- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 1. DOI 10.35630/2025/15/1.111
Sleep is a physiological process essential for maintaining both physical and mental health, it plays a significant role in various bodily functions. Throughout life, changes in sleep duration and quality can impact overall well-being. This literature review explores the complex relationship between sleep disorders and conditions such as depression, Alzheimer's disease, type 2 diabetes, and cardiovascular diseases. Research indicates that sleep disorders, including sleep deprivation and interrupted sleep, can influence the development and progression of these diseases. In Alzheimer's disease, poor sleep quality contributes to the accumulation of beta-amyloid plaques, which impair cognitive functions. Inadequate sleep also negatively affects the onset of type 2 diabetes by disrupting glucose metabolism and insulin sensitivity. Additionally, both insufficient and excessive sleep have detrimental effects on cardiovascular health, highlighting the importance of sleep in the pathogenesis of these conditions.
Purpose: This review emphasizes the multidimensional impact of sleep on health, highlighting the necessity for effective treatment of sleep disorders as a preventive measure against various diseases.
Methods: After a thorough analysis of articles on PubMed, we have selected the most significant diseases whose development and progression are influenced by sleep disorders. We provided a brief overview of the mechanisms underlying sleep and then carefully described the relationships between sleep and the selected diseases. Our aim is to emphasize the significant impact that sleep has on the overall functioning of the body.
Conclusion: Sleep plays a crucial role in maintaining health and preventing the development of many diseases. Sleep disorders can impair immune system function, increasing the risk of infections and autoimmune diseases. Sleep deprivation also contributes to cardiovascular diseases, such as hypertension and atherosclerosis, by disrupting blood pressure regulation and inflammatory processes. Lack of sleep negatively affects metabolism, raising the risk of type 2 diabetes and obesity. Additionally, chronic sleep disorders are linked to deteriorating mental health, including the development of depression, anxiety, and dementia.
Keywords: Sleep Deprivation, Sleep Duration, Diabetes, Sleep Quality, Cardiovascular Diseases, Insulin Resistance
Sleep is a physiological process that plays a crucial role in maintaining health and overall well-being. Sleep duration and requirements undergo significant modifications throughout an individual's lifespan, with a systematic decrease in sleep needs as age progresses. [6] The American Academy of Sleep Medicine and the Sleep Research Society recommend ≥7 hours of sleep per night for adults aged 18–60 [38], while the National Sleep Foundation suggests 7–9 hours for adults (aged 18–64) and 7–8 hours for older individuals (aged ≥65) [13]. Sleep disorders represent a substantial public health concern affecting a significant portion of the population. Epidemiological studies demonstrate that approximately 30% of adults experience various sleep disturbances [32]. The importance of adequate sleep extends far beyond mere rest, playing a critical role in multiple physiological processes. A 2021 study published in the journal Sleep Medicine analyzed the global prevalence of insomnia. The results indicate that approximately 30% of adults worldwide experience symptoms of insomnia, and approximately 10% meet diagnostic criteria for chronic insomnia. This frequency varies depending on the region and the research methods used.[1] In Poland, there are no large-scale epidemiological studies on insomnia published after 2020. However, studies conducted in Central and Eastern Europe suggest that the prevalence of insomnia symptoms in this region is similar to the global average.
However, it is important to note that the COVID-19 pandemic has had a significant impact on mental health, including an increase in sleep problems, which may impact current statistics. [27]. Optimal sleep quantity and quality are essential for maintaining proper metabolic function, supporting immune system responses, and regulating emotional processes [19,22]. Emerging research consistently highlights sleep's profound impact on cognitive functions and endocrine system regulation, positioning it as a crucial factor in chronic disease prevention. [35, 29] Poor sleep hygiene has been strongly associated with increased risks of mental health disorders, particularly depression and anxiety [19,26]. Moreover, a growing body of scientific evidence suggests a significant correlation between sleep disturbances and neurodegenerative conditions, including Alzheimer's disease. [11] Research has also established links between inadequate sleep and increased risks of cardiovascular diseases and type 2 diabetes. Sleep disorders can lead to dysregulation of glucose metabolism, potentially contributing to obesity and metabolic syndrome [32].
This comprehensive literature review aims to examine the multifaceted impact of sleep and its disorders on human physiological functioning. We will specifically focus on the intricate relationships between sleep patterns and critical health conditions, including depression, Alzheimer's disease, type 2 diabetes, and cardiovascular disorders. Our goal is to highlight the importance of healthy sleep as a fundamental element in disease prevention and holistic health management.
After analyzing PubMed articles, we identified key diseases linked to sleep disorders. We briefly outline sleep mechanisms and detail its connections to these diseases, highlighting sleep’s crucial role in overall health.
Sleep is a complex process regulated by the brain. It consists of two main stages: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. [14] The reticular formation, located in the brainstem, regulates muscle tone, cortical arousal, and the activity of other brain structures, such as the thalamus. Changes in the activity of its various parts determine whether we remain alert or transition into sleep. The reticular formation in the pons contains an EEG desynchronization center, whose activity counteracts sleepiness. The intensity of neurotransmitter release varies between wakefulness and different sleep phases. Norepinephrine, serotonin, and acetylcholine play crucial roles in regulating cortical arousal, which in turn influences the form and content of dreams during REM and NREM sleep. [36]
The hypothalamus regulates circadian rhythms via the suprachiasmatic nucleus (SCN), which synchronizes the sleep-wake cycle with environmental cues, such as light and darkness. The SCN also controls melatonin secretion from the pineal gland, signaling the body when it is time to sleep. Meanwhile, the thalamus acts as a gateway, transmitting sensory information to the cerebral cortex. During NREM sleep, thalamic activity decreases, allowing a reduction in the processing of external stimuli. The cerebral cortex plays a key role in processes such as memory consolidation, regeneration, and the formation of dream content.[14]
NREM sleep consists of three stages according to the current AASM classification. It is characterized by a decrease in consciousness and brain activity. During REM sleep, the brain becomes more active, vivid dreams occur, and the body experiences muscle paralysis. Various neurotransmitters, hormones, and brain regions coordinate this cycle, ensuring restorative functions, memory consolidation, and regulation of immune system activity. The sleep-wake cycle is influenced by the body’s internal clock, known as the circadian rhythm, which responds to environmental cues such as light and darkness. [14,4] Factors such as stress, lifestyle, and certain health conditions can also affect sleep quality and duration. The sleep cycle and its stages can be observed through electroencephalographic (EEG) recordings, which display electrical patterns of brain activity. A sleep episode begins with NREM sleep, which smoothly transitions into REM sleep, forming alternating cycles. One sleep cycle lasts an average of 90 minutes. For sleep to be restorative, it should consist of multiple cycles; for example, six hours of sleep includes four full sleep cycles. [14,4]
Stages 1 and 2 of NREM sleep are considered light sleep, while stage 3 represents deep sleep. Falling asleep involves processes such as a reduction in acetylcholine levels. The pons ceases to stimulate the sensory part of the thalamus and stops inhibiting the reticular nucleus of the thalamus, which begins to generate oscillations. These oscillations are then transmitted to the central sensory part of the thalamus and subsequently to the cortex, manifesting as synchronization in the EEG, observed as slow waves. Characteristic of NREM sleep are EEG recordings dominated by high-amplitude slow waves. This is a time when heart rate and respiratory rate decrease, and eye movements are slow. [36]
In the first stage of NREM sleep, brain activity transitions from wakefulness, characterized by rhythmic alpha waves in the EEG, to low-voltage waves of mixed frequency. During this stage, the EEG predominantly shows low-amplitude and mixed-frequency waves, transitioning from alpha rhythm to theta waves. This is the onset of sleep, lasting a few minutes and easily disrupted by environmental noise.
In the second stage of NREM sleep (light sleep), brain activity displays low-voltage waves, with sleep spindles and K-complexes appearing in the EEG. [14] Sleep spindles are bursts of brain activity, with wave frequencies averaging 12-16 Hz and lasting 0.5 to 1.5 seconds. K-complexes are characterized by single, high-amplitude waves. This stage lasts an average of 20 minutes and lengthens with each sleep cycle. It is the longest stage of NREM sleep. During this stage, brain activity decreases, while heart rate and respiratory rate slow further.
Stage 3 of NREM sleep is also known as deep sleep or slow-wave sleep (SWS). EEG recordings during this stage are dominated by delta waves (0.5–4 Hz) with high amplitude, reflecting maximal synchronization of neuronal activity in the brain. [14] During this stage, growth hormone (GH) secretion peaks, playing a crucial role in tissue regeneration and metabolism. Cortisol levels stabilize and begin to rise in later sleep stages, while cytokine production, essential for proper immune system function, is supported. During slow-wave sleep, declarative memory consolidation occurs. Information gathered during the day is processed and stored in the hippocampus and cerebral cortex.
Stage 3 of NREM sleep is crucial for the deep regeneration of the body, supporting immune, hormonal, and cognitive processes. It is characterized by the dominance of delta waves in the EEG, the lowest level of metabolic activity, and difficulty waking up. Proper functioning of this sleep stage is essential for physical and mental health. [14,4,36]
REM sleep begins approximately 90 minutes after falling asleep and constitutes 20-25% of total sleep. During this stage, vivid dreams occur. EEG recordings show high-frequency, low-amplitude activity, while heart and respiratory rates increase. Rapid eye movements occur during this phase. Additionally, norepinephrine and serotonin levels are minimal, while cholinergic (acetylcholine) activity increases, initiating activity in the pons, lateral geniculate body, and occipital lobe. This process is responsible for the appearance of PGO waves, which generate visual sensations interpreted as dreams. [36]
Muscle atonia is also characteristic of this stage. Most skeletal muscles are completely relaxed due to the action of the GABAergic system, which prevents movement during dreams. [36]
During REM sleep, dreams are intense, often unrealistic, and chaotic. They may include visual, auditory, or falling sensations, resulting from random neural discharges in the pons. Dreams during NREM sleep are less vivid and have a more logical structure.
Table 1. Differences between the NREM and REM sleep phases.
| NREM | REM |
| Stage 1 and 2 - Light Sleep Stage 3 - Deep Sleep | Dreams occur |
| EEG slow waves with high amplitude, low brain activity | EEG high-frequency, low-amplitude waves, high brain activity |
| It lasts about 1 hour, accounting for 75-80% of total sleep time. | It begins 90 minutes after falling asleep, accounting for 20-25% of total sleep time. |
| Reduced heart rate and respiratory rate | Increased heart rate and frequency |
| Slow eye movements | Rapid eye movements |
Depression is recognized as the most common cause of chronic insomnia. However, sleep disturbances often precede the onset of a depressive episode. Research indicates that insomnia may be a prodromal symptom of depression. Therefore, the relationship between depression and sleep should be considered bidirectional [10].
Sleep disorders can lead to the emergence of depressive symptoms by influencing emotional regulation and emotional reactivity. The mechanisms of this phenomenon are still under investigation. Sleep disorders increase the impact of other depression risk factors and reduce the body's adaptive abilities to stressors, hindering regeneration and adaptation to these factors [20].
Both psychological and physical violence are associated with the risk of sleep disorders. In women who have been victims of assault and suffer from insomnia, the risk of developing depression is eight times higher compared to victims who do not experience insomnia [28].
Leggett et al. demonstrated that stressful life experiences, combined with sleep disorders, intensify depressive symptoms [20].
In 17-50% of individuals without depression but experiencing insomnia for at least two weeks within six months, major depression developed later on [5].
In a study on first-year residents with pre-existing sleep disorders and short sleep duration (less than 6 hours), there was an increased risk of developing chronic depression. Furthermore, it was shown that short sleep increases the risk of depression development, regardless of whether it is a recurrence of depression or a new onset [18].
Mendoza et al. found that individuals suffering from insomnia have a higher risk of developing depression compared to those who sleep for a short duration or have poor sleep quality [9].
It is important to note that not all patients with chronic insomnia will develop depression. The development of depression also depends on additional environmental factors (such as stress, lifestyle, coping mechanisms in crisis situations) [31]. Early treatment and diagnosis of insomnia can prevent the development of depression.
Alzheimer's disease is a neurodegenerative disorder characterized by the accumulation of amyloid plaques composed of beta-amyloid, tau proteins, and neuronal loss. Beta-amyloid aggregation in the hippocampus area leads to the formation of amyloid plaques, inhibiting neurogenesis and causing cognitive dysfunction.
In cross-sectional studies, sleep ≤ 5 hours or ≥ 11 hours is associated with an increased risk of cognitive disorders. In other studies, daytime napping, delayed sleep onset, and fragmented sleep are also considered risk factors for the development of Alzheimer's disease [15].
Proper sleep plays a crucial role in removing toxic metabolites deposited in the brain. Sleep increases the flow of cerebrospinal fluid, enhancing beta-amyloid clearance. Studies show a high level of beta-amyloid before sleep and a low level after proper sleep [34,25].
Lucey et al. demonstrated in their study that reduced non-rapid eye movement (NREM) sleep is responsible for beta-amyloid deposition. They suggest that mixed slow-wave sleep occurs in the case of tau protein deposition in healthy individuals or those with mild cognitive impairment [23].
Sleep disorders increase the expression of BACE 1 enzyme and APP protein, which participate in the pathogenesis of Alzheimer's disease. Moreover, these disorders elevate cortisol levels, impairing cognitive function in Alzheimer's patients.
Aquaporin 4 (AQP4) is a water channel in the brain involved in the removal of beta-amyloid and tau proteins, preventing their accumulation. Rainey-Smith et al. showed that patients with less sleep experience a genetic mutation in AQP4 [2,30].
Ju et al. demonstrated that poorer sleep quality over 6 days is associated with higher levels of tau protein in cerebrospinal fluid [16].
Similar to depression, there is a bidirectional relationship between sleep and Alzheimer's disease. Sleep disorders can lead to the development of Alzheimer's disease, while Alzheimer's disease is associated with reduced sleep quality and decreased NREM sleep.[37]
Type 2 diabetes mellitus (T2DM) is currently one of the most frequently diagnosed chronic diseases in a doctor's office. It is believed that by 2045, 783 million people in the world will be sick. [8] Sleep hygiene, in addition to an unhealthy diet, overweight, a positive family history of T2DM, low physical activity and the habit of smoking, is one of the factors influencing the development of type 2 diabetes. [8, 12] A relationship between the duration of sleep and the onset of diabetes has been observed, weight gain, obesity, cardiovascular diseases or stress. It has been found that insufficient sleep causes dysregulation of metabolism and increased immune response, leading to an increased risk of cardiometabolic diseases. [12] The pathophysiology of this phenomenon is explained in a study conducted by Broussard et al., who reported a reduction in cellular insulin sensitivity in adipocytes by approximately 30% after 4 nights of sleep restriction to 4.5 hours/day. Therefore, it could be hypothesized that sleep plays an important role in peripheral metabolism and cellular insulin signaling. [17]
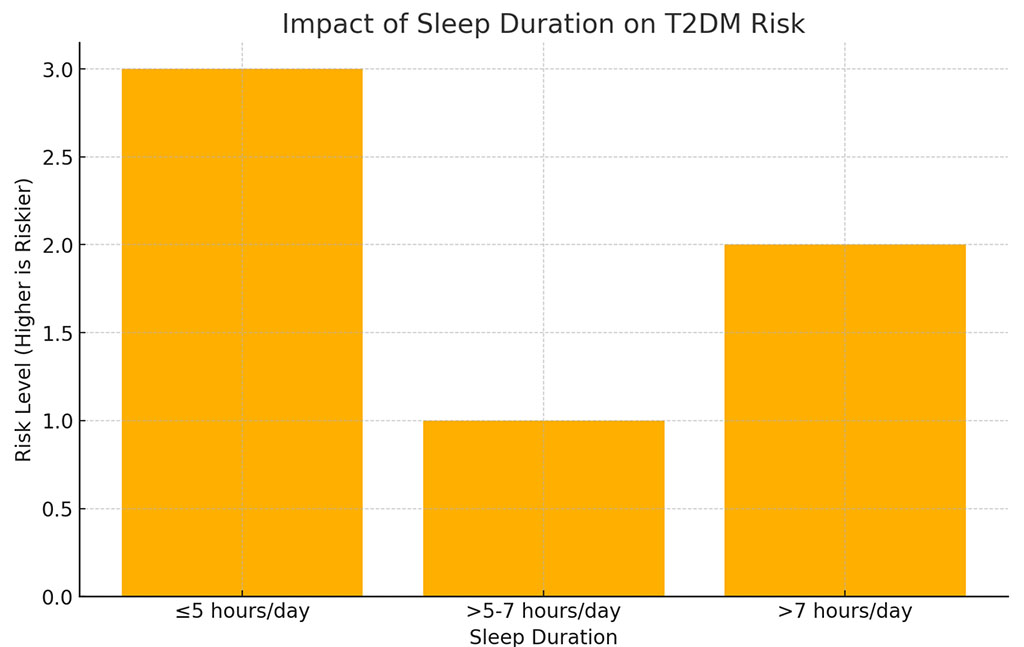
Research conducted by Da Young Lee et all showed that people who sleep ≤5 hours a day have a higher risk of type 2 diabetes compared to people who sleep >5-7 hours a day. Sleep longer than 7 hours did not increase the risk of T2DM. A significant increase in risk was noticed among men. Under 60 years of age, whose average daily duration was less than 5 hours/day. [8]
Increased cardiometabolic risk caused by a sleep deficit of less than 5 hours a day is observed in patients with prediabetes, characterized by increased fasting glucose and glucose tolerance, as well as blood sugar levels of 5.6 and 6.9 mmol/l. Moreover, an increase in hemoglobin A1c (HbA1c), a marker of glucose metabolism, was observed in patients sleeping on average less than 5 hours per day. [12] Studies using continuous glycemia measurements and glucose tolerance tests have shown a significant impact of sleep deprivation on the increase in the incidence of insulin resistance and glucose intolerance. [12]
Numerous studies comparing the impact of sleep deficiency, the risk of T2DM and obesity are also taken into account. The mechanism connecting these components may be behavioral in nature, understood as abnormal health behaviors. Particularly taken into account is excessive daily caloric intake, leading to obesity and other metabolic diseases ultimately resulting in the development of diabetes. [8, 12]
On the other hand, the study conducted by Jung Ah Lee et al does not confirm the correlation between short sleep duration (≤ 5 hours) and the increased incidence of T2DM. According to the above study, the risk of type 2 diabetes was higher in people with poor sleep quality, high BMI, central obesity and a positive family history of type 2 diabetes [17].
Cardiovascular diseases (CVD) account for the largest share of morbidity and mortality in the global population. One-third of cardiovascular-related deaths are classified as premature (before the age of 70), prompting extensive research into risk factors and optimal prevention. CVD encompasses a wide range of conditions affecting the cardiovascular and cerebrovascular systems, including coronary artery disease (CAD), heart failure (HF), and stroke (both ischemic and hemorrhagic). Coronary artery disease is the most frequently diagnosed heart condition, typically including stable angina, unstable angina, myocardial infarction (MI), or sudden cardiac death.
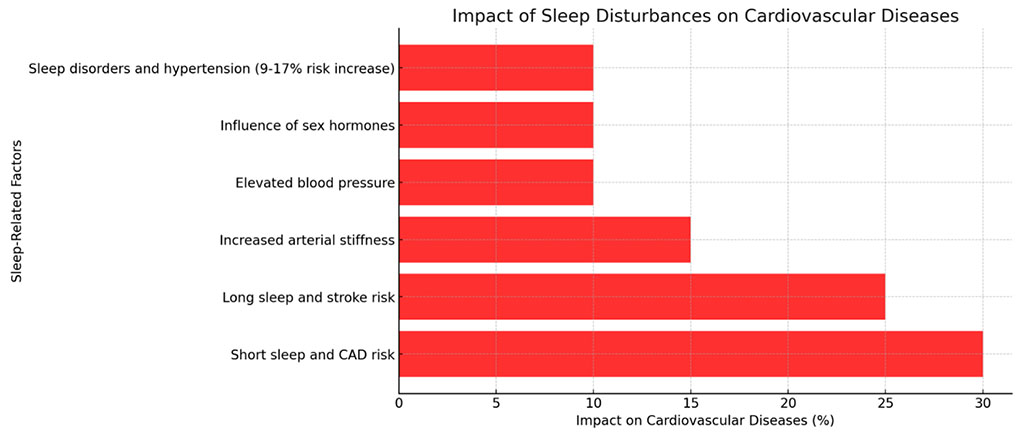
Modifiable risk factors include smoking, an unhealthy diet, low physical activity, and poor sleep hygiene. Numerous studies suggest a significant impact of reduced sleep duration on the risk of cardiovascular diseases. However, conducting controlled, randomized studies on this subject is challenging. Therefore, fully confirming the influence of sleep on the cardiovascular system, independent of other significant risk factors, is not entirely possible. [33, 7] Sleep deprivation has long been considered a component of an unhealthy lifestyle. Pathophysiological mechanisms include fluctuations in ghrelin and leptin levels, serum lipid levels, and overactivation of the autonomic nervous system. Increasing research also points to the negative effects of excessively long sleep durations on the cardiovascular system, particularly their association with increased arterial stiffness. [7]
Some studies indicate differences in how sleep duration and quality affect CVD based on gender. This is attributed to the influence of sex hormones, especially the significant hormonal changes that are more pronounced in women than in men. [13] However, other findings report no association between age or gender and the increased risk of cardiovascular diseases related to sleep. [33, 7] Behavioral and psychosocial factors, on the other hand, have consistently been shown to have an impact. [33, 7, 3]
When assessing the influence of sleep on the cardiovascular system, it is essential to consider sleep duration, patient-reported sleep problems, and sleep disorders—such as interrupted sleep and irregular sleep duration. [21] Irregularity in sleep timing, as measured by total sleep duration, was significantly associated with an increase in hypertension by 9% to 17%. This was also linked to greater variability in systolic and diastolic blood pressure. Studies observed that compared to individuals maintaining a healthy sleep pattern (7-8 hours), those with poor sleep patterns were consistently at higher risk of developing hypertension. [21, 24]
According to recent research, both too short and too long sleep durations influence the risk of coronary artery disease and stroke. In the case of CAD, shorter sleep durations had a significantly greater impact on disease occurrence than longer sleep durations. Conversely, excessive sleep was associated with an increased risk of stroke. It is essential, however, to consider that results may vary depending on the composition of the study population. [33, 7]
Sleep disorders are a common health issue that can have complex consequences for both mental and physical functioning. A thorough review of the scientific literature highlights the multifaceted negative effects of sleep disruptions. Research indicates that sleep disorders significantly exacerbate depressive symptoms, particularly in the context of highly stressful life events. [20] The relationship between sleep and Alzheimer's disease resembles the mechanisms observed in depression, where sleep disorders may initiate the development of the disease, and conversely, Alzheimer's disease can lead to a deterioration in the quality of sleep, especially in the NREM phase. [37]
]Moreover, studies have established a clear correlation between reduced sleep duration and an increased risk of serious metabolic and cardiovascular diseases, including type 2 diabetes, obesity, and cardiovascular conditions. [8] These findings emphasize the critical role that sleep plays in maintaining overall health and preventing serious illnesses.
This literature review emphasizes the key role of sleep in maintaining health and preventing serious diseases, indicating the multidimensional impact of sleep disorders on the functioning of the body.