- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Despite scientific and technological progress and the emergence of modern diagnostic methods, the number of neglected cases of oncopathology has been increasing annually, and its mortality rate has been also increasing. Thus, over the past five years in Russia it increased by 12.4%. Moreover, the one-year mortality of patients with oral mucosa oncological pathology (OMC) is over 50 %, the 5-year survival rate is 24 % for men and 37 % for women. One of the demanded areas of effective medicine is the use of minimally invasive organ-preserving diagnostic tests, which unfortunately have not been widely used in practical dentistry. The purpose of the study is to improve early diagnostic efficiency for detecting pathological processes in the oral mucosa through the combined use of optical and cytological methods for its study. We examined 350 patients of both sexes aged from 20 to 67 years within consultation appointments with the aim of specifying the diagnosis and determining the algorithm of treatment. Methods: clinical, analytical, physical (autofluorescence dentistry), laboratory (liquid cytology), statistical. Conclusion: combined use of methods of autofluorescence stomatoscopy and liquid cytology increases efficiency of diagnostic stage, reduces risk of neglected stages of pathological processes, improves quality of patient's life.
Keywords: cancer screening, early diagnosis, precancer, cancer. Information about authors:
With the upward trend in dental pathology (41% of the world population in 2003, 45% - 2019), which are in front-line positions pathology of the oral mucosa in the structure of dental diseases (ranked third), neglected cases of oral cancer in Russia (64.7%) actualize the problem of cancer screening and oncological alertness [1-5]. Despite visual accessibility during the oral cavity examination and availability of modern diagnostic methods, over 9500 new cases of oral mucosal cancer are registered annually in Russia, and in the Volga Federal District the morbidity rate is second among Russian regions and reaches 550 per 100,000 people [6-8].
The fight against cancer is one of our federal strategic directions, and its tasks are: to reduce the mortality rate due to malignant neoplasms to 185 cases per 100 000 of the population, to introduce cancer screening to diagnose pathological conditions in the early stages of development, and to raise oncological awareness among doctors of all specialties [8-12]. A medical service - autofluorescence stomatoscopy was added into the State Guarantees Program of the compulsory medical insurance system. This enables to expand the coverage of the population with this type of examination and prevention of oncopathology [13-16].
Timely detection of pathological processes of oral mucosa at a risk of malignant transformation, using minimally invasive technologies, as well as minimizing their provoking risk factors, is one of the basic issues of modern dentistry [17-22]. Due to the fact that April is “Head and Neck Cancer Awareness” Month, we raised the issue once again [23-26].
Since cancer screening has high sensitivity (98%), against the background of relative specificity (75%), the issues related to the differential diagnosis of the pathology are still debatable [27-31]. The use of cytological methods at the stages of diagnosis reduces the risk of possible false positive and false negative results, and is the basis for further research for effective diagnostic methods [32-37].
The purpose of the study is to improve early diagnostic efficiency for detecting pathological processes in the oral mucosa through the combined use of optical and cytological methods for its study.
350 male and female patients, aged 20 to 67 years old, who applied for a consultation to clarify their diagnoses and determine the algorithm of treatment, were examined at the Department of Dentistry, Privolzhsky Research Medical University (Nizhny Novgorod, Russia). Due to the fact that one of the components of cancer alertness is the timely detection and prevention of risk factors, we have developed a questionnaire aiming to extract the information about bad habits, episodic contact with hazardous industrial factors as well as smoking (including hookahs, electronic and conventional cigarettes).
Research methods: clinical, analytical, physical (autofluorescence stomatoscopy), laboratory (liquid cytology).
Visualization of the pathological processes of the mucous membrane was performed using the AFS-D system (LLC Polironic, registration certificate No. FSR 2011/10669) with a wavelength of ≈ 400 nm. The method of imaging is based on the principle of different absorption and reflection of light by cellular and stromal fluorophores within epithelial tissues, the number of which depends on structural and metabolic changes. Deficiency of fluorophores causes a lack of energy for a normal luminescence. As a result, the focus of "luminous extinction" is determined in inflammatory processes and the focus of complete loss of luminescence in dysplastic processes is the "dark spot".
Examination of the oral mucosa was carried out following the developed protocol with the topography and coding of the elements of the lesion according to the WHO classification in accordance with the modified scheme-topogram of Roed-Petersen and Renstrup, modified by O. S. Gileva et al., 2008. The elements of the lesion in the area of the red border of the lip were evaluated and registered following the topographic scheme in accordance with the author's method (Gazhva S.I., Dyatel A.V., 2015).
To interpret the results of the obtained optical images using stomatoscopy in a clinical setting, a standardized scale of RAL shades of green has been proposed. It marked the mucous membrane correspondence of fluorescence shades and conditions of the oral mucosa under normal conditions, inflammation, precancer and cancer.
Liquid-based cytology was used to determine the nature of the disease. Being a minimally invasive, organ-preserving method, it allows in vivo morphological diagnosis of cells and non-cellular components in a smear from the material of various organs and tissues taken from the patient. The sampling was carried out at the Department of Dentistry using a Rovers Orcellex brush, followed by immersion in a BD SurePath vial containing an alcohol solution. The vial shelf life of the material is 4 weeks at room temperature and 6 months in the refrigerator. Up to 5 preparations can be made from the residual sample for immunocytochemistry, immunohistochemistry and PCR for the detection of human papillomavirus. This study was carried out as part of a professional cooperation on the basis of LLC "National Center for Clinical Morphological Diagnostics" (St. Petersburg).
During dental examinations of 350 patients of both sexes aged 20 to 67 years, in 200 people there were no clinical manifestations of pathological processes of the oral mucosa (OM), whereas in 150 patients pathological processes were detected. As a result, the obtained optical images of each clinical situation demonstrated that a healthy mucosa, when using the AFS system, comes in various shades of green. Based on the morphological examination, the structure was proven to be dependent on the OM, the severity of the vascular component, the number of cellular and stromal fluorophores (Goryacheva T.P., 2018) (Fig. 1).

Fig.
1a Normal oral mucosa
Fig.
1b Obtained optical images of OM in normal
Among all examined patients presenting no clinical manifestations of pathological processes, 124 patients had some oral mucosal changes at the preclinical level. To establish the nature of the pathological process, liquid-based cytology was performed for each case. Based on the analysis of the results obtained, we can assume that the initial pathology originates inside the epithelium, starting mainly with inflammatory processes, followed by the addition of parakeratosis and hyperkeratosis (Table 1).
Table 1 Prevalence of pathological processes at the preclinical level
| М / % of the total number of examined patients | F / % of the total number of examined patients | |
| Reactive (inflammatory) changes | 48 | 32 |
| 24% | 16% | |
| Parakeratosis | 16 | 9 |
| 8% | 4,5% | |
| Hyperkeratosis | 12 | 7 |
| 6% | 3,5% |
So, during the initial clinical examination, the oral mucosa had no visible pathological processes. But when using autofluorescence stomatoscopy, foci of quenching fluorescence were determined in inflammatory changes, and light green fluorescence in hyperkeratosis (Fig. 2). In the results of liquid cytology, reactive changes and parakeratosis of the surface layers of the epithelium were determined.

Fig.
2a The mucous membrane of the mouth without visible pathological
changes
Fig
2b Visualization of the pathological process at the preclinical level
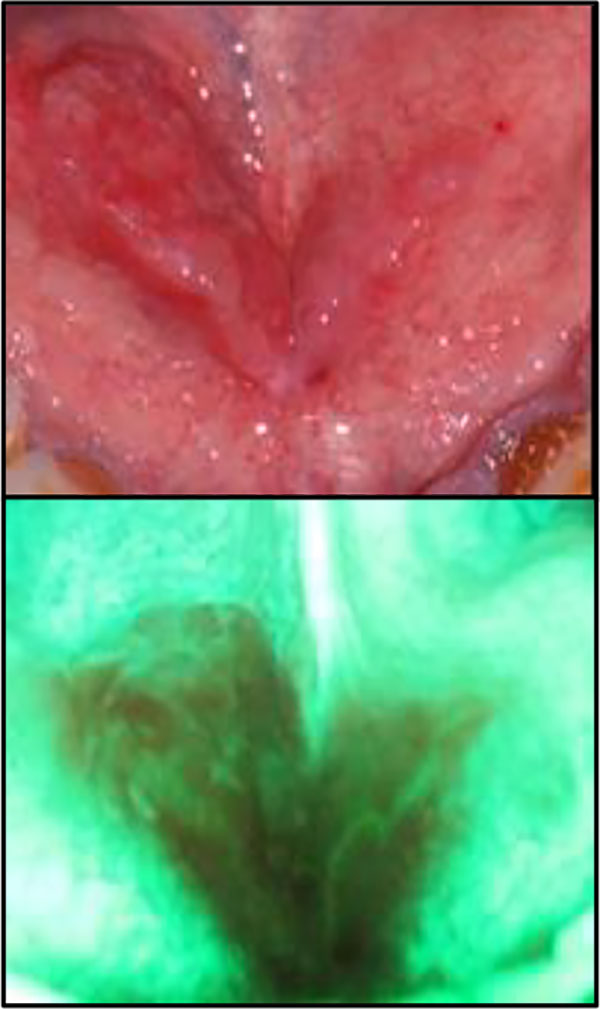
Among the patients presenting pathological processes of the OM, 54 had hyperkeratosis, 93 had inflammatory changes, and 3 had neoplasms of the OM. The optical image of hyperkeratosis is characterized by a lesion on the unchanged OM, with clear boundaries, and a predominance of light green luminescence against the background of normal luminescence of the healthy mucosa (Fig. 3). The more pronounced the phenomena of hyperkeratosis, the brighter the fluorescence of the lesion. According to the results of cytology, there are phenomena of hyperkeratosis and parakeratosis of the superficial and medial layers without atypism.

Fig
3a The phenomena of OM hyperkeratosis
Fig
3b Optical image of hyperkeratosis with APS
In inflammatory diseases, the optical image is characterized by a lesion with clear boundaries in the form of a quenching fluorescence, against the background of an unchanged oral mucosa (Fig. 4). At the same time, the boundaries of the lesion focus during stomatoscopy significantly prevail over the clinically presentable boundaries of the pathological processes. As a result of liquid cytology, parakeratosis, reactive and inflammatory phenomena of the intermediate and deep layers without atypism are determined.
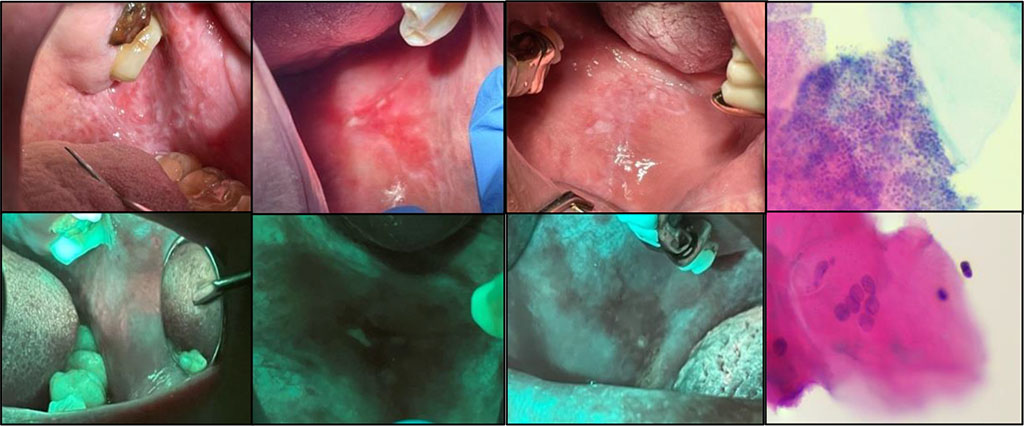
Fig
4a Inflammatory processes of the oral mucosa
Fig
4b Optical image of inflammatory changes
The optical image of oncological diseases is characterized by a complete loss of luminescence - a “dark spot” against the background of the unchanged OM, showing clear boundaries (Fig. 5). In addition, there were some cases presenting no clinical manifestations in the oral cavity (Fig. 6). However, in some cases, the boundaries of the lesion significantly prevailed over the clinical boundaries of the pathological process.
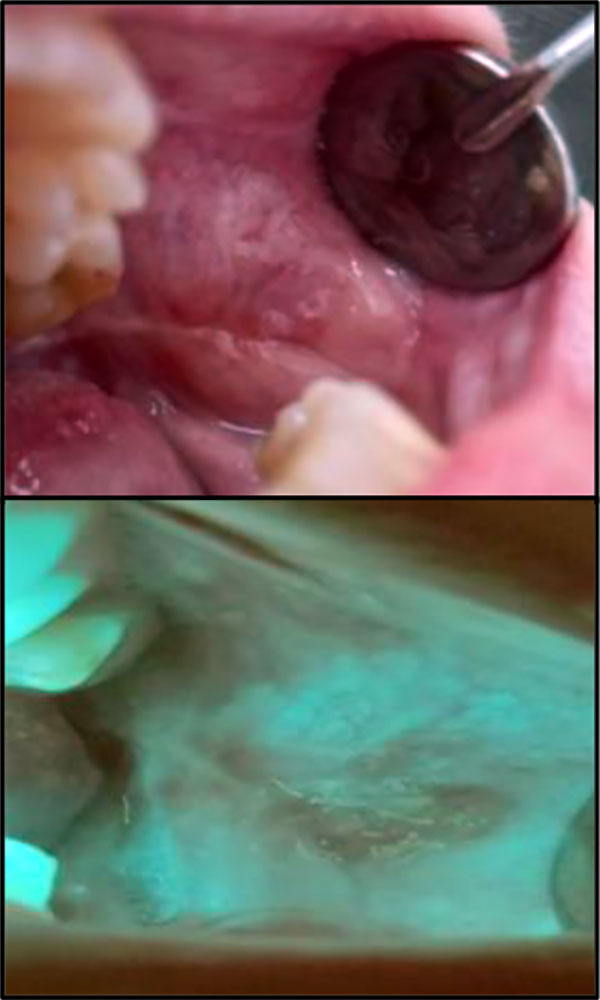
Fig
5a Buccal mucosa malignant neoplasm of the left cheek
Fig
5b Optical image of oncology
Fig
6a Oncology of the floor of the mouth
Fig
6b Optical image of oncology
As a result of the examination, it was determined that one of the most frequent localizations of pathological processes is the mucous membrane of the cheeks (26%), the tongue (20%), and the vestibule of the oral cavity (18%) (Fig 7).
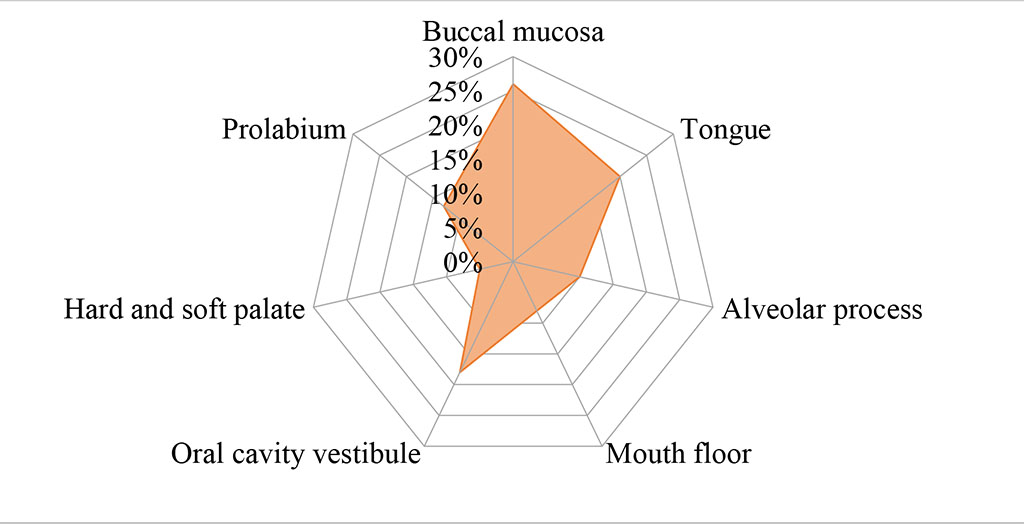
Fig. 7 Localization of pathological processes
Among all those examined with diseases of the oral mucosa, oral lichen planus ranked 1st at 48.6%, leukoplakia ranked 2nd at 32%, trauma ranked 3rd at 7.3%, aphthous stomatitis ranked 4th at 6%, cheilitis ranked 5th at 4%, and oncopathology was the 6th rank at 2 % (Fig. 8). The prevalence of inflammatory processes at the preclinical level was also determined. (Fig. 9).
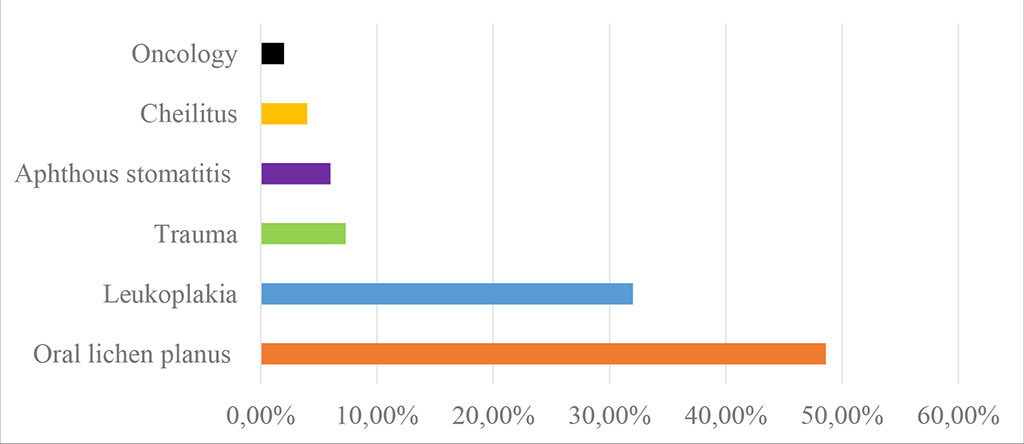
Fig. 8 Diagram of prevalence of OM diseases
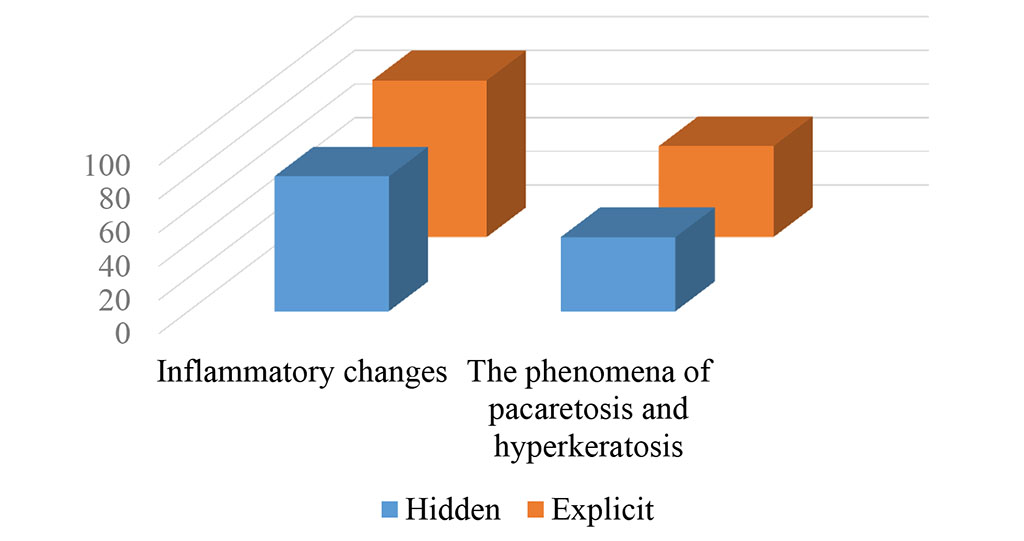
Fig 9 Diagram of hidden and overt pathological processes
As a result of the study, more than 75% of the diagnoses made on the basis of the use of stomatoscopy were confirmed by the results of liquid cytology, further cementing the high diagnostic value of stomatoscopy as a method of diagnosing pathological processes (Fig. 10).
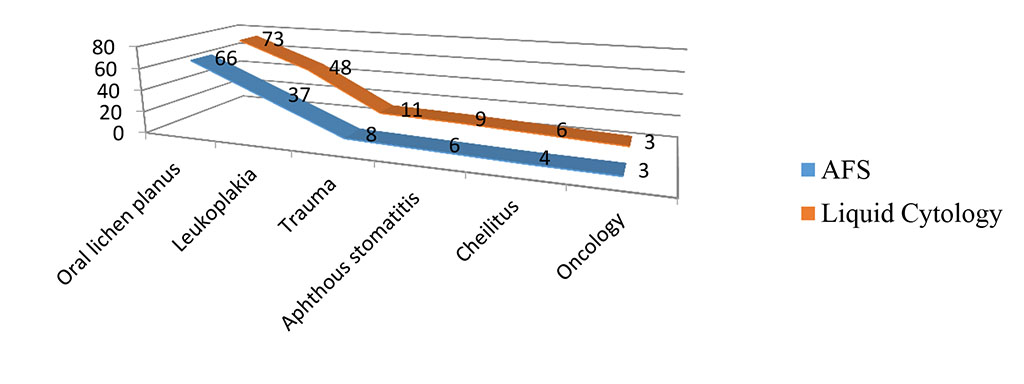
Fig. 10 Confirmed clinical diagnoses
The analysis of the results obtained at the preclinical stage of the examination allows us to hypothesize that the pathological process initially starts intraepithelially, with inflammatory manifestations. Later, in the presence of persistent predictors, it transforms into other inflammatory-destructive processes, which manifest on the oral mucosa in the form of a visualizable pathological focus. This is confirmed by pathological processes of lichenoid nature, which dominate in the structure of oral pathology. As the method of autofluorescence stomatoscopy has a high sensitivity and relative specificity, not allowing to determine the morphology of the pathological process, it is necessary to use liquid cytology to reduce the risk of false-positive and false-negative results at advanced stages of pathological processes in the OM. It has been established that the places of the most common localization of pathological processes of the OM are the buccal mucous (26%), the tongue (20%), the vestibule of the oral cavity (18%), that should be taken into account during a dental examination.