- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
The study presents the experience of surgical treatment for deforming osteoarthritis of the knee joint of II-III stage, with axial deformations in 75 patients. Supracondylar varus resection osteotomies of the femur and supratuberous valgus osteotomies of the tibia were performed depending on the knee joint deformities. The results of these surgical interventions were evaluated according to the methods developed in our clinic. Good results were obtained in 74% of cases, satisfactory - in 26% of cases.
Keywords: knee joint, corrective osteotomy, deforming arthrosis, varus deformity, valgus deformity.
Deforming arthrosis, also known as osteoarthrosis (OA), osteoarthritis, is the most common multifactorial joint disease, which is characterized by chronic pain syndrome, functional disability, and a significantly decreased quality of life in the patients [1]. According to the data of epidemiological studies, 10-20% of the population currently suffers from OA worldwide, and in 10% of cases, the disease is the cause of permanent disablement and disability [2-4]. Among the OA of major joints, one of the most pressing problems is knee joint damage - gonarthrosis, which is currently recognized as the most common form of OA [5]. OA of knee joint accounts for nearly 4/5 of the OA burden globally. This frequency is associated with the aging of the world population, as well as the obesity pandemic [6]. According to statistics, 7-22% of people in the world suffer from diseases of the knee joint. In the early stages of the disease, various methods of conservative and surgical treatment are used [7-11]. And although the development of modern medicine today makes it possible to effectively identify and treat patients with pathology of the musculoskeletal system, OA of the knee joint still remains an incurable disease, since patients usually seek medical help in the late stages of the disease, when conservative therapy is ineffective. The progression of gonarthrosis leads to the development or increase in the deformation of the knee joints in 32 - 65% of patients [12].
The purpose of this study was to improve the results of treatment in patients with gonarthrosis due to the use of a differentiated approach to the choice of reconstructive surgery, depending on the type of knee joint deformity.
We analyzed the results of surgical treatment in 75 patients with deforming osteoarthritis of the knee joint of II-III stage (according to Kellgren) [13]. There were 49 women and 26 men, the average age of the patients was 54.7 years.
Juxta-articular osteotomies were chosen, considering the following criteria:
Depending on the existing symptoms, the patients underwent: corrective osteotomies of the tibia, arthroscopic interventions in combination with corrective supratuberous tibial osteotomies and supracondylar osteotomies of the femur (Table 1)
In the case of varus deformities of the knee joint, which are caused by an abnormality of the axis of the tibia, which was radiographically manifested by a decrease in the basotibial angle, we performed a supratuberous corrective osteotomy of the tibia using autogenous grafts of the appropriate size of iliac wing, and used stable and functional osteosynthesis with plates. According to this technique, 68 patients were operated on (Fig. 1)
In the presence of degenerative damage to the menisci on MRI, which was clinically manifested by flexion contracture or joint block, the corrective osteotomy of the tibia was supplemented with arthroscopic intervention. 5 patients were operated on according to this technique.
In case of deformations of the knee joint space due to a abnormality of the axis of the femur, which was radiologically manifested by a change in the basofemoral angle, we performed a supracondylar corrective osteotomy of the femur with wedge resection and metallic osteosynthesis using plates. According to this technique, 11 patients were operated on (Fig. 7).
Table 1. Distribution of Patients According to the Type of Operative Interventions
| Designation of the operation | Number of patients | Number of operations |
| Supratuberous corrective osteotomy | 59 | 59 |
| Supratuberous corrective osteotomy + arthroscopy of knee joint | 5 | 5 |
| Supracondylar corrective osteotomy | 11 | 11 |
| Total | 75 | 75 |
In 5 patients with osteoarthritis of the knee joint with valgus deformity, during supracondylar osteotomy of the femur, we used an individual navigation system (INS) for more accurate correction and simplification of the operation (Fig. 6, 7, 8). The uniqueness of the INS consists primarily in the manufacture of an individual implant, so-called custom-made implant, which will ideally fit the bone geometry of a specific patient, taking into account all its defects. That is, INS opens the possibility of personalized surgery. INSs are manufactured using 3D printing of biocompatible photopolymer resins or plastic. After sterilization, it can be used during surgery. In order to visualize the bones, computerized tomography of the anatomical segment is performed with minimal slice thickness (≤1 mm). When basing the INS, first of all, its location on the bone is determined, which can be exposed by the surgeon during surgery. As a rule, it coincides with the top of bone deficiency. The surface of the base of the navigation system molds the contours of the bone, so the unevenness of the bone in the base area facilitates the fixation of the INS during surgery. The dimensions of the navigator as a whole should be as small as possible, without losing the strength of its structure and the reliability of its fixation. The direction of the slots coincides with the planes of the osteotomy, which are calculated by the bioengineer together with the surgeon, according to the operative plan. It is necessary to design the thickness of the slots by 0.5 mm greater than the thickness of the oscillating saw blade. The length of the slots should provide free movement for the saw blade, which is necessary for sawing the full diameter of the bone. INS is fixed to the bone with pins. It is recommended to design at least three holes for pins per the distal and proximal parts of the bone. FDM (Fused Deposition Modeling) - modeling by surfacing method - is often used to create an individual mockup-prototype on a 1:1 scale. The object is formed by layer-by-layer laying of the molten thread of a fusible working material. It is advisable to use printers with a construction camera of 300x300x300mm.
The operated patients were observed from 2 to 9 years after surgery. In order to evaluate the results of the treatment, we developed a scoring system for the functional state of the knee joint (Table 2), which was supplemented with the Lequesne algofunctional index [14] (Table 3). In order to evaluate the results of treatment, 7 parameters (criteria) were taken into account, each of which was evaluated with a numerical expression of 3, 2 or 1 point. The following criteria are taken into account in this system: the patient's subjective assessment of the state of the knee joint, pain, range of motion, support ability, flexion contracture, limping, deformation of the knee joint in the frontal plane.
Table 2. A System for Evaluating the Results of Treatment of Patients with Gonarthrosis
| Criteria | Scores | ||
| 3 | 2 | ||
| Subjective assessment of the state of the knee joint by the patient | Good | Satisfactory (complaints about slight impairment of limb function) | |
| Pain | Absent | Moderate in case of physical exertion | |
| Range of motion | More than 90° | More than 80° | |
| Flexion contracture | Absent | Up to 10° | |
| Support ability | Preserved | Moderately disordered | |
| Limping | Absent | Moderate | |
| Varus (valgus deformity) of the knee joint | 0–50 | 60–100 | |
If the total score was 18-14, we considered it a good result, 13-10 - satisfactory, 9-6 - unsatisfactory.
Table 3. Lequesne Algofunctional Index for Gonarthrosis
| Criteria | Scores |
| 1 | 2 |
| Pain or discomfort | |
| Night pain | |
| Only
when moving in a certain position Even at rest |
1 2 |
| Morning stiffness or pain after sleep | |
| Less
than 15 minutes. More than 15 minutes. |
1 2 |
| Pain occurs when walking | |
| Only
after passing a certain distance Immediately and then intensifies |
1 2 |
| 2. Maximum pain-free walking distance | |
| More
than 1 km, but with rest About 1 km. From 500 to 900 m. From 300 to 500 m. From 100 to 300 m. Less than 100m. With one stick or crutch With two sticks or crutches |
1 2 3 4 5 6 +1 +2 |
| 3. The presence of difficulties in everyday life | |
| Can you climb one flight of stairs? Can you go down one flight of stairs? Can you put anything on the bottom shelf of the cupboard while kneeling? Can you walk on a bumpy road? Do you experience shooting pain or a sudden sensation of loss of support in the affected limb? sometimes often |
0–2 0–2 0–2 0–2 1 2 |
The sum of 21 - 17 points according to the Lequesne index from 1 to 5 points was considered good results, satisfactory: 17 - 10 according to the Lequesne index from 6 to 8 points, unsatisfactory - 9 or less according to the Lequesne index 9 or more points.
Good results were obtained in 74% (56 people), satisfactory - in 26% (19 people). the results of juxta-articular corrective osteotomies in patients with gonarthrosis with axial deformations are presented in Table 4.
Table 4. Analysis of the Effectiveness of Juxta-articular Corrective Osteotomies in the Treatment of Patients with Osteoarthrosis of the Knee Joint
| Result (scores) | Juxta-articular corrective osteotomies of the knee joint | |
| Supracondylar, people(%) | Supratuberous, people(%) | |
| Good (21-17) Lequesne index (1-5) | 11 | 45 |
| Satisfactory (17-10) Lequesne index (6-8) | 0 | 19 |
| Unsatisfactory ( ≥ 9 ) Lequesne index ( ≥ 9) | 0 | 0 |
| Total | 11 | 64 |
Patient P. is 55 years old. She referred to the clinic with complaints of pain and deformation in the right knee joint. At the time of reference, several clinical trials were carried out, according to the results of which a diagnosis was made: Left-sided gonarthrosis of the III stage varus deformities of the left knee joint (Fig. 1). The patient underwent a supratuberous valgus osteotomy of the right tibia, with bone autoplasty and МОС ХМ plate (Fig. 2)
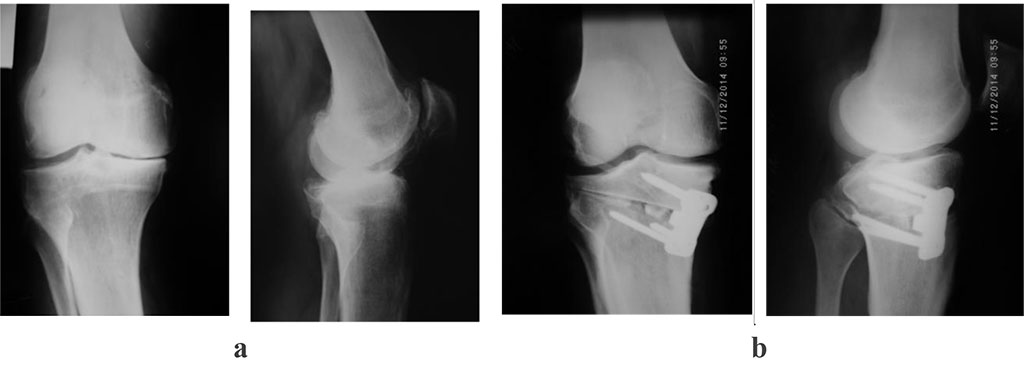
Figure 1: photoprints of radiographs of patient P., 55 years old, with a diagnosis of III stage left-sided gonarthrosis. varus deformities of the left knee joint. a – before surgery; b - after surgery: supratuberous valgus osteotomy of the right tibia, with bone autoplasty and МОС ХМ plate
Patient T. is 48 years old. He referred to the clinic with complaints of pain and deformity in the right knee joint. At the time of reference, several clinical trials were conducted, according to the results of which the patient was diagnosed with: bilateral gonarthrosis of the III stage with valgus deformity on the right and varus deformity on the left (Fig. 2).
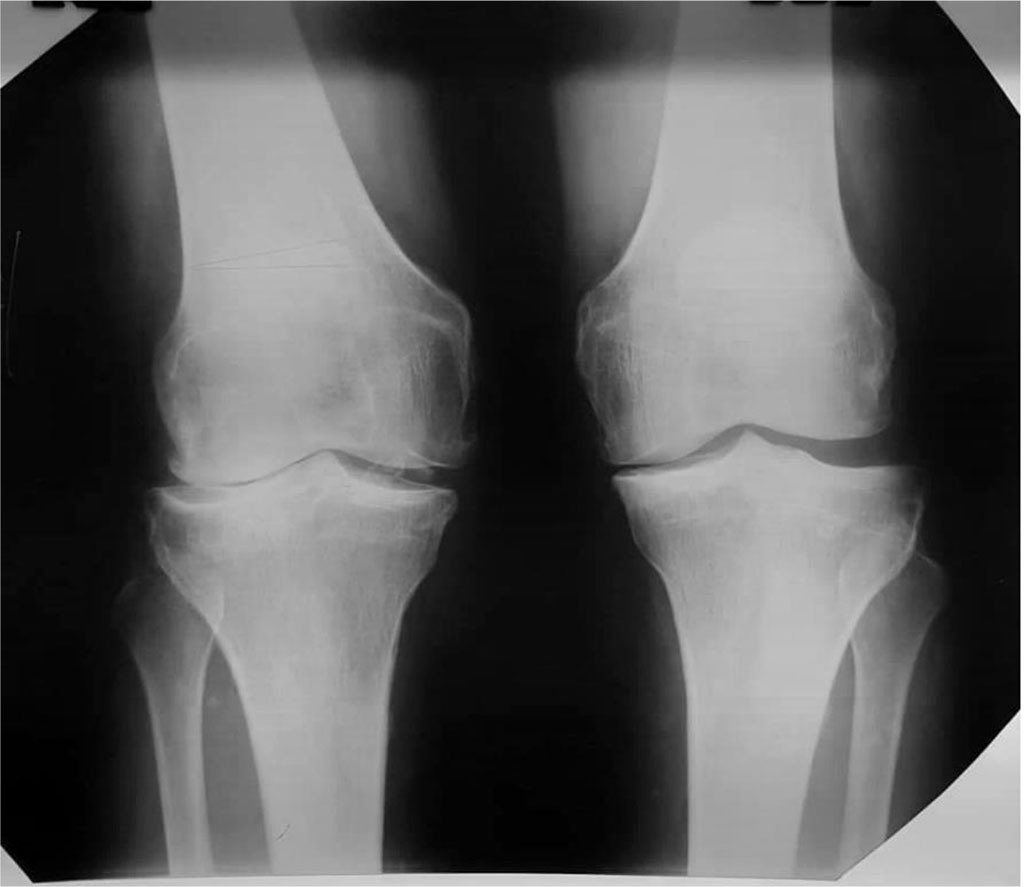
Figure 2. Radiographs of the knee joints before the operation in the loaded state.
The patient underwent supracondylar resection varus osteotomy of the right femur (Fig. 6).
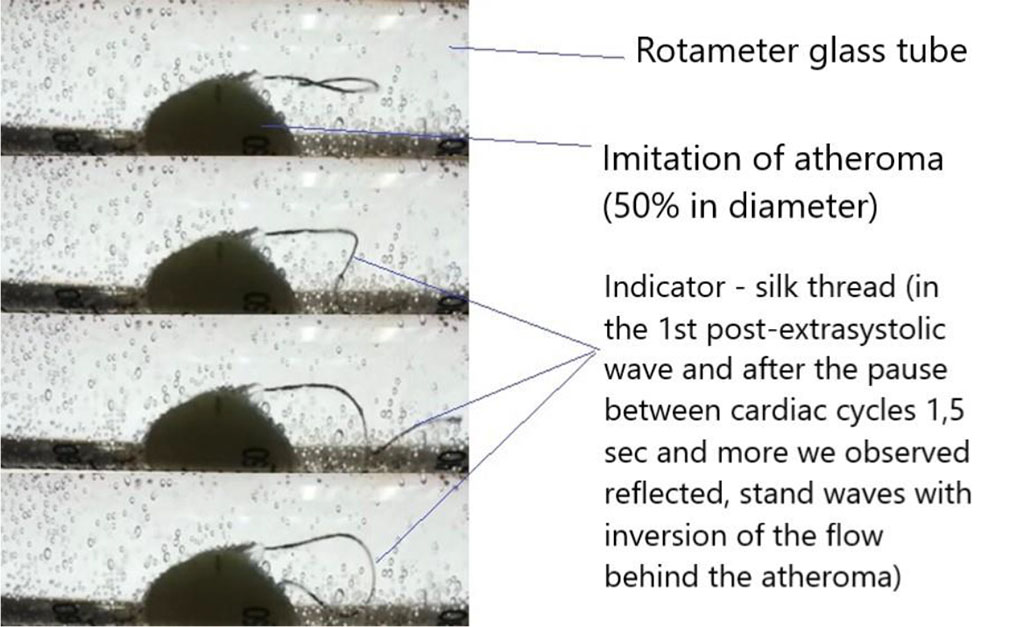
Figure 3. A 3D model of the right femur was made with INS for performing a supracondylar resection varus osteotomy.
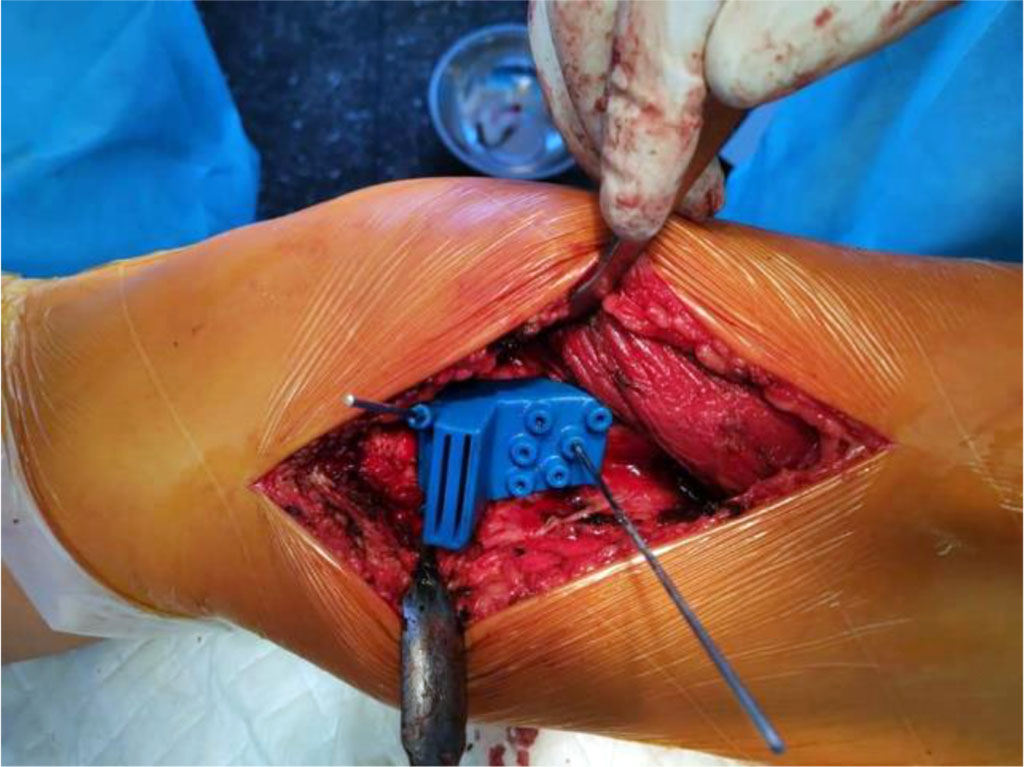
Figure 4. Appearance of INS in the operative wound

Figure 5. Appearance of the INS and bone wedge of the femur after resection
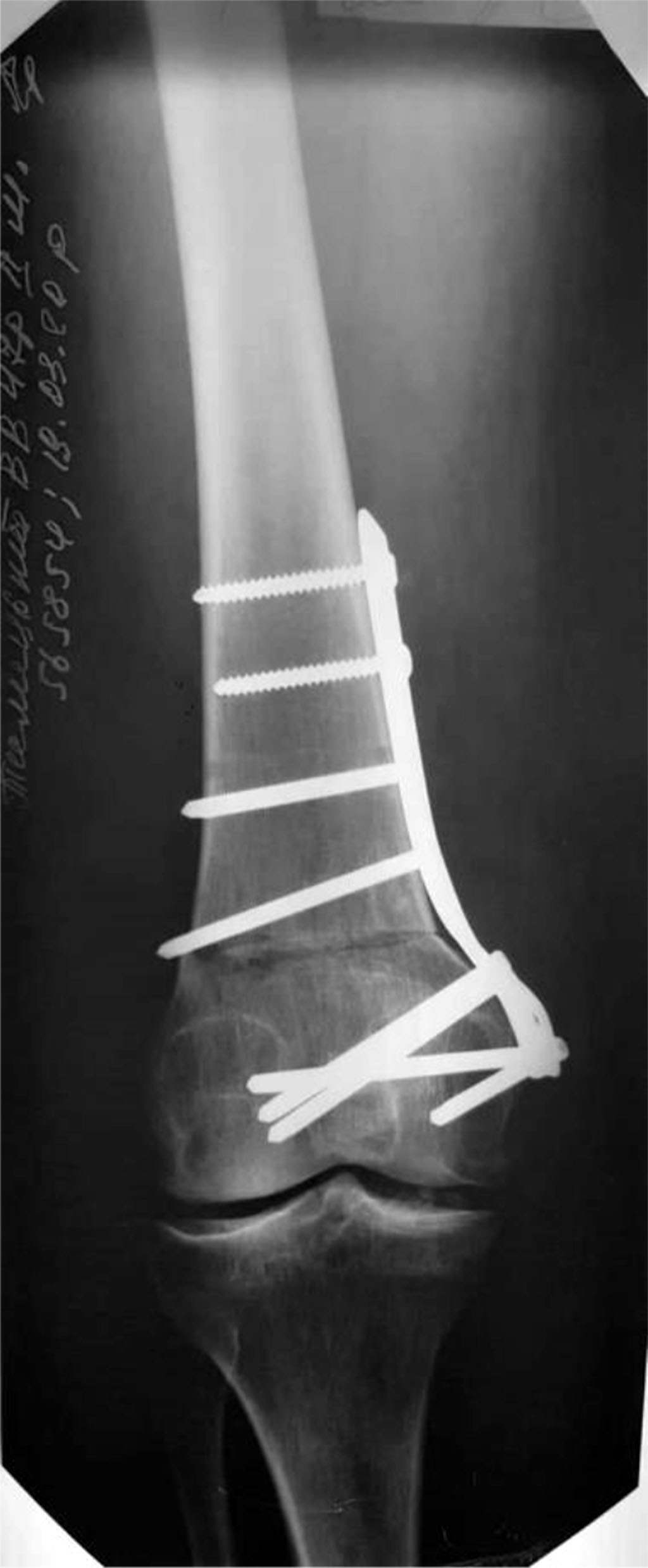
Figure 6. X-ray of the knee joint after carrying out supracondylar resection varus osteotomy of the right femur. With MOC LCR - plate.