- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 1. DOI 10.35630/2025/15/1.117
Cutaneous manifestations of digestive system diseases have different pathomechanisms, from autoimmune disorders, as in inflammatory bowel disease or celiac disease, through disturbed liver metabolism in acute and chronic liver diseases, to parasitic infections. Skin changes accompanying digestive system diseases may be one of the first symptoms of the disease. In Crohn's disease, 25% of patients had skin lesions before the official diagnosis was made. Skin manifestations can be discreet, such as itching, excoriations or rash, to spectacular, such as fissures or abscesses. The most common skin complaints of gastrointestinal diseases are recurrent aphthous ulcers, erythema nodosum, skin discoloration, pyoderma gangrenosum, and perianal fistulas or abscesses. Correct diagnosis of all changes is extremely important, because the primary cause may occur in an organ other than the skin. When a patient reports skin symptoms, an underlying digestive cause should be considered.
Methods: We conducted a review of scientific publications and specialist literature on digestive system diseases and their skin manifestations. Information was gathered using the PubMed database, Google Scholar search engine, and medical texts from relevant disciplines. The analysis focused on identifying connections between gastrointestinal disorders and associated dermatological symptoms.
Conclusion: Cutaneous manifestations of digestive system diseases often precede their diagnosis and can range from mild symptoms, such as rashes or itching, to severe conditions like abscesses or fistulas. Recognizing these skin changes is crucial, as they may indicate underlying gastrointestinal disorders, including autoimmune or metabolic dysfunctions. Vigilance in linking skin symptoms to potential digestive causes ensures accurate diagnosis and effective treatment.
Keywords: Pyoderma Gangrenosum; Stomatitis; Digestive System; Autoimmune Diseases; Abscess; Fistula
The skin is an organ with an area of approximately 2m2 that performs important functions in the proper functioning of the body, ranging from its protective role to participation in metabolic and immune processes of the body. Skin manifestations occur in the course of many diseases, including diseases of the digestive system. A properly collected medical interview with the patient and a physical examination often guide the doctor to the correct diagnosis, because skin lesions are often one of the first disturbing symptoms with which the patient reports. The following article presents selected diseases of the digestive system with characteristic skin manifestations.
The aim of this study is to comprehensively present and discuss the cutaneous manifestations of gastrointestinal diseases, their pathophysiological mechanisms, and their significance in clinical diagnostics. In recent years, increasing attention has been given to the connections between the immune system, gut microbiota, and the skin, opening new perspectives in the diagnosis and treatment of gastrointestinal diseases with dermatological symptoms. This study reviews the latest scientific research highlighting the importance of the gut-skin axis, the role of gut dysbiosis, and the impact of biological therapies (e.g., TNF-α inhibitors) on skin changes in patients with inflammatory bowel disease (IBD).
One of the key aspects discussed in the study is the early occurrence of skin manifestations as a precursor to gastrointestinal diseases, emphasizing the role of dermatologists and internists in the early recognition of these conditions. Special attention is given to the frequency and characteristics of skin lesions in patients with IBD, celiac disease, and liver diseases, as well as their possible associations with genetic mutations and metabolic disorders.
A novel approach in this field is the analysis of the impact of elimination diets and gut microbiota on the skin symptoms of gastrointestinal diseases, which could be significant for personalized patient therapy. Recent studies increasingly point to the role of probiotics, prebiotics, and lifestyle modifications in alleviating both skin and intestinal symptoms.
We analyzed scientific publications and specialist literature on digestive system diseases and skin manifestations of selected diseases. To search for information, we used the PubMed website, the Scholar search engine and scientific literature from selected branches of medicine.
We have focused on most common digestive diseases that manifest with skin symptoms. Among them are Crohn’s Disease, inflammatory bowel disease, ulcerative colitis, celiac disease, liver diseases and gastrointestinal infections.
Crohn's disease (CD) belongs to a group of diseases known in scientific nomenclature as inflammatory bowel disease. It is characterized by a chronic inflammatory process, initially in the mucous membrane, and over time affecting all layers of the digestive tract wall. CD can affect any part of the digestive tract.[14] This disease is characterized by periods of relapses and remissions, and the most common symptoms include abdominal pain, severe diarrhea, weakness, weight loss due to malabsorption syndrome and characteristic skin changes, which will be discussed in detail. [14]
The exact cause of Crohn's disease is not fully understood, but it is thought to be influenced by a combination of factors such as genetic predisposition, environmental factors, immune system dysfunction, and the body's abnormal response to gut bacteria. [4,27] The immune
system mistakenly attacks healthy cells of the digestive tract, which leads to chronic inflammation, the formation of ulcers, fistulas and narrowing of the intestinal wall. The chronic inflammatory component in CD is probably caused by impaired activation of Th1 and Th17 immune pathways with simultaneous increased levels of interleukin 23 and 17. [4] This inflammation interferes with the normal functioning of the digestive system, causing symptoms associated with Crohn's disease. Interestingly, patients with a mutation in the TRAF3IP2 gene are predisposed to skin manifestations. [4]
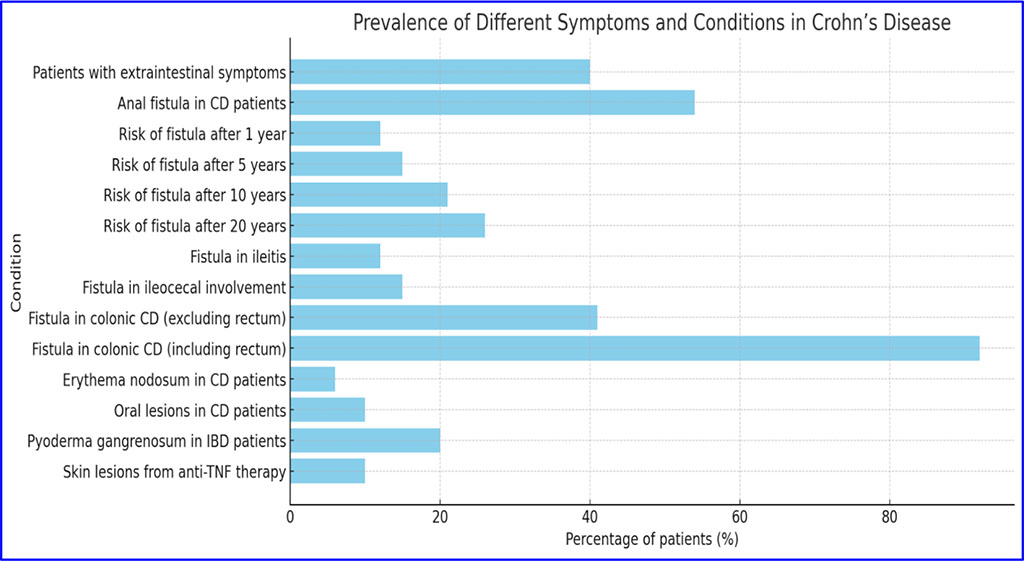
Approximately 40% of patients diagnosed with CD experience at least one extraintestinal symptom, with skin lesions being the most common manifestation in these patients. It should be emphasized that symptoms outside the digestive system occur before the official diagnosis of CD in as many as 25% of patients. That is why cooperation between specialists is so important for quick diagnosis and diagnosis of the disease, which speeds up the introduction of appropriate therapy. [4] Skin abnormalities resulting from the spread of intestinal disease to the skin commonly occur around the anus and face. During examination, skin lesions may manifest themselves in the form of ulcers, fistulas and fissures on an erythematous background or abscesses, while histopathological examination results may reveal non-caseous granulomatous inflammation. Cases of verrucous lesions resembling condyloma acuminata have also been reported.[5,11]
The presence of an anal fistula in patients with Crohn's disease occurs in approximately 54% of patients in whom inflammatory changes are located in the distal part of the digestive tract.[19]
It is usually complex and accompanied by difficult-to-heal fissures, inflammatory infiltrates and abscesses. Anal fistula and its accompanying changes have a dynamic course, which often results in narrowing of the anal canal and rectum and hypertrophy of anodermal folds.
The location of inflammatory changes in the anorectal area is considered a poor prognostic factor in the course of the disease. Studies conducted on the population have shown that the risk of fistula increases with the duration of the disease. It affects 21% to 23% of patients, with approximately 12% occurring in the first year of the disease, 15% after 5 years, 21% after 10 years, and even 26% after 20 years of the disease. There is also a relationship between the location of the primary site and the formation of fistulas. In ileitis, a fistula in the anus occurs in 12% of patients, and in 15% of patients with ileocecal involvement. When the disease affects the colon excluding the rectum, a fistula occurs in approximately 41% of patients, while in the case of inflammation of the large intestine, including the rectum, it may occur in up to 92% of people. Changes around the anus may be an initial symptom of Crohn's disease, the first symptom or occur simultaneously with intestinal symptoms.[19,11,22]
The skin changes that may accompany CD are caused by abnormalities in the HLA system and are associated with a chronic inflammatory reaction in the body. Interestingly, the appearance and intensity of cutaneous manifestations usually correspond to the level of activity of the intestinal disease. An example is erythema nodosum, associated with rheumatological diseases. The incidence in patients with Crohn's disease is 6-15%.[4] It is located on the front surface of the shin in the form of tender nodules on an erythematous background. Histologically, these changes are a limited inflammation of the subcutaneous fat tissue, starting initially in the interlobular septa. Erythema nodosum is characterized by small, painful skin protrusions that may merge with each other and leave brown skin discolorations, but when fully healed they leave no trace [5] The histopathological result shows septal panniculitis.[4] The appearance of erythema nodosum correlates with the severity of intestinal symptoms of CD. Among the skin lesions associated with Crohn's disease, lesions in the oral cavity are quite common, affecting approximately 10% of patients, who may develop aphthous ulcers, purulent stomatitis or periodontitis. Although each symptom manifests differently, all three share the common aspect of causing discomfort and pain in the mouth. Patients with aphthous stomatitis develop painful, shallow ulcers with a fibrous, greasy base, often surrounded by erythema on the mucous membrane of the cheek or lips.[4,5]
Pyostomatitis vegetans similarly affects the mucous membrane of the lips and cheeks, showing delicate tissue with scattered erosions and ulcerations. Although periodontitis is not exclusively a consequence of Crohn's disease or ulcerative colitis, more severe disease has been observed in patients with IBD. [4,22]
Pyoderma gangrenosum occurs in 20-50% of patients with inflammatory bowel disease. It is more often associated with ulcerative colitis, but it can also occur in patients suffering from Crohn's disease.[4] The lesions usually begin as tender papules surrounded by an erythematous edge that gradually turns purple. The area then becomes necrotic, leading to the formation of an ulcer. The most advanced lesions develop as an ulcer with a sterile, purulent base and irregular, washed-out, brown edges.[5] In adults, the most common site of occurrence is the lower limbs, while in children they are more often located on the head or in the genital area. Pyoderma gangrenosum disappears leaving scars. Diagnosis is usually based on clinical observation, because histopathological results are usually non-specific - culture results are usually sterile, and the examination reveals neutrophilic infiltration.[4,5] Anti-TNF preparations used in the treatment of Crohn's disease may also induce the appearance of lesions. skin in the course of the disease. It is estimated that approximately 10% of patients with inflammatory bowel disease taking therapy based on these drugs will develop cutaneous manifestations. Most often, these are eczema or psoriatic lesions.[4]
Inflammatory bowel disease (ulcerative colitis) is a non-specific inflammatory condition of the intestines, resulting from an abnormal and excessive immune response to antigens of the normal intestinal microflora. [14] In the course of the disease, increased activity of CD4+ lymphocytes and Th2 is observed (leading to the release of cytokines such as IL-4, IL-5, IL-13). Additionally, there is activation of macrophages that secrete cytokines: IL-1, IL-6, IL-8, TNF-α. Neutrophils, lymphocytes, eosinophils, and macrophages play a major role in the inflammatory infiltrates in the pathomechanism. Accumulation of histamine, leukotrienes, and prostaglandins in the intestinal wall results in increased vascular permeability and edema, leading to increased mucus production. [12] Consequently, this damages the mucosal barrier, allowing toxins from bacteria to penetrate deeper into the intestinal wall. The changes affect only the large intestine. Crohn's disease’s continuous nature differs from that Inflammatory Bowel Disease’s. They typically localize in the mucosal and submucosal layers of the rectum and/or colon. In advanced stages, they can lead to ulcers, which tend to merge. The disease exhibits periods of exacerbation and remission, classified according to Truelove and Witts for assessing the severity of disease flares (mild form <4 bowel movements with blood per day, severe form <6 bowel movements with blood per day, and moderate form >4 bowel movements with blood per day). [14,2]
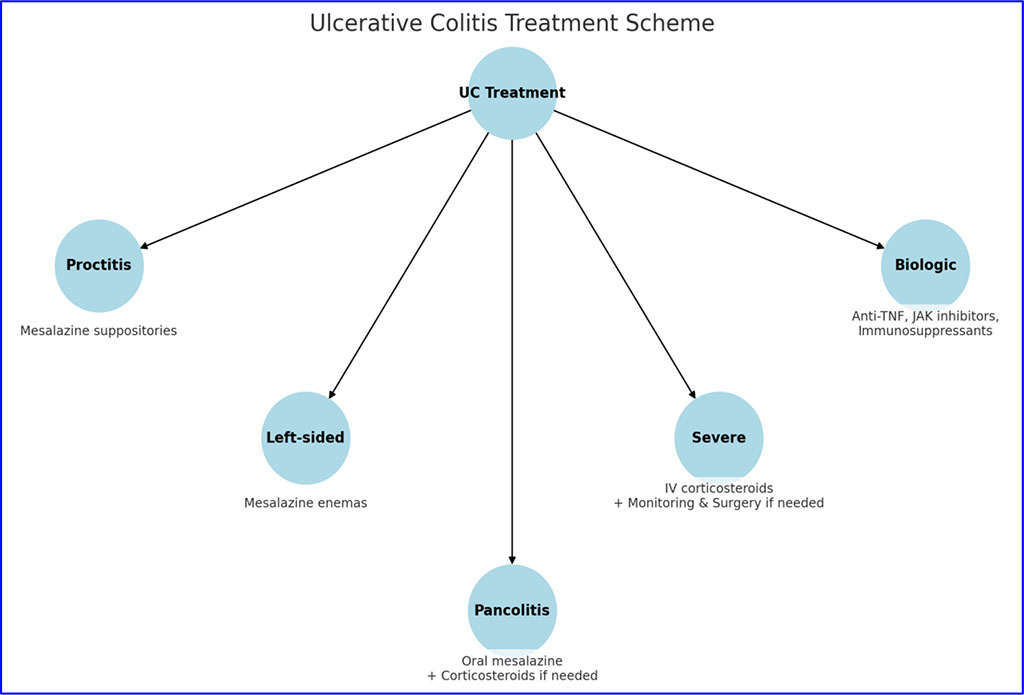
The diagnosis of ulcerative colitis includes laboratory tests revealing increased CRP and ESR levels, anemia, hypoalbuminemia, and autoantibodies against perinuclear neutrophil antigen (pANCA). Other diagnostic methods include endoscopic, histological, and imaging studies. A diagnosis is made based on the aforementioned examinations. [14,15]. Ulcerative colitis (UC) is a chronic inflammatory disease of the colon that requires individually tailored treatment depending on the location and severity of the lesions. Below are general therapeutic schemes based on current guidelines.[9]
Erythema nodosum occurs in approximately 15% of patients with non-specific inflammatory bowel diseases. It is characterized by tender, reddish-brown inflammatory nodules located on the lower (shins) and upper (forearms) extremities. These changes usually resolve within about 2 weeks.[13]
Pyoderma gangrenosum is the most severe cutaneous manifestation in the course of ulcerative colitis, occurring in about 5% of patients. It is characterized by the presence of nodules and pustules throughout the body, which rapidly transform into purple and elevated ulcers with poorly defined borders. They persist for many months or even years, leaving extensive scars after healing. [21]
Psoriasis is a common skin condition, occurring in about 11% of the population dealing with non-specific inflammatory bowel diseases. Symptoms include plaques and scales located on the knees, elbows, and the sacroiliac area. [5]
Celiac disease is an autoimmune disorder that occurs at various stages of life in individuals predisposed with the HLA-DQ2 or HLA-DQ8 antigen. This disease arises due to gluten intolerance, a protein found in wheat, barley, and rye. [14] The main mechanism of the disease involves an inflammatory response and the production of pro-inflammatory cytokines, leading to the activation of macrophages and fibroblasts that produce metalloproteinases intensifying the apoptosis of enterocytes.[29] Antibodies against tissue transglutaminase (tTG) inhibit the differentiation of enterocytes, resulting in the atrophy of intestinal villi. The consequence of atrophy is a reduced absorptive surface of the intestine, leading to deficiencies in calcium, iron, vitamin D3, and folic acid, which can cause gastrointestinal disturbances and skin manifestations. [14,6]
The diagnosis of celiac disease is based on serological tests, including the detection of antibodies: TTG IgA, EMA IgA, DGP IgG, TTG IgG, anti-gliadin IgA, IgG, and IgA in individuals who have consumed gluten in the last month. Another diagnostic method involves histopathological evaluation of duodenal biopsies, which should be performed in individuals consuming gluten for at least two weeks. [5,1]
The treatment of celiac disease primarily involves a gluten-free diet (facilitating the regeneration of intestinal villi) and the use of immunosuppressive drugs the use of these being less extended. [14]
A dermatological manifestation of celiac disease is Dermatitis Herpetiformis, a blistering skin inflammation. The disease is characterized by erythema, blisters, vesicles, pustules, papules, and urticarial blisters most commonly located on elbows, forearms, neck, knees, and buttocks. Additionally, numerous blisters and erosions may occur in the oral mucosa. [25] Patients with Dermatitis Herpetiformis complain of intense itching and burning in the mentioned areas. The pathomechanism of the disease involves the presence of granular deposits of immunoglobulin A within the skin papillae. Despite the aforementioned symptoms, the disease can have a latent course in individuals with celiac disease, but it can also be present in the general population in the case of the occurrence of the relevant HLA antigens. [17] The course of the disease is prolonged, relapsing with periods of remission. Factors exacerbating symptoms may include iodine present in medications, the environment, or food. To diagnose the disease, it is necessary to:
Dermatitis Herpetiformis is differentiated from pemphigoid and drug rash. Treatment begins with pharmacotherapy, including the use of sulfones such as dapsone (which does not alleviate gastrointestinal symptoms). A gluten-free diet is recommended to alleviate gastrointestinal disorders, influencing the improvement of skin lesions after approximately 7 months of its introduction. This allows for the discontinuation of pharmacological treatment, which carries numerous adverse effects such as anemia, jaundice, or polyneuropathy. [17,7]
Currently, it is believed that many dermatological changes are caused by disturbed hepatic metabolism. Cutaneous manifestations accompany both acute and chronic liver diseases. [26]
Skin lesions can be discreet and manifest themselves as scratches, hair loss under the arms or gynecomastia. Localized or generalized skin redness, palmar erythema, paper-money skin, rosacea and rhinophyma are common manifestations of liver disease that are often overlooked by physicians.[20,10] Generalized discoloration is associated with porphyria cutanea tarda, hemochromatosis, megaloblastic anemia (vitamin B12 and folic acid deficiency), malabsorption syndrome and Whipple's disease. [26] Jaundice, telangiectasia, leukonychia and clubbing of the fingers are known and often associated with liver diseases. [20]
The shade of jaundice is important in determining the pathogenesis of the disease. A yellow-red skin tone (rubinicterus) indicates the presence of hepatic bilirubin in the blood and tissues. Jaundice may manifest itself as a green-yellow discoloration of the skin (verdinicterus) and suggests a chronic disease state. It may occur with biliary cirrhosis, sclerosing cholangitis or accompany chronic gastrointestinal obstruction caused by tumor masses. [23] The brown-black (melasicterus) shade of the external integuments of the body or lemon-yellow (flavinicterus) indicates the extrahepatic origin of jaundice, usually hemolytic. Please remember that jaundiced skin does not take on a uniform color. The change in shade begins in the upper parts of the body - initially it affects the sclera and palate, and then affects the trunk and limbs. The shade intensifies with each intensification of the disease, and the greatest accumulation of pigment is in the areas affected at the beginning. Therefore, the duration of jaundice in the upper parts of the body is the longest.[26] Yellow patches appearing on the upper and lower eyelids are common skin lesions accompanying chronic primary liver cirrhosis and hypercholesterolemia. Vitiligo, dry skin and melanosis are less frequently observed. [20]
Liver diseases with cholestasis are accompanied by chronic, generalized itching. Often, it is the first symptom of ongoing liver disease. Initially, it affects the distal parts of the body, and the symptoms are most severe at night. As a result of chronic, troublesome itching, excoriations appear on the skin.
Staying on the topic of gastrointestinal diseases, we should also mention parasitic infections affecting this system. Parasitic infections of the gastrointestinal tract constitute a significant public health burden in developing countries, affecting millions of people each year. [18]
Intestinal parasites such as Giardia lamblia (lamblia), Entamoeba histolytica (dysentery amoeba), Enterobius vermicularis (pinworm), Ascaris lumbricoides (roundworm), Taenia saginata (unarmed tapeworm) and Taenia solium (armed tapeworm) may contribute to to the occurrence of urticarial eruptions in the form of urticaria wheals accompanied by swelling of the dermis or other chronic or recurrent allergic skin reactions. [5,16]
The main symptom of infection with the nematode Enterobius vermicularis (pinworm) parasitizing the gastrointestinal tract is intense itching around the anus, which intensifies at night. Continuous scratching of this area may lead to injuries around the anus, excoriation and complications in the form of secondary bacterial infections. The cutaneous form of amoebiasis caused by Entamoeba histolytica is characterized by lesions of the skin and subcutaneous tissue caused by ameotrophoites, located in the anus and perineum. This symptom is rare, most often observed among infants, and is related to prolonged contact with contaminated feces caused by diapers. Continuous exposure of irritated anal skin to trophozoites results in the development of characteristic ulcers with pus-secreting sinuses in the diaper area of the buttocks, perineum and inguinal folds. If left untreated, lesions may cause serious tissue damage requiring surgical intervention. In adults, amoebiasis can be transmitted sexually and mainly affects men who have sex with men (MSM). In these types of cases, ulcers occur on the anus and penis. [18,14]
Gastrointestinal infections caused by protozoa - Giardia lamblia, as well as those of bacterial etiology (e.g. Yersinia enterocolitica, Salmonella enteritidis) may have cutaneous manifestations in the form of erythema nodosum and pyoderma gangrenosum described above. There are reports suggesting a connection between ascariasis infection and lung infection in the etiology of erythema nodosum. [3,28] It is currently suggested that Helicobacter pylori, in addition to its proven association with inflammation of the gastric and duodenal mucosa, peptic ulcer disease and cancer, may play a role in the pathogenesis of diseases of the cardiovascular, nervous and pulmonary systems as well as autoimmune and metabolic diseases. There are references in publications pointing to the role of H. pylori in the pathogenesis of skin diseases. These include psoriasis, chronic urticaria and rosacea. In the course of rosacea, papulopustular lesions located in the central part of the face and fixed telangiectasia with an erythematous base are observed. In men aged 40-50, the hypertrophic form most often develops, the lesions are located mainly on the nose (i.e. rhinophyma). [24]
| Skin manifestations | Characteristics of skin changes | Disease |
| Erythema Nodosum | painful, tender nodules on an erythematous background, typically located on the shins; can merge and leave brown discolorations upon healing, but do not leave scars |
|
| Pyoderma Gangrenosum | usually found on lower limbs; begins as tender papules with an erythematous edge that turn purple and become necrotic, leading to ulcers with a purulent base and irregular brown edges |
|
| Aphthous Stomatitis | on the mucous membrane of the cheek or lips; painful, shallow ulcers with a fibrous base, surrounded by erythema | Crohn’s Disease |
| Pyostomatitis vegetans | affects the mucous membrane of the lips and cheeks; showing delicate tissue with scattered erosions and ulcerations | Crohn’s Disease |
| Perianal Fistulas and Ulcers | ulcers, fistulas and fissures on an erythematous background or abscesses; often results in narrowing of the anal canal and rectum and hypertrophy of anodermal folds | Crohn’s Disease |
| Psoriasis | plaques and scales located primarily on the knees, elbows, and sacroiliac area |
|
| Dermatitis Herpetiformis | typically found on the elbows, forearms, neck, knees, and buttocks; characterized by erythema, blisters, vesicles, pustules, and papules; presence of itching and burning in affected areas | Celiac Disease |
| Rosacea | located on the face; papulopustular lesions and fixed telangiectasia with an erythematous base; rhinophyma | Potentially linked to the Helicobacter pylori infection |
| Jaundice | yellowing of the skin and sclera |
|
In this paper, we focused on the most common diseases that manifest with skin symptoms. Every doctor may encounter such conditions in their practice, which is why it is important to consolidate knowledge about them and pay attention to skin symptoms in patients. Skin manifestations of gastrointestinal diseases have various causes, ranging from parasitic infections to genetically conditioned disorders. The type of skin eruptions depends on the underlying cause of the gastrointestinal disease. The treatment of such cases also depends on the nature of the disorder. Effective methods include elimination diets, as in the case of celiac disease, steroid therapy for conditions such as ulcerative colitis, and antibiotic therapy for parasitic-related disorders. In many cases, the elimination or regression of gastrointestinal disease can lead to a complete resolution of skin changes in patients. This topic is extensive, and it is crucial to remember that skin manifestations may not be exclusively related to gastrointestinal diseases, so a thorough and comprehensive diagnosis is necessary for patients presenting with such issues.