- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Background: Antibiotic resistance is an issue of concern to physicians, scientists and patients. It has an impact on the increase of morbidity, length of hospital stay and mortality of patients. There is also a correlation between the resistance of bacteria to antibiotics and their geographical location.
Objective: Analysis of the prevalence of nosocomial skin and soft tissue infection pathogens and the rate of development of antimicrobial resistance in the Siberian and Far Eastern regions of Russia.
Methods: Data on microbial antimicrobial susceptibility and prevalence of major genetic determinants of antimicrobial resistance were analyzed. The work was carried out on the basis of data from the AMRmap online platform. Comparison of indicators was based on samples obtained from adult surgical patients with infected skin and soft tissues throughout 2016-2020 in the Siberian and Far Eastern regions of Russia.
Results: 5 microorganisms were identified in adult surgical patients with infected skin and soft tissues on the territory of the Siberian region and the Far Eastern region (Russia) in 2016-2020. They were Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli, Acinetobacter baumannii. The authors used the AMRmap online platform to study the sensitivity and resistance to various antibacterial drugs applied to the three most important pathogens in the regions.
Conclusions: The results indicate a rapid spread of resistance genes in the studied strains of Klebsiella pneumoniae, P. aeruginosa, S. aureus, E. coli, Acinetobacter baumannii. Systems for monitoring resistance to antibacterial drugs by laboratory methods need to be improved. It is also necessary to create new databases and improve the existing ones. These will help to select the optimal drug treatment strategy for patients according to their resistance profile.
Keywords: Sensitivity, antibiotic resistance, the Siberian region, the Far East region, antibacterial drugs, SSTI, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli, Acinetobacter baumannii.
Antibiotic resistance has become one of the most pressing global issues for healthcare professionals. Increasing microbial resistance to a wide range of antibiotics gradually reduces the effectiveness of prescribed treatment. That's the reason why the mortality rate is on the rise in many regions of the country.
In addition, many diseases caused by various bacteria are becoming more common and taking longer to treat. The emergence of microbial resistance is a natural biological response to the use of antimicrobial agents. It results in a selective effect, the survival and reproduction of resistant strains.
The problem has been worsening by the decline in the development and production of new antibacterial drugs.
It is important to note that diseases caused by resistant bacteria vary in their duration. A patient with such a disease will have to stay in the hospital for a long period of time. Doctors have to use second-line or third-line drugs when first-line drugs fail. These drugs tend to be more expensive and less safe, and they are not always available. All this increases the economic cost.
The development of molecular genetic technologies continues to contribute to the study of antibiotic resistance mechanisms. Sequencing helps to analyse the genetic structure of bacteria, which makes it possible to identify their local characteristics. It has been demonstrated that international clones with a high epidemic risk, capable of spreading rapidly, pose the greatest threat. In this context, monitoring the molecular epidemiology of priority pathogens is an important tool for monitoring the spread of antibiotic-resistant bacterial strains and developing measures to prevent them.
The aim: to analyse the prevalence of pathogens of nosocomial skin and soft tissue infections (SSTI) and the rate of development of antibiotic resistance in the Eastern part of Russia (Siberia and the Far East)
Analysis of data on the sensitivity of microorganisms to antimicrobial drugs and the prevalence of the main genetic determinants of resistance to antimicrobial drugs was conducted. Comparison of indicators was based on samples obtained from adult surgical patients with infected skin and soft tissues. The data was collected in 2 federal districts of Russia in the period from 2016 to 2020.
We analyzed the data from the AMRmap online platform. The results are presented as the percentage of isolates that are resistant and susceptible to increased exposure to a particular antibiotic or group of antibiotics. The priority sequence R/I/S is used to assign a pathogen to a specific sensitivity category. Maximum antibiotic resistance has been defined as resistance R to one or more drugs, intermediate susceptibility or susceptibility with increasing exposure as I, and hypersusceptibility to antibiotics as S.
Klebsiella pneumoniae (29%) ranks first as one of the most common pathogens of nosocomial infections in the Siberian region for the period 2016-2020. The second most common microorganism is Pseudomonas aeruginosa (18%). Staphylococcus aureus (16%) is also in the top three of the microorganisms.
Klebsiella pneumoniae is a member of the Enterobacteriaceae family of microorganisms. It is a gram-negative, encapsulated (real capsule), non-motile bacterium. The capsule allows the bacteria to defend itself against the body's immune response to destroy the pathogen, such as phagocytosis. They are widely distributed among water, soil and living things. K. pneumoniae can spread from the surface of mucous membranes to other tissues and cause life-threatening infections, most commonly pneumonia.
Pseudomonas aeruginosa is a gram-negative, aerobic, motile, rod-shaped bacterium. It is practically nothing it needs to survive and reproduce. It will grow and multiply in distilled water for up to 2.5 months, even though it will reduce its activity by a factor of ten. Its ideal environment is a dark, warm and humid place in the body (wounds, lower respiratory tract, urinary tract). It causes dermatitis and pyoderma of the skin.
Staphylococcus aureus is a spherical, gram-positive bacterium of the genus Staphylococcus. The frequency of colonisation of open biocenoses by Staphylococcus aureus is in the range of 25-30%. Under conditions of high temperature and humidity, infections caused by this type of microorganism occur. It is also associated with damaged skin, surgical interventions and injections. Staphylococcus aureus causes purulent-inflammatory processes in organs and tissues. They include boils, abscesses, phlegmon, osteomyelitis, mastitis and other inflammatory processes.
Staphylococcus aureus has a high level of sensitivity (100%) to antibiotics: Ceftaroline, Fusidic acid, Linezolid, Rifampicin, Trimethoprim-sulfamethoxazole, Tigecycline, Telavancin, Tedizolid, Vancomycin.
Staphylococcus aureus is most resistant to Ciprofloxacin and Erythromycin (44.5%) among all antibiotics used in Sibircky federal district (Figure 1).
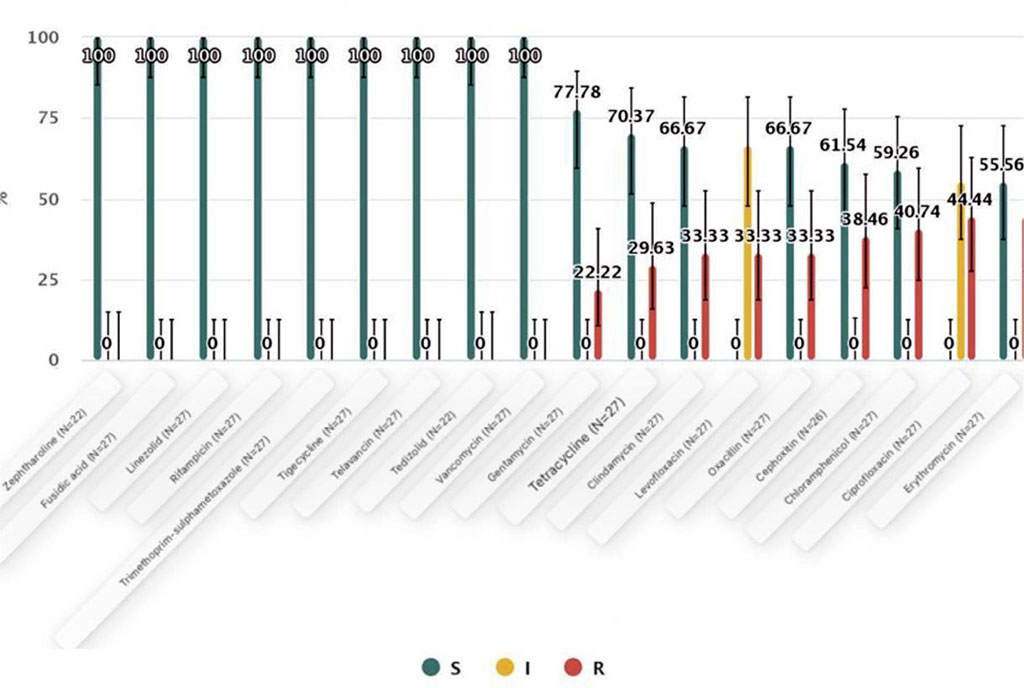
Figure 1: Antibiotics SIR summary of Staphylococcus aureus in the Siberian region.
The gram-negative aerobe Pseudomonas aeruginosa is absolutely sensitive to Colistin (100%) in the Sibircky federal district. The maximum resistance of this microorganism was revealed to the antibiotics Ciprofloxacin and Imipenem (83.4%) (Fig. 2).
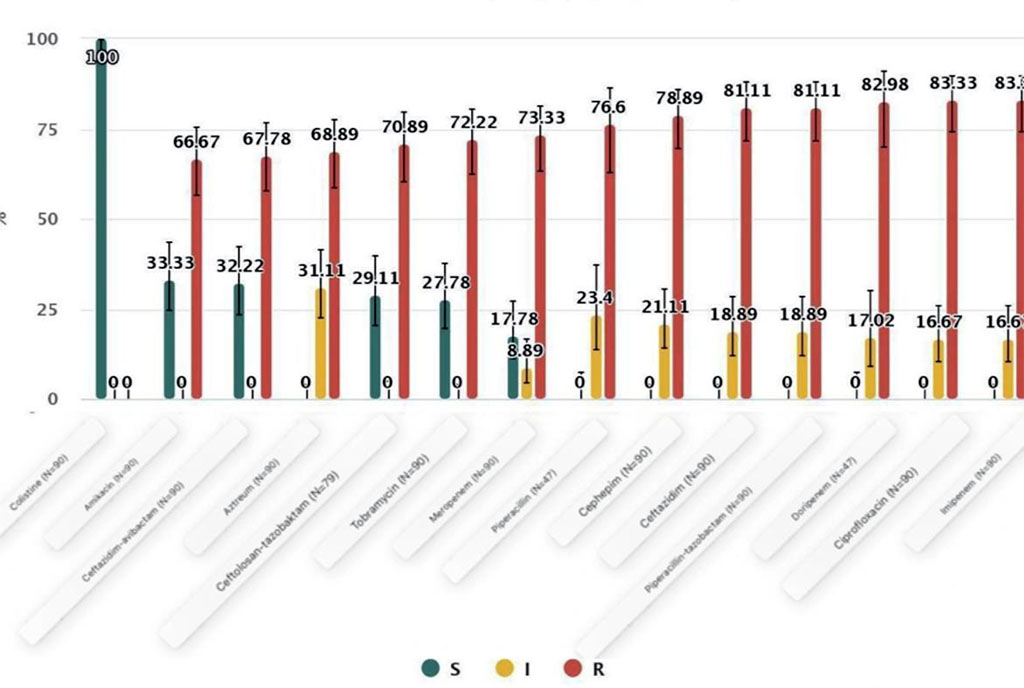
Figure 2: Antibiotics SIR summary of Pseudomonas aeruginosa in the Siberian region
Klebsiella pneumoniae is one of the most important members of the Enterobacteriaceae. It occupies a leading position in the list of the most common nosocomial skin and soft tissue pathogens in the Sibircky federal district. This microorganism is most sensitive to the antibiotic Сolistin (98%). It is most resistant to the antibiotics Ampicillin (98%) and Ciprofloxacin (88%). (Fig. 3).
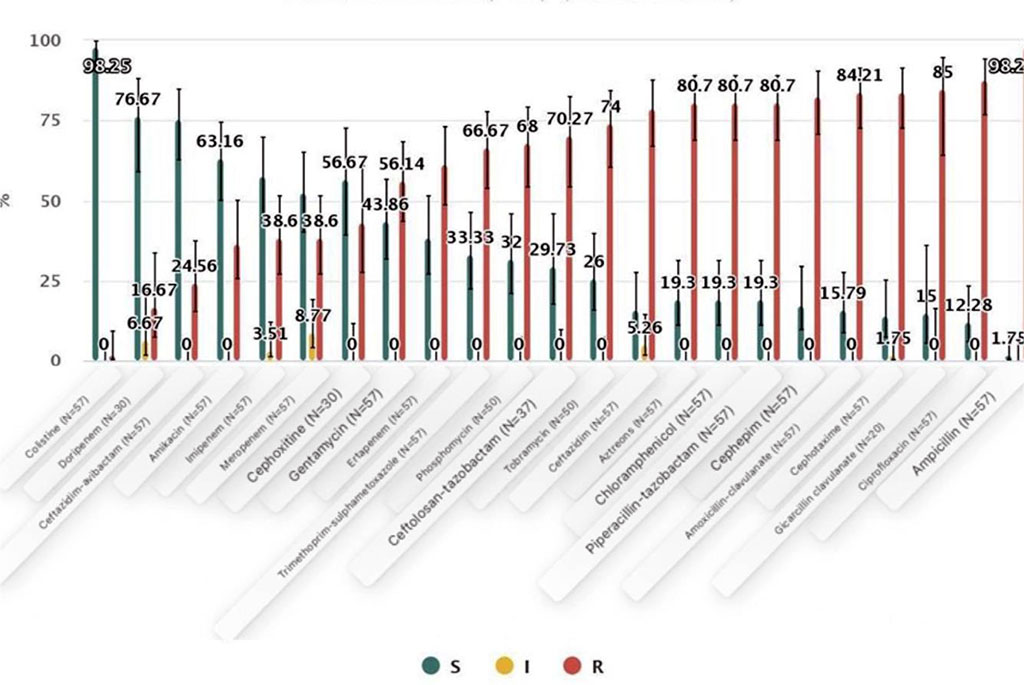
Figure 3: Antibiotics SIR summary of Klebsiella pneumoniae in the Sibircky federal district.
The Far Eastern region includes the following representatives among the three most common nosocomial skin and soft tissue pathogens in surgical patients: Pseudomonas aeruginosa (32%), Klebsiella pneumoniae (20%) and Escherichia coli (11%).
Pseudomonas aeruginosa in this region is significantly more sensitive to the antibiotic Colistin (100%). This microorganism is most resistant to Ciprofloxacin (73.2%) and Tobramycin (70.7%) (Figure 4).
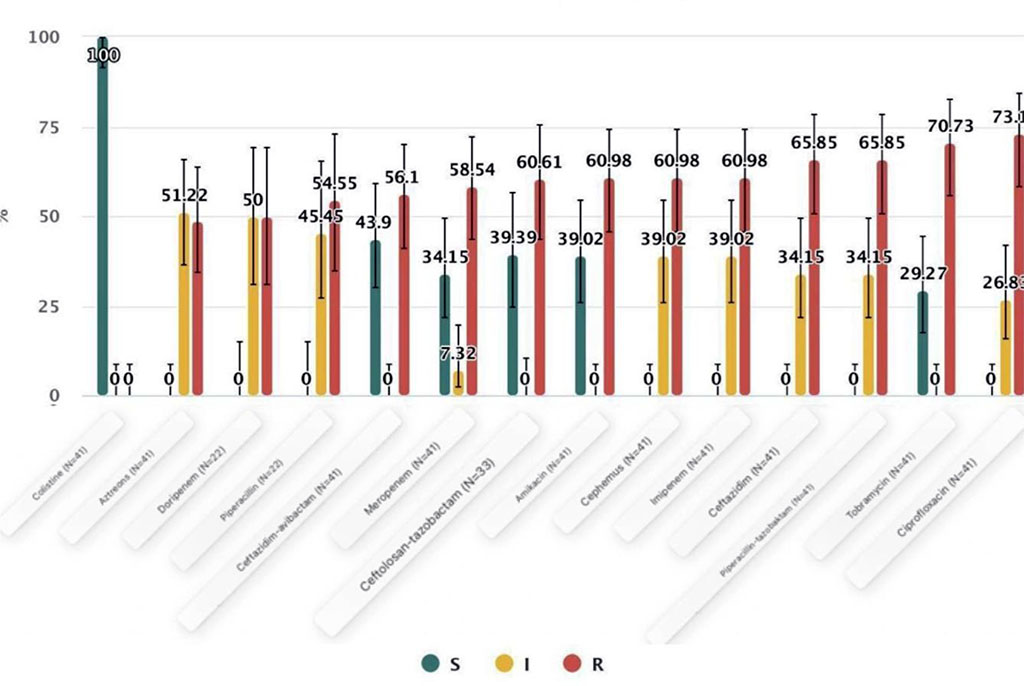
Figure 4: Antibiotics SIR summary of Pseudomonas aeruginosa in the Dalnevostochny federal district.
An analysis of clinical strains shows a high level of resistance to meropenem. It is associated with the presence of two resistance mechanisms (losing the OprD protein and activating the efflux system). One mechanism is sufficient for the manifestation of a high level of resistance to imipenem (loss of the OprD protein).
There is evidence that P. aeruginosa strains can have more than one mechanism of resistance to beta-lactam antibiotics at the same time. For example, depression of the chromosomal β-lactamases can be combined with plasmid production and a decrease in the permeability of the outer membrane.
Klebsiella pneumoniae is most sensitive to the antibiotic Colistin (98 %). The maximum resistance of this micro-organism is to ampicillin (98%) (Fig. 5).
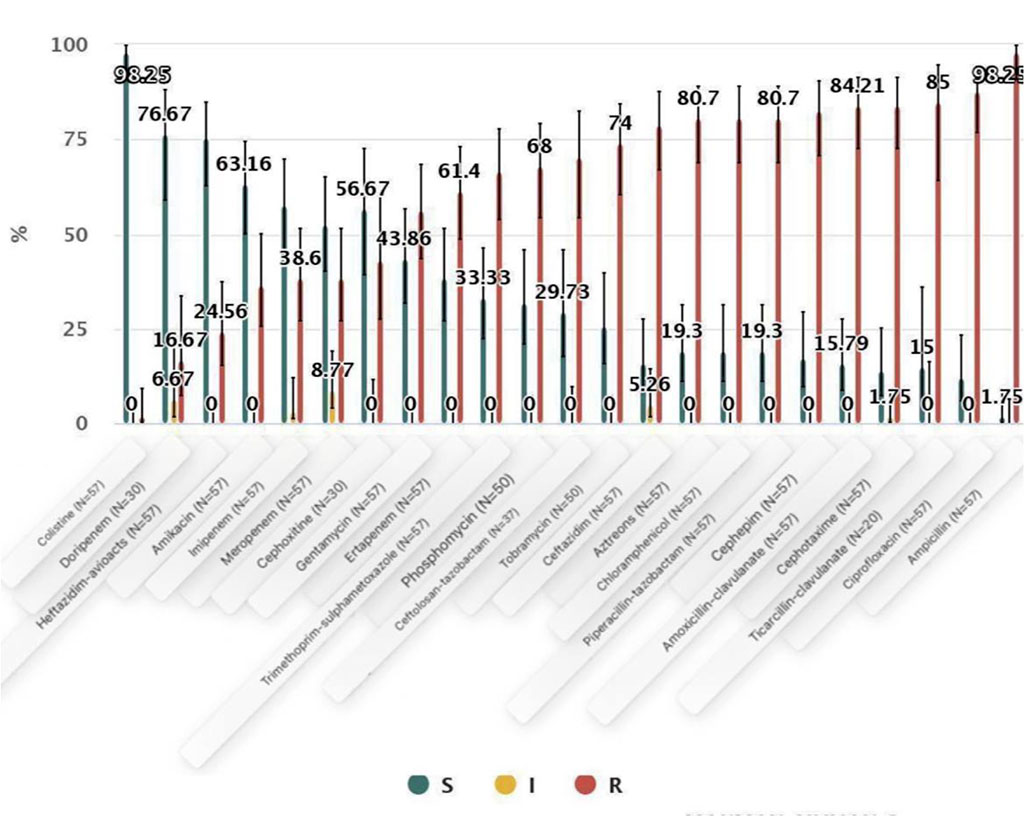
Figure 5: Antibiotics SIR summary of Klebsiella pneumoniae in the Far East region.
K. pneumoniae is the most active colonising organism among the Enterobacteriaceae and is the actual causative agent of nosocomial infections. There has also been an accumulation of chromosomal mutations that code for resistance to the fluoroquinolones. Since 2000, the rapid spread of multi-resistant strains of K. pneumoniae has been observed. These microorganisms are resistant to carbapenems by producing plasmid carbapenemase.
Escherichia coli also has the highest level of resistance to the antibiotic ampicillin. Maximum sensitivity was observed for Colistin (100%) and Tigecycline (97%) (Figure 6).
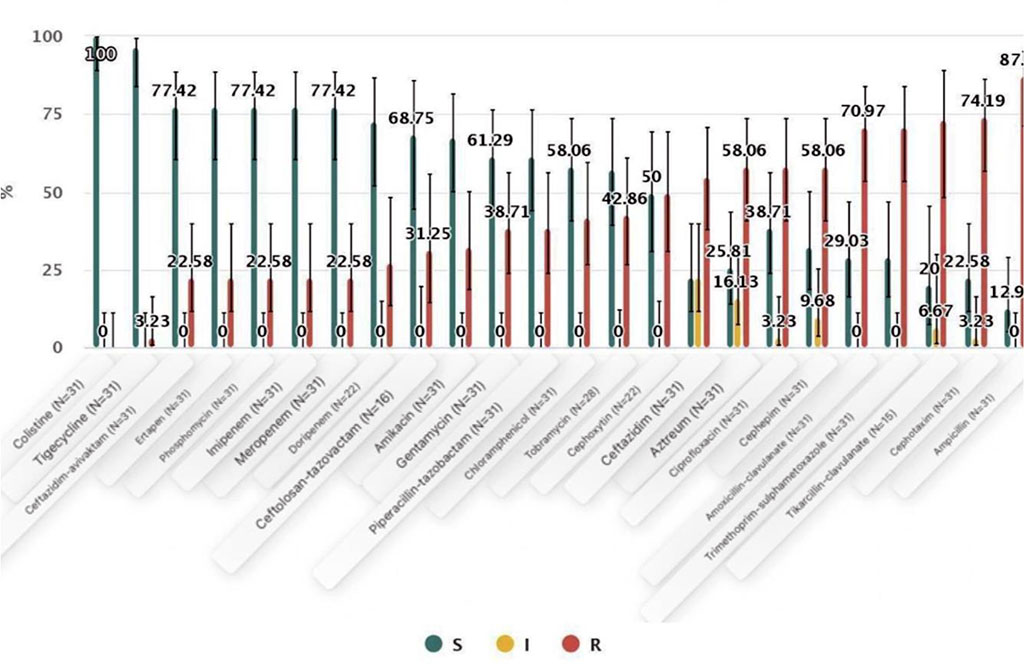
Figure 6: Antibiotics SIR summary of Escherichia coli in the Far Eastern region.
Resistance to antibiotics from different groups is usually associated with these strains. That is why carbapenems are the preferred drugs to treat nosocomial infections caused by these strains. However, the emergence and spread of resistance to carbapenems in Enterobacteriaceae is a major problem at the present time. There is a real need to monitor the susceptibility of nosocomial pathogens.
Antibiotics are one of the most important and powerful medicines that humans have created. They are an active part of every doctor's daily practice.
At the end of February 2017, the WHO published a list of the 12 most antibiotic-resistant 'priority pathogens', divided into three groups (extreme priority, high priority and medium priority) in accordance with the level of need for the development of new antibiotics against them. It should be the benchmark for scientific research in all countries. Some of the antibacterial drugs used in practice begin to lose their effectiveness after only a short time of using them.
Members of the Enterobacteriaceae are most resistant to the antimicrobial drugs Ampicillin (98%) and Ciprofloxacin (88%) in the Siberian region for the period from 2016 to 2020. These microorganisms are most resistant to Ampicillin (98%) in the Far East Region for the same period. Staphylococcus aureus is most resistant to Ciprofloxacin and Erythromycin among all antibiotics used in the Siberian region.
Pseudomonas aeruginosa is most resistant to ciprofloxacin and imipenem in equal proportions (83.4%) and to doripenem (83 %) in the Far Eastern region.
The development of more advanced methods of resistance of microorganisms to drugs in the future may be initiated if there will be no changes in the indications and regimens of antibiotic therapy. It is necessary to improve the qualifications of doctors and other medical personnel, to educate citizens about the need to be sensitive when using antibiotics, to develop individual resistance profiles for each patient, and to create a single database that allows all levels to determine the most effective method of antibiotic therapy.