- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 1. DOI 10.35630/2025/15/1.104
Aims: To analyze potential influences of primary arterial hypertension in patients with an inguinal hernia after Liechtenstein open inguinal hernia repair by using different types of surgical mesh implants.
Method: 40 patients with inguinal hernia were operated by the Lichtenstein repair using different types of mesh implants during the period between January 2022 and the end of December 2024. The patients were splitted into 2 equal groups (no=20); Group A (Normotensive Patients) and Group B (Hypertensive Patients),and the results were analyzed using machine learning Artificial Intelligence programming language; Python.
Results: Duration of herniation, total hospitalization stays, time of operation and the incidence of postoperative complications — the results of the t-tests show no statistically significant differences among both groups.
Conclusions: In our study, we found that hypertension status does not significantly impacts upon the outcomes of inguinal hernia repair.
Keywords: Artificial intelligence; Hernia; Hypertriton; Lichtenstein; Surgical mesh.
The international guidelines for inguinal hernioplasty still consider the Liechtenstein technique as the reference standard [1] among more than 300 available repair methods [2] for inguinal hernia, which account for about 10-15% of the globally operated surgical procedures annually [3]. The pathogenesis of abdominal wall hernia and its recurrence is complex and multifactorial [4], being commoner among patients with connective tissue disorders and abdominal aortic aneurysms. This is evidenced by the thinning and disturbance of collagen fibres of rectus sheath in inguinal hernia patients in comparison to normal population. Even more, direct inguinal hernias possess thinner diameter of collagen fibres in the rectus sheath and a higher amount of interfibrillar matrix of fascia transversalis, in comparison to oblique hernias. Subserosal fibrosis are present in both types and may be attributed to the hernia itself, rather than the cause [5].
Patients with varicocele have a potential high risk of developing chronic venous disease and inguinal hernias over time, demonstrating a strong pathogenic link among three conditions, where an imbalance of the extracellular matrix (ECM), in the form of elevated levels of matrix metalloproteinases (MMP), particularly MMP-9, is found in these three conditions [6]. Furthermore, MMP-2 levels are elevated in patients with direct inguinal hernia, MMP-1 is associated with incisional and recurrent inguinal hernias which are also associated with elevated levels MMP-13 expression [7].
Other evidence of the ultimate relation between the coexistence of vascular disease and inguinal hernia is that vascular system consists of specialized cells surrounded by a dynamic ECM that not only provides structure through connections of cells within the network, but also instructs cellular function by facilitating the absorption of growth factors by the cells of the vascular system, which becomes dysregulated upon disease [8].The relation between abdominal aortic aneurysm (AAA) and abdominal hernias do exists, but doesn’t involve the size or even the rupture of the AAA, denning the relation between hernia and the aggressiveness of the AAA [9]. Even more, the prevalence of inguinal hernia is higher among patients with thoracic aortic diseases [10]. This fact makes us consider screening of aortic aneurysm in geriatric patients with inguinal hernia [11].
Using Artificial intelligence programs in hernia surgery e.g., Python [12] improved computer-vision methodology from supervised learning and machine learning algorithms in detecting wounds after inguinal hernia surgery, recognition of vas deferens during laparoscopic inguinal hernia surgery more accurately as well as the development of a laparoscopic training system for offering online training to surgeons [13]. Beside the development of an automated phase-recognition system for identifying surgical phases in Transabdominal Preperitoneal (TAPP) procedures, and a computerized vision algorithm designed to recognize surgical steps in videos of totally extraperitoneal (TEP) inguinal hernia repair automatically [14]. In addition, Applying Artificial intelligence in abdominal hernia surgery had led to sustainable healthcare for abdominal hernia patients as it enhances the development of computer analytics improving patient outcomes [15].
Our study was carried on 40 patients diagnosed with inguinal hernias and operated by the Liechtenstein using different types of surgical mesh implants in the clinical hospital no. 85 FMBA, Moscow, Russia.
Inclusion criteria:
Exclusion criteria:
Our study group was splited into 2 equally divided subgroup;
In Group A- patients (No=20) normotensive patients. Average age was 51.45 years. This groups contains 20 male patients; 16 patients with right inguinal hernia and 4 with left inguinal hernia. The ratio of oblique to direct inguinal hernia 12:8. In this group we used 8 PolypropyleneTM, 6 PartieneTM, 5 ProgripTM and 1 Bard 3D MaxTM mesh implants (Table 1).
While in Group B- patients (N0=20) hypertensive patients. Average age was 55.95 years. This groups contains 18 male patients and 2 female patients; 10 patients with right inguinal hernia and 10 with left inguinal hernia. The ratio of oblique to direct inguinal hernia 10:10. In this group we used 14 PolypropyleneTM and 6 PartieneTM (Table 2).
Table 1. The demographics of group A (Normotensive Patients)
| Metric | Mean | Standard Error | Median | Mode | Standard deviation | Range | Minimum | Maximum |
| Age (years) | 51.45 | 3.03 | 53 | 70 | 13.56 | 43 | 27 | 70 |
| Duration of Herniation (months) | 24.75 | 8.58 | 7.5 | 6 | 38.39 | 117 | 3 | 120 |
| Hernia Length (cm) | 6.9 | 0.61 | 6 | 6 | 2.71 | 9 | 3 | 12 |
| Hernia Width (cm) | 4.68 | 0.28 | 4.5 | 4 | 1.26 | 4.5 | 2.5 | 7 |
| Hernia Height (cm) | 3.75 | 0.45 | 3.5 | 3 | 1.28 | 4 | 2 | 6 |
| Hernia Volume (cm³) | 85.35 | 21.11 | 39 | 12 | 94.41 | 276 | 12 | 288 |
| External Inguinal Ring Size (cm) | 2.5 | 0.11 | 2.5 | 2.5 | 0.51 | 2 | 1.5 | 3.5 |
Table 2. The demographics of group B (Hypertensive Patients)
| Metric | Mean | Standard Error | Median | Mode | Standard deviation | Range | Minimum | Maximum |
| Age (years) | 55.95 | 2.96 | 63 | 64 | 13.26 | 41 | 27 | 68 |
| Duration of Hernia (month) | 22.7 | 4.41 | 18 | 24 | 19.70 | 58 | 2 | 60 |
| Hernia Length (cm) | 7.35 | 0.88 | 6 | 5 | 3.95 | 13 | 2 | 15 |
| Hernia Width (cm) | 4.7 | 0.33 | 4.5 | 4 | 1.49 | 5 | 2 | 7 |
| Hernia Height (cm) | 3.29 | 0.61 | 3 | 2 | 1.60 | 4 | 2 | 6 |
| Hernia Volume (cm³) | 86.3 | 28.05 | 31 | 25 | 125.46 | 498 | 6 | 504 |
| External Inguinal Ring Size (cm) | 2.35 | 0.19 | 2.5 | 1.5 | 0.83 | 2.5 | 1.5 | 4 |
The statistical data was analyzed by using machine learning Artificial Intelligence programming language; Python. The analysis included the following data:
Right-sided hernias are more common in Group A (61.54%), while left-sided hernias are predominant in Group B (71.43%). Direct hernias show a slightly higher prevalence in Group B (55.56%), whereas oblique hernias are more frequent in Group A (54.55%) [Table 3].
Table 3. The distribution of hernia site (Right: left) and hernia types (Direct: Oblique) among both study groups
| Metric | Group A (Normotensive) | Group B (Hypertensive) | Grand Total | Group A (%) | Group B (%) |
| Sum of Hernia Site (Right) | 16 | 10 | 26 | 61.54% | 38.46% |
| Sum of Hernia Site (Left) | 4 | 10 | 14 | 28.57% | 71.43% |
| Sum of Hernia Type (Direct) | 8 | 10 | 18 | 44.44% | 55.56% |
| Sum of Hernia Type (Oblique) | 12 | 10 | 22 | 54.55% | 45.45% |
The average age was higher in Group B versus Group A (55.95 vs. 51.45 years) (Figure 1), with a slightly shorter herniation duration (22.7 vs. 24.75 months) (Figure 2).
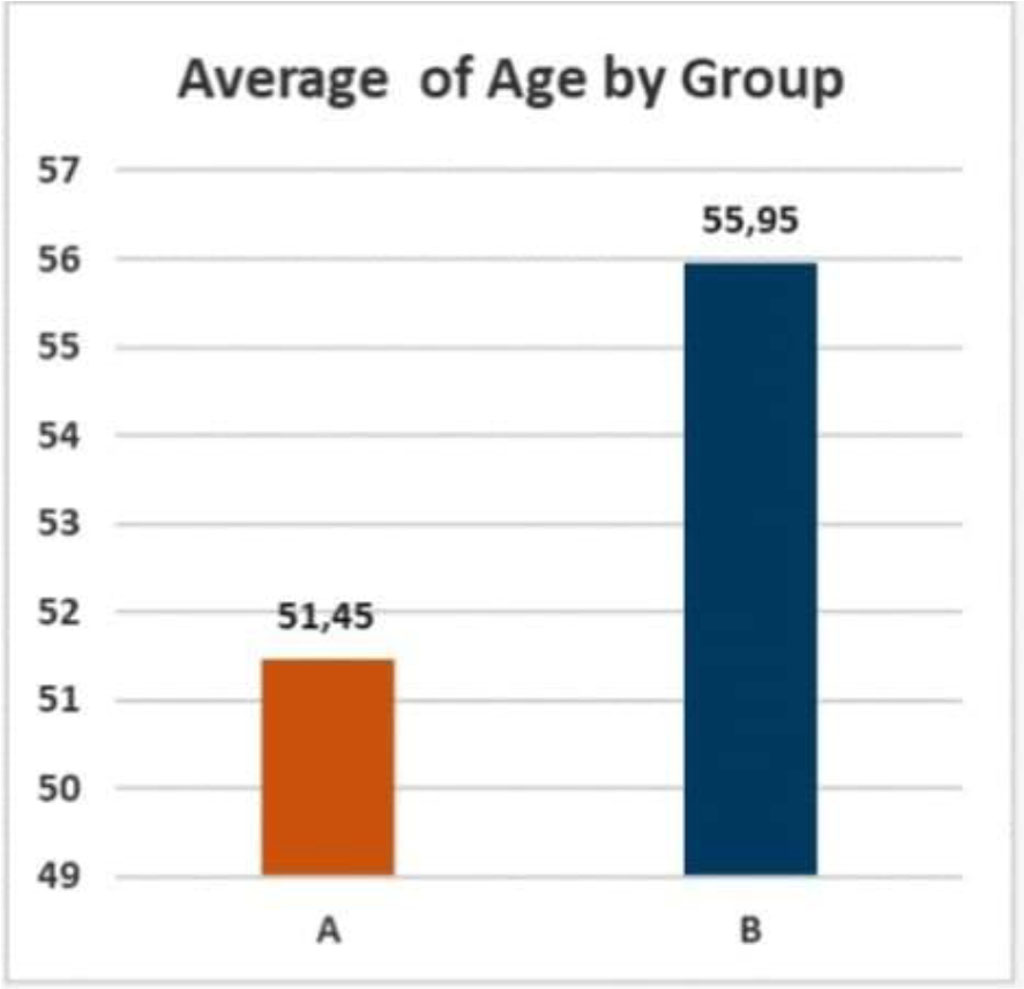
Figure 1. Average age in both groups
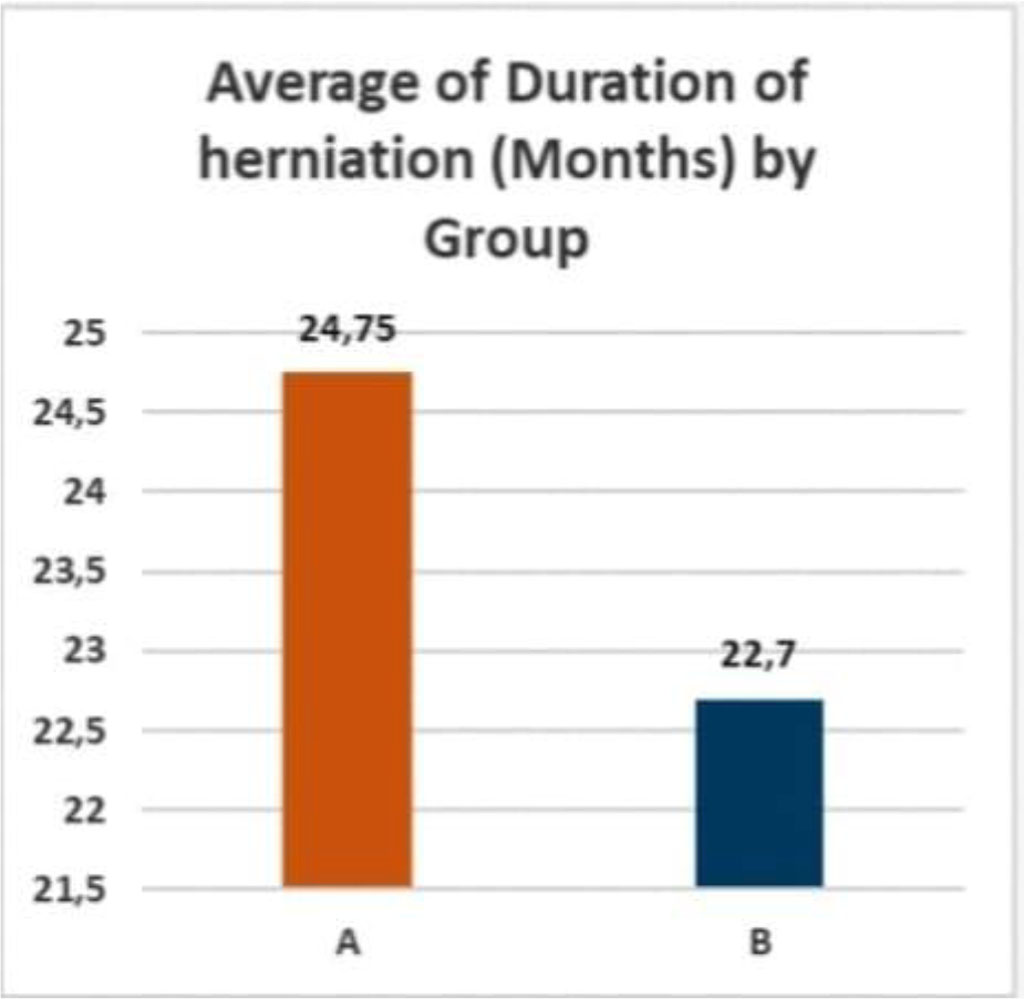
Figure 2. Average duration of herniation in both groups
Preoperative abdominal ultrasonographic examination was done for detecting the size of the external inguinal ring and the dimensions of the hernial sacs in both groups (Table 4).
Table 4. Average dimensions of the external inguinal ring and hernial sacs
| Metric | Group A (Normotensive) | Group B (Hypertensive) | Grand Total |
| Average External Inguinal Ring Size (cm) | 2.5 | 2.35 | 2.43 |
| Average Length of Hernial Sac (cm) | 6.75 | 7.6 | 7.18 |
| Average Width of Hernial Sac (cm) | 3.9 | 4.63 | 4.26 |
| Average Height of Hernial Sac (cm) | 3.0 | 3.19 | 3.10 |
| Average Volume of Hernial Sac (cm³) | 99.93 | 135.1 | 117.51 |
In group B (hypertensive patients), we found 13 (65%) patients with associated comorbidities other than arterial hypertension (8 (40%) patients with cardiovascular diseases, 3(15%) with gastrointestinal diseases and 2(10%) patients with metabolic diseases) [Table 5].
Table 5. Associated comorbidities in group B patients
| Associated disease | Incidence |
| Congestive heart failure | 5/20 (25%) |
| Coronary heart disease | 2/20 (10%) |
| Chronic gastritis | 2/20 (10%) |
| Chronic cholecystitis | 1/20 (5%) |
| Varicocele | 1/20 (5%) |
| Type II diabetes mellitus | 1/20 (5%) |
| Dyslipidemia | 1/20 (5%) |
| Grand total | 13/20 (65%) |
Type of anesthesia
Spinal anesthesia is the most used technique in both groups, slightly higher in Group B (52.63%). Endotracheal anesthesia is uniquely applied in Group A patients (100%) (Table 6).
Table 6. Types of used anathesia in both groups
| Anesthestic route | Group A (Normotensive) | Group B (Hypertensive) | Grand Total | Group A (%) | Group B (%) |
| Spinal | 18 | 20 | 38 | 47.37% | 52.63% |
| Endotracheal | 2 | 0 | 2 | 100.00% | 0.00% |
Types of used mesh implants
For group A- we used 8 PolypropyleneTM, 6 PartieneTM, 5 ProgripTM and 1 Bard 3D MaxTM mesh implants, while in group B- patients (N0=20) hypertensive patients. Average age was 55.95 years. This groups included 18 man and 2 women; 10 patients with right inguinal hernia and 10 with left inguinal hernia. The ratio of oblique to direct inguinal hernia 10:10. In this group we used 14 PolypropyleneTM and 6 PartieneTM (Table 7). Mesh dimensions are mentioned (Table 8).
Table 7. Types and distribution of surgical mesh implants in both groups
| Mesh type | Group A (Normotensive) | Group B (Hypertensive) | Grand Total | Group A (%) | Group B (%) |
| PolypropyleneTM | 8 | 14 | 22 | 36.36% | 63.64% |
| ParieteneTM | 6 | 6 | 12 | 50.00% | 50.00% |
| ProgripTM | 5 | 0 | 5 | 100.00% | 0.00% |
| Bard 3D MaxTM | 1 | 0 | 1 | 100.00% | 0.00% |
Table 8. Average dimensions of the used mesh implants in both groups
| Average Mesh Length (cm) | Average Mesh Width (cm) | Average Mesh Area (cm²) | |
| Group A (Normotensive) | 8.95 | 10.8 | 96.3 |
| Group B (Hypertensive) | 7.35 | 11.6 | 89.85 |
| Grand Total | 8.15 | 11.2 | 93.08 |
Polypropylene mesh is more commonly used in Group B (63.64%), while Progrip and Bard 3D Max meshes are exclusively used in Group A.
The average operative time was in group A (normotensive patients), only 5 minutes less than that of group B (hypertensive patients) (Table 9) (Figure 3).
Table 9 Average operative time (in minutes) for both groups
| Group A (Normotensive) | Group B (Hypertensive) | Grand Total |
| 44.5 | 50.25 | 47.375 |
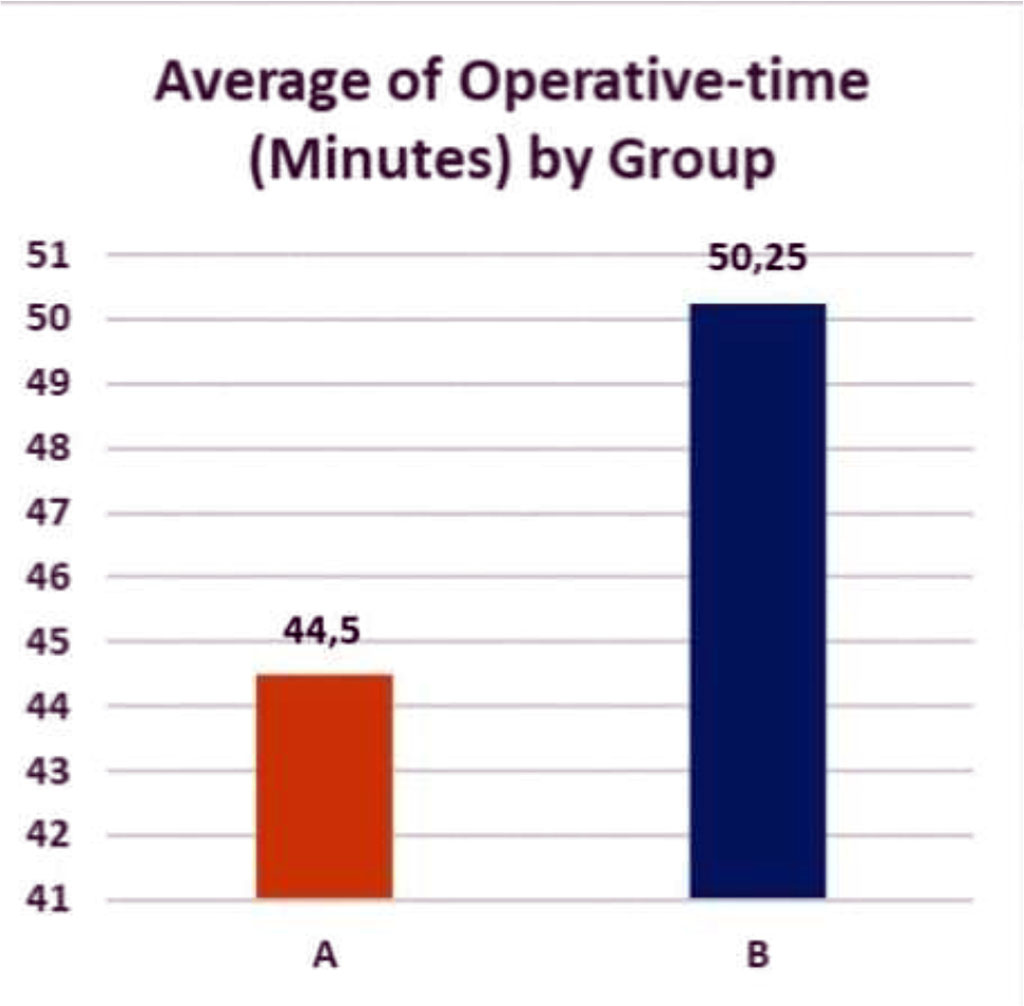
Figure 3. Average operative time in both groups
The average duration of hospitalization shows no significant differences among both groups; 4.9 days for group A (normotensive patients) versus 4.95 days for group B (hypertensive patients) (Table 10) (Figure 4).
Table 10. Average duration of total hospitalization (beds/day)
| Group A (Normotensive) | Group B (Hypertensive) | Grand Total |
| 4.9 | 4.95 | 4.925 |
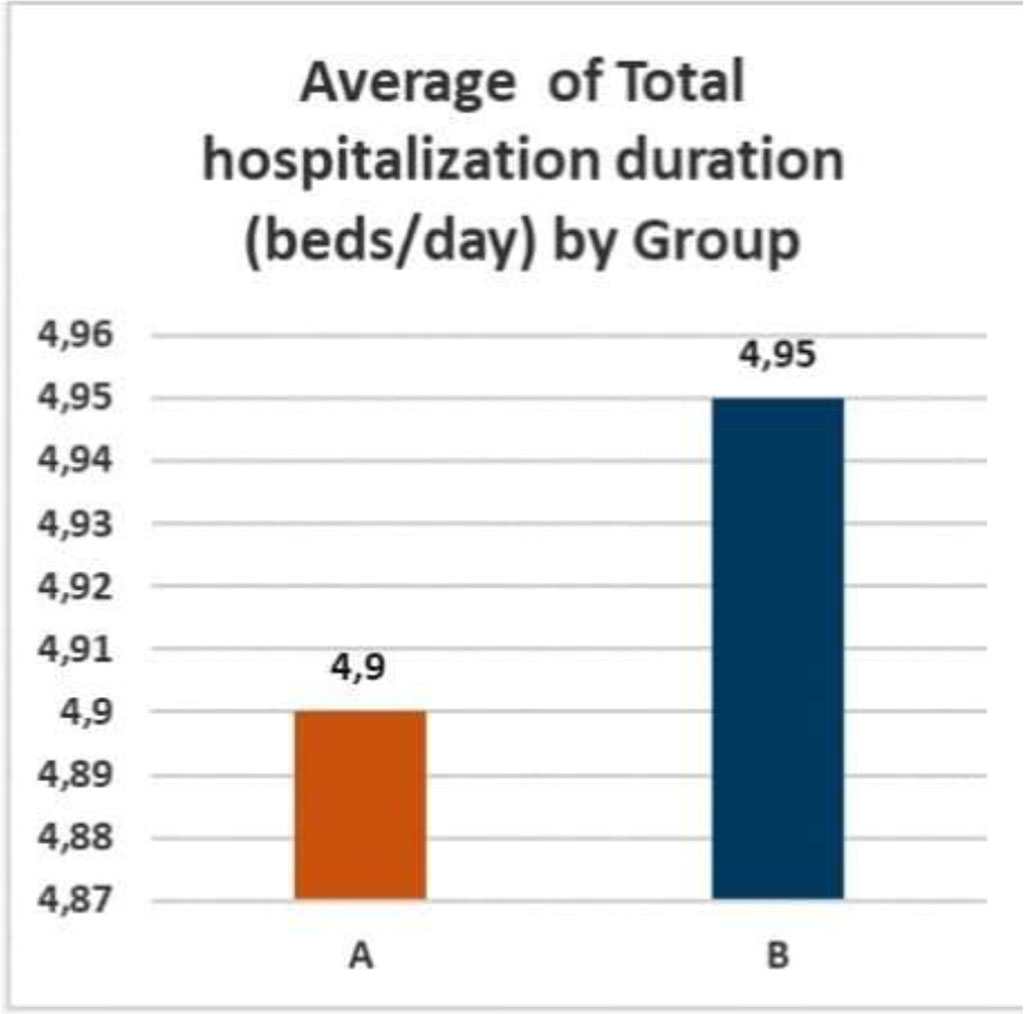
Figure 4. Average duration of total hospitalization (beds/day).
The incidence of complications during the post-operative period included;
In group A; 2 patients had post-operative pain which was relieved by using NSAIDs.
For group B; 4 patients had post-operative pain which was relieved by using NSAIDs and 1 patient had foreign body sensation (Table 11).
Table 11. Post-operative complications in both groups.
| Group A | Group B | |
| Post-operative pain | 2/20 (10%) | 4/20 (20%) |
| Foreign body sensation | 0/20 (0%) | 1/20 (5%) |
In group A- No complications.
In group B- No complications.
Not a single case of hernia recurrence had been recorded among both groups.
In an attempt to understand the possible effects of arterial hypertension upon the consequences of open anterior inguinal hernia repair, we correlated the following parameters; Duration of hernaition, hernia Characteristics site, mesh dimensions, operative-time and hospitalization stays (Table 12).
Table 12: Comparison of Hernia Characteristics, Surgical Parameters, and Hospitalization Data by Hernia Site (Right/Left)
| Metric | Group A (Left) | Group A (Right) | Group B (Left) | Group B (Right) | Grand Total (Left) | Grand Total (Right) |
| Average of Total Hospitalization (beds/day) | 4.25 | 5.06 | 5.1 | 4.8 | 4.86 | 4.93 |
| Average of Duration of Herniation (Months) | 28.25 | 23.88 | 17.4 | 28.0 | 20.5 | 25.46 |
| Average of Hernia Length (cm) | 6.5 | 7.0 | 7.1 | 7.6 | 6.93 | 7.23 |
| Average of Hernia Width (cm) | 4.25 | 4.78 | 4.5 | 4.9 | 4.43 | 4.83 |
| Average of Hernia Height (cm) | 3.67 | 3.8 | 2.33 | 4.0 | 3.0 | 3.89 |
| Average of Hernia Volume (cm³) | 97.25 | 82.38 | 45.8 | 126.8 | 60.5 | 99.46 |
| Average of External Inguinal Ring Size (cm) | 2.25 | 2.56 | 2.2 | 2.5 | 2.21 | 2.54 |
| Average of Mesh Length (cm) | 8.0 | 9.19 | 7.8 | 6.9 | 7.86 | 8.31 |
| Average of Mesh Width (cm) | 11.25 | 10.69 | 11.8 | 11.4 | 11.64 | 10.96 |
| Average of Mesh Area (cm²) | 87.0 | 98.63 | 97.8 | 81.9 | 94.71 | 92.19 |
| Average of Length of Hernial Sac (cm) | 4.75 | 7.25 | 7.0 | 8.2 | 6.36 | 7.62 |
| Average of Width of Hernial Sac (cm) | 3.25 | 4.06 | 4.7 | 4.55 | 4.29 | 4.25 |
| Average of Height of Hernial Sac (cm) | 2.5 | 3.18 | 2.88 | 3.5 | 2.75 | 3.32 |
| Average of Volume of Hernial Sac (cm³) | 46.5 | 113.28 | 135.4 | 134.8 | 110.0 | 121.56 |
| Average of Operative Time (Minutes) | 37.5 | 46.25 | 50.0 | 50.5 | 46.43 | 47.88 |
By comparing hernia metrics based on hernia site (Left = 0, Right = 1) across Group A (Normotensive) and Group B (Hypertensive), we found that:
These data may indicate notable differences in metrics between right and left hernias, with right-sided hernias having longer duration of herniation, showing larger dimensions and longer operative times overall.
In attempt to understand if the type of inguinal hernia (Direct: Oblique) could influence the outcomes of hernioplasty, we conducted the following comparison (Table 13).
Table 13: Comparison of Hernia Characteristics, Surgical Parameters, and Hospitalization Data by Hernia Type (Direct/Oblique).
| Metric | Group A (Oblique) | Group A (Direct) | Group B (Oblique) | Group B (Direct) | Grand Total (Oblique) | Grand Total (Direct) |
| Average Total Hospitalization (beds/day) | 4.42 | 5.63 | 5.4 | 4.5 | 4.86 | 5.0 |
| Average Duration of Herniation (Months) | 26.92 | 21.5 | 28.5 | 16.9 | 27.64 | 18.94 |
| Average Hernia Length (cm) | 6.83 | 7.0 | 8.4 | 6.3 | 7.55 | 6.61 |
| Average Hernia Width (cm) | 4.46 | 5.0 | 4.8 | 4.6 | 4.61 | 4.78 |
| Average Hernia Height (cm) | 3.5 | 4.5 | 2.5 | 4.33 | 3.1 | 4.4 |
| Average Hernia Volume (cm³) | 84.17 | 87.13 | 70.7 | 101.9 | 78.05 | 95.33 |
| Average External Inguinal Ring Size (cm) | 2.46 | 2.56 | 2.4 | 2.3 | 2.43 | 2.42 |
| Average Mesh Length (cm) | 9.42 | 8.25 | 8.7 | 6.0 | 9.09 | 7.0 |
| Average Mesh Width (cm) | 10.42 | 11.38 | 12.2 | 11.0 | 11.23 | 11.17 |
| Average Mesh Area (cm²) | 96.25 | 96.38 | 113.7 | 66.0 | 104.18 | 79.5 |
| Average Length of Hernial Sac (cm) | 6.83 | 6.63 | 9.3 | 5.9 | 7.95 | 6.22 |
| Average Width of Hernial Sac (cm) | 3.25 | 4.88 | 4.9 | 4.35 | 4.0 | 4.58 |
| Average Height of Hernial Sac (cm) | 2.75 | 4.0 | 3.11 | 3.29 | 2.9 | 3.5 |
| Average Volume of Hernial Sac (cm³) | 64.63 | 152.88 | 179.8 | 90.4 | 116.98 | 118.17 |
| Average Operative Time (Minutes) | 42.92 | 46.88 | 57.0 | 43.5 | 49.32 | 45.0 |
By comparing between Oblique (Type = 0) and Direct (Type = 1) hernias across Groups A (Normotensive) and B (Hypertensive) we found:
These data may indicate notable differences in metrics between oblique and direct inguinal hernias, where oblique inguinal hernias having longer duration of herniation, while direct inguinal hernias were found to attain larger volumes in hypertensive patients.
These findings could suggest differences in surgical and hernia metrics depending on inguinal hernia site and type.
Analyzing the correlation between type of anathesia and other metrics during open anterior inguinal hernia repair we found: [Table 14].
Table 14: Comparison of Metrics Based on Type of Anaesthesia (Spinal = 1, Endotracheal = 0)
| Metric | Group A (Endotracheal) | Group A (Spinal) | Group B (Spinal) | Grand Total (Endotracheal) | Grand Total (Spinal) |
| Average Total Hospitalization (beds/day) | 5.00 | 4.89 | 4.95 | 5.00 | 4.92 |
| Average Duration of Herniation (Months) | 63.00 | 20.50 | 22.70 | 63.00 | 21.66 |
| Average Hernia Length (cm) | 10.50 | 6.50 | 7.35 | 10.50 | 6.95 |
| Average Hernia Width (cm) | 6.00 | 4.53 | 4.70 | 6.00 | 4.62 |
| Average Hernia Height (cm) | 3.50 | 3.83 | 3.29 | 3.50 | 3.54 |
| Average Hernia Volume (cm³) | 215.50 | 70.89 | 86.30 | 215.50 | 79.00 |
| Average External Inguinal Ring Size (cm) | 3.25 | 2.42 | 2.35 | 3.25 | 2.38 |
| Average Mesh Length (cm) | 13.50 | 8.44 | 7.35 | 13.50 | 7.87 |
| Average Mesh Width (cm) | 11.50 | 10.72 | 11.60 | 11.50 | 11.18 |
| Average Mesh Area (cm²) | 160.50 | 89.17 | 89.85 | 160.50 | 89.53 |
| Average Length of Hernial Sac (cm) | 9.00 | 6.50 | 7.60 | 9.00 | 7.08 |
| Average Width of Hernial Sac (cm) | 4.50 | 3.83 | 4.63 | 4.50 | 4.25 |
| Average Height of Hernial Sac (cm) | 3.00 | 3.00 | 3.19 | 3.00 | 3.10 |
| Average Volume of Hernial Sac (cm³) | 108.00 | 99.03 | 135.10 | 108.00 | 118.01 |
| Average Operative Time (Minutes) | 37.50 | 45.28 | 50.25 | 37.50 | 47.89 |
By comparing surgical and hernia metrics between Spinal and Endotracheal anesthesia, we found:
Our findings could suggest that Endotracheal anesthesia is linked with the cases of longer hernia durations and larger meshes, while Spinal anesthesia is more common for less severe cases with shorter operative times.
By comparing the duration of total hospitalization between both groups we estimated its correlation with arterial hypertension [Table 15].
Table 15: Comparison of Total Hospitalization Duration in both Groups.
| Metric | Group A (Normotensive) | Group B (Hypertensive) |
| Mean | 4.9 | 4.95 |
| Variance | 2.31 | 1.10 |
| Observations | 20 | 20 |
| Pooled Variance | 1.70 | - |
| t Stat | -0.12 | - |
| P(T<=t) two-tail | 0.90 | - |
| t Critical two-tail | 2.02 | - |
The p-value (0.90) indicates no statistically significant difference in hospitalization duration between the two groups.
Upon comparing the effect of duration of herniation upon the surgical outcomes in both groups [Table 16].
Table 16: Comparison of Duration of Herniation (Months) in both Groups
| Metric | Group A (Normotensive) | Group B (Hypertensive) |
| Mean | 24.75 | 22.7 |
| Variance | 1473.57 | 388.22 |
| Observations | 20 | 20 |
| Pooled Variance | 930.89 | - |
| t Stat | 0.21 | - |
| P(T<=t) two-tail | 0.83 | - |
| t Critical two-tail | 2.02 | - |
The p-value (0.83) suggests no statistically significant difference in the duration of herniation between the groups.
Upon comparing the average operative-times in both groups aiming at estimating possible effects of arterial hypertension on the time of hernia repair [Table 17].
Table 17: Comparison of Operative Time (Minutes) in Group A and Group B
| Metric | Group A (Normotensive) | Group B (Hypertensive) |
| Mean | 44.5 | 50.25 |
| Variance | 115.53 | 159.14 |
| Observations | 20 | 20 |
| Pooled Variance | 137.34 | - |
| t Stat | -1.55 | - |
| P(T<=t) two-tail | 0.13 | - |
| t Critical two-tail | 2.02 | - |
The p-value (0.13) indicates no statistically significant difference in operative time between the two groups.
In our study, we found that duration of herniation, operative-time, total hospitalization stays as well as the complications during both the postoperative and short-term follow up periods, for all these metrics—the results of the t-tests show no statistically significant differences between Group A (Normotensive Patients) and Group B (Hypertensive Patients), suggesting that arterial hypertension status does not significantly impact these metrics even with the presence of comorbidities.
On the other hand, right sided inguinal hernias, were shown to have larger dimensions and longer operative times in comparison to left sided inguinal hernias. Furthermore, direct inguinal hernias were found to attain larger volumes in hypertensive patients. These findings could suggest that the site and type of inguinal hernia could affect the outcomes of hernia repair, regarding size of mesh and operative-time.
Authors have no conflict of interest to declare.
This publication was prepared without any external source of funding.
Andrey Protasov, Mekhaeel Mekhaeel, Sameh Salem, Khalid Al-Tekreeti - conceptualization, writing original draft, review and editing, project administration; Mekhaeel Mekhaeel, Sameh Salem, Khalid Al-Tekreeti, Eman Abdo, Abdalhakem alhatem– visualization, Andrey Protasov – supervision.