with antibiotic sensitivity test from the discharge of scalp pustules and nasal mucosa [8,9,13,149,13,14]. According to a study by Fernández-Crehuet P. etal., there is no statistically significant relationship between the severity of the disease and the results of trichoscopy [3]. However, an article by Vanó-Galván S. et al. showed that the presence of pustules is an independent factor in severe cases of FD [2]. In the acute stage of FD, trichoscopic signs of FD are found: tufted hair, superficial follicular pustules, the presence of a large number of yellowish scales, "honey" crusts lying perifollicularly over a background of erythema and spot hemorrhages. In the chronic stage, white dots without follicular openings and perifollicurian hyperkeratosis are detected. In doubtful cases, the patient is indicated to perform a diagnostic biopsy, which can detect inflammatory infiltrate from neutrophils and perifollicular fibrosis [9, 10].
Treatment of folliculitis decalvans, which results in scarring alopecia, is one of the most difficult tasks in trichology. The effectiveness of treatment depends on the timely detection and the size of the lesion. The main goal of treatment is to stop the inflammation and progression of scarring alopecia. However, the treatment of the disease is long-term and does not prevent relapses. Maintenance therapy and elimination of trigger factors can prolong disease remission [6, 14].
The results of FD treatment were discussed in 20 studies involving 282 patients, 73.4% of whom were men. Bunagan M.J., Banka N. и Shapiro J. Demonstrated in their study that a 10-week course of clindamycin and rifampicin allowed remission from 2 to 12 months in 10 out of 18 patients (55.6%), the longest FD remission was achieved was 7.2 months. The remission period was shorter among those treated with doxycycline or azithromycin for 3-6 months. Additional treatment with oral antibiotics, isotretinoin, or clobetasol lotion was required in 11 out of 23 patients to maintain the remission [4].
As study was conducted in which 39 male patients participated, with an average age of 37.9 ± 15.5 years. All patients received isotretinoin orally at a dose of 0.1-1 mg / kg / day (up to 90 mg /day.) for 2.5-8 months. Clinical recovery was observed in 82% of patients. Patients who received oral isotretinoin at a dose of ≥0.4 mg / kg /day. for ≥3 months responded better and 66% of them did not relapse for a longtime. Contrary to popular belief, oral isotretinoin monotherapy resulted in a complete response in the majority of patients in this study. Based on this discovery, oral isotretinoin at a dose of ≥0.4 mg/kg/day. should be administered for ≥3 months to minimize the likelihood of relapse. Oral isotretinoin monotherapy should be considered as a promising alternative for the treatment of folliculitis decalvans instead of treatment with antibiotics, but this requires further research [5].
There are indications that treatment with activation in the red light spectrum led to clinical improvement in 9 out of 10 patients, while long-term remission was achieved in 6 patients.Other methods of treatment with a low level of evidence are described using tacrolimus ointment, human immunoglobulin, adalimumab, infliximab [6].
Thus, the evaluated studies did not have a sufficient sample group, there were no control groups, and they were not randomized. The combination of clindamycin and rifampicin is the most effective. The lack of higher level evidence highlights the need for new studies to evaluate treatment methods of FD, but its rare occurrence complicates this task [7].
We have been monitoring female patient I., 25 years old with a diagnosis of "folliculitis decalvans", concomitant condition-pregnancy of 20 weeks, since November 2021.
Anamnesis morbi. The patient’s primary complains on the first visit were that of pain, itching and burning on the scalp, as well as superficial bleeding during scratching. At the age of 5, the patient was bitten by a dog, after which multiple scars had been formed on the scalp. In July 2021, at 16 weeks of pregnancy, rashes appeared around the scars, and therefore patient I. decided to visit a dermatologist.
Dermatological status. The pathological process is localized on the scalp, on the crown of the head. There is a focus of scarring alopecia, irregularly shaped, up to 10 cm in diameter. In the central part of the scar, there is an ulcer defect with purulent-hemorrhagic discharge. On the periphery of the defect – follicular pustules, as well as purulent and hemorrhagic crusts are located around the hair follicles. There is a tuft-like growth of hair – 5 or more hair shafts that come out of one widened follicle (Fig. 1)

Fig 1. Ulcer defect over a background of erythematous skin. Multiple pustulo-hemorrhagic crusts. Tufted hair growth.
Physical, laboratory and instrumental studies at the time of treatment did not reveal any deviations from the average indicators of age and gender norms. The patient refused to get a histological examination done.
Dermatoscopy. Pronounced perifollicular hyperkeratosis and multiple purulent-hemorrhagic crusts, follicular pustules, lost hair follicular openings (fibrotic white dots) (Fig 2).
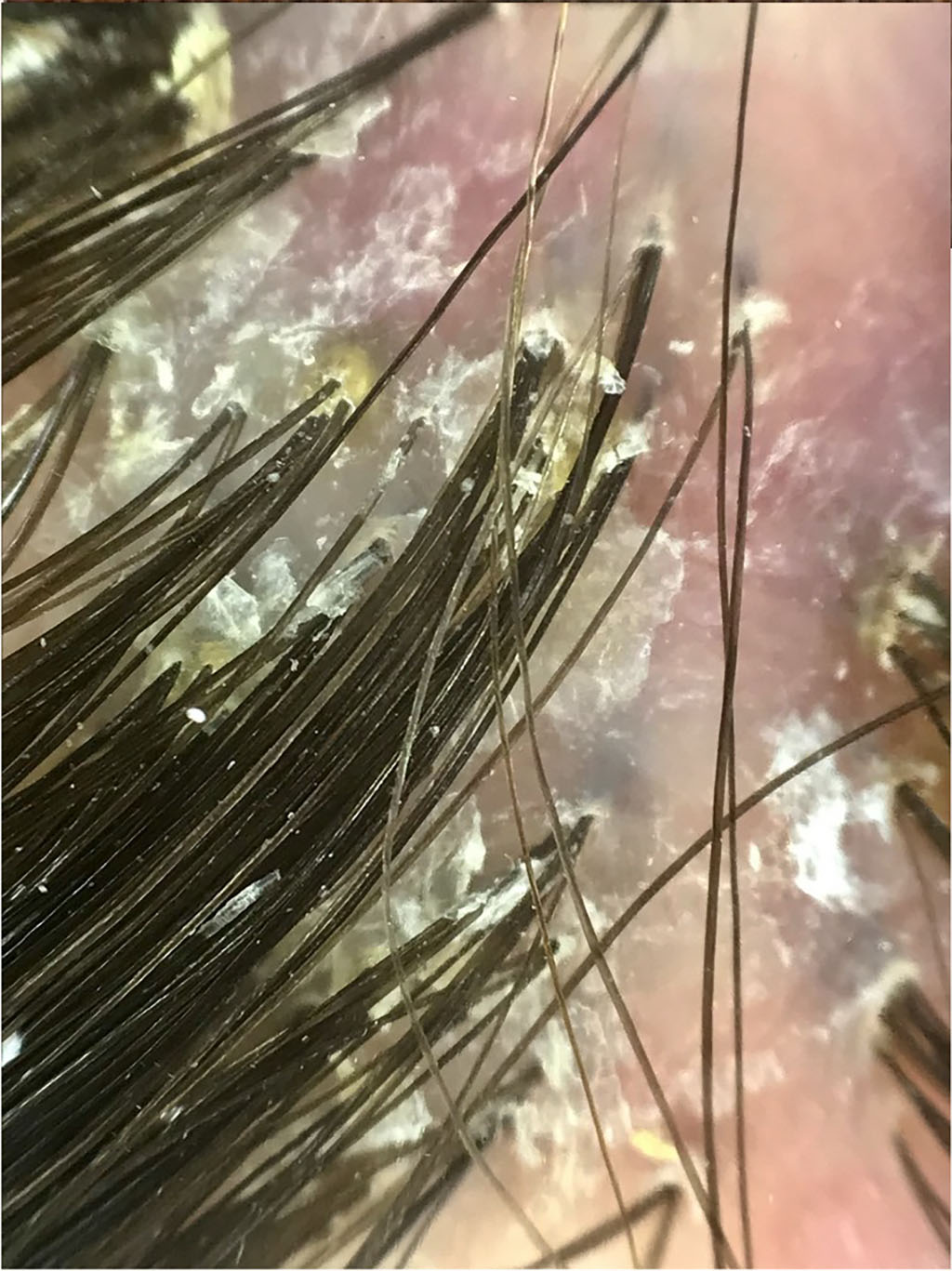
Fig 2. Perifollicular hyperkeratosis. Follicular pustules. Lost hair follicle opening.
Treatment. Due to pregnancy, despite the severity of the disease, systemic treatment and local administration of glucocorticosteroids were not prescribed. For 3 months, the treatment was carried out only topically. A shampoo containing salicylic and glycolic acids and micronized sulfur was used. The ulcer defect was treated with 0.05% chlorhexidine bigluconate solution, and creams with fusidic acid and its combination with betamethasone were applied. Over the course of the treatment, the symptoms disappeared, the pustules were resolved, the ulcer defect was epithelized, and the perifollicular hyperkeratosis was partially preserved. The phenomena of scarring alopecia, tufted hair of more than 6 from one unit (up to 15 in some places) remained unchanged (Fig 3). Until the end of pregnancy, the therapeutic shampoo with exposure is recommended.

Fig 3. – Epithelization of ulcer defect with the formation of scarring alopecia. Tufted hair growth.
It is known that pregnancy provokes or worsens the course of many skin diseases. The given clinical case clearly shows that pregnancy was a trigger for the development of FD at the site of a former injury. Immunological and endocrinological changes that occurred during pregnancy led to the formation of a severe form of FD. In addition, during gestation, physiological vascular changes occur, including increased blood flow to the skin. These factors were predisposing to the appearance of an ulcer defect and pronounced symptoms of Folliculitis decalvans. Methods of systemic treatment of FD are undesirable or prohibited during pregnancy, so it is necessary to focus on topical therapy.