- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 1. DOI 10.35630/2025/15/1.101
Purpose: This study compares post-operative pain and recovery time in pterygium surgery using fibrin glue for flap closure as well as corneal bandaging (Fibrin CL group) as opposed to vicryl 7.0 suturing of conjunctival flap without corneal bandaging (No CL group).
Methods: A single medical center, randomized, prospective study. Consecutive patients, scheduled for standard pterygium excision surgery were enrolled from 2017 to 2020. Postoperative pain was evaluated with the Brief Pain Inventory at two time points: at 24 hours and one-week post-surgery.
Results: A total of 50 eyes of 50 patients who underwent pterygium surgery were enrolled and were included in the final analysis. Mean pain level at one week after surgery was significantly reduced in fibrin corneal bandage group, mean pain score 2.12 in the fibrin corneal bandage group and 3.20 in the No CL group (p = 0.0304). Maximal pain level after one week was 3.88 in the fibrin CL group and 5.36 in the No CL group (p = 0.07). The mean minimal pain level after one week was 0.76 in the fibrin CL group and 0.80 in the No CL group (p = 0.362). Additionally, the mean duration of overall days of pain within one week was 3.04 in the fibrin CL group and 4.36 in the No CL group (p = 0.0287).
Conclusion: The usage of bandaging corneal surgical wound with fibrin glue may lead to reduced pain levels and a shorter overall duration of pain compared to pterygium surgery without bandaging. Further studies with larger sample sizes and more often follow-up periods are necessary to confirm these findings and explore potential factors contributing to these observed differences.
Keywords: Pterygium; Pterygium surgery; Fibrin glue; Postoperative pain, conjunctival autograft
Pterygium is a benign growth of conjunctival and subconjunctival fibro vascular tissue onto the cornea (Figure 1). Advanced pterygium frequently requires surgical intervention to alleviate symptoms and prevent visual impairment. Over the years, a range of surgical techniques has been employed to achieve successful outcomes, with a focus on minimizing postoperative complications and enhancing patient comfort. Among these techniques, the suturing the conjunctival flap and more recently, the application of fibrin glue, are both employed approaches for securing flaps or grafts during pterygium surgery.
Sutures have been a longstanding standard technique for wound closure in pterygium surgery, providing dependable tissue fixation and enabling precise tension adjustment for optimal wound healing (1).
Fibrin glue, a biological adhesive derived from human plasma, has gained popularity due to its ability to provide secure tissue adhesion without the need for sutures. Both synthetic and biologic fibrin glues have a well-established presence in the field of ophthalmology, with a history of extensive use. Tisseel, a commercially available fibrin bio sealant, has been employed in Europe for over 25 years, facilitating more than 9.5 million surgical procedures. It promotes hemostasis, reduces surgical time, and eliminates the potential complications associated with suture use, such as suture-related discomfort and induced astigmatism (2).
In 2008, Jiang et al. conducted an assessment of the effectiveness and safety of fibrin glue in fixing conjunctival autografts for primary pterygium, comparing it with suturing. Their findings revealed that the application of fibrin glue significantly reduces the operating time and is associated with fewer postoperative symptoms compared to a sutured graft, highlighting the safety of this procedure (3).
However, one critical aspect that demands attention in comparing these techniques is the postoperative pain experienced by patients. Pain following surgery has been shown to correlate with surgical wound size, size of corneal erosion, and presence of bare sclera following surgery. The level of pain and discomfort following surgery can significantly impact the patient's recovery and satisfaction.
Understanding the differences in post-operative pain associated with fibrin glue and sutures is essential for both surgeons and patients in selecting the most appropriate approach for pterygium surgery.
While both closure techniques allow for good approximation of conjunctival wound edges and scleral coverage. Usage of fibrin glue offers an additive effect of the ability to “bandage” the site of corneal surgical erosion in addition to the usage of the fibrin glue to approximate the conjunctival flap or graft.
Numerous studies aim to illustrate the superior efficacy of using fibrin glue over sutures in reducing postoperative pain. In 2007, Baher et al. conducted a comparison of the prolonged outcomes of conjunctival closure using fibrin glue versus Vicryl sutures in pterygium surgery. They observed that employing fibrin glue in this surgical procedure significantly diminishes operative time and alleviates patient discomfort when contrasted with suturing (4).
Both methods fail to address the exposed corneal erosion following surgery, and the resulting pain it creates. We introduce an innovative technique for securing corneal surgical wounds using fibrin glue as a bandage. This approach provides a solution to alleviate post-operative pain stemming from corneal erosion. We compare the levels of post-operative pain between two groups of patients: 1) those who underwent surgical conjunctival closure with fibrin glue and a fibrin bandage contact lens for corneal erosion, and 2) those with conjunctival closure with Vicryl sutures and exposed corneal erosion.
This prospective study spanned three years at a medical center in Jerusalem, Israel, where a single experienced ophthalmic surgeon conducted all pterygium surgeries. The research adopted a single-center, randomized, prospective, follow-up design within a tertiary medical center in Israel. The primary objective was to compare postoperative pain levels in individuals undergoing pterygium surgery, employing the same surgical technique by closing the defect of the nasal conjunctiva with a flap of healthy supra limbal conjunctiva and without creating an additional wound of the superior conjunctiva by bringing the new superior border of the conjunctiva closer to the superior limbus and two techniques for conjunctival flap anchoring: one group with fibrin glue fixation and second group with Vicryl suture fixation. For first group with fibrin glue anchoring flap was used additional corneal Fibrin glue bandaging.
We studied 90 patients scheduled for elective outpatient pterygium surgery. 50 patients met the inclusion criteria were enrolled in the study. Their informed consent was obtained. All patients were day case patients.
Inclusion criteria were as follows: patient's age between 18 and 85 years, diagnosed with primary nasal advanced pterygium, and undergoing their first pterygium surgery. Patients with collagen diseases, a history of previous corneal surgery, taking drops for glaucoma treatment, with allergic conjunctivitis or pregnant women were excluded from the study.
Prior to surgery, all patients provided informed consent and were thoroughly briefed on the study objectives and procedures. 25 patients underwent pterygium surgery with the usage of fibrin glue flap fixation and corneal wound bandage, while twenty-five patients underwent surgery with Vicryl sutures flap anchoring without corneal wound cover.
The surgical procedure began with the preparation of the eye and surrounding area using Povidone-iodine 5%. Subsequently, a subconjunctival injection of lidocaine HCL 2% and epinephrine 1:100,000 was administered for anesthesia. The pterygium (Figure 1) tissue was separated utilizing lidocaine and epinephrine injection using 30-gauge needle, followed by the precise removal of the pterygium head from the cornea. Pterygium head and adjacent conjunctival and tenon tissue was removed and sent for pathological analysis. Mitomycin-C 0.02% was applied for 90 seconds and thoroughly flushed with more than 200ml of balanced salt saline. Corneal irregularity and some scarring was then excised using a crescent blade and corneal drill. The superior conjunctival flap was prepared (Figure 2,3) and secured to nasal sclera in group 1 using biologic fibrin glue (Figure 4A). After the flap was completely secured to nasal sclera the fibrin glue was additionally applied corneal wound until a clearly defined layer was formed to create corneal fibrin bandage lens. (Figure 5) Alternatively, the conjunctival flap was fixed with single interrupted Vicryl 7-0 sutures (Figure 4B) without corneal wound covering.
Closure was carefully inspected to ensure proper alignment. Of note, in both cases, no superior conjunctival gap was left for secondary wound healing for minimization of additional source of pain. Subconjunctival dexamethasone and gentamicin injection was administered, followed by the application of Sterodex (Dexamethasone Sodium Phosphate 0.1%), Vigamox (Moxifloxacin as HCL 0.5%), Cycloplegic drops (Cyclopentelate hydrochloride 1%) and Synthomycin 5% Ointment (Chloramphenicol 5%). Finally, the eye was closed with patch for 24 hours.

Figure 1. Advanced pterygium of left eye.
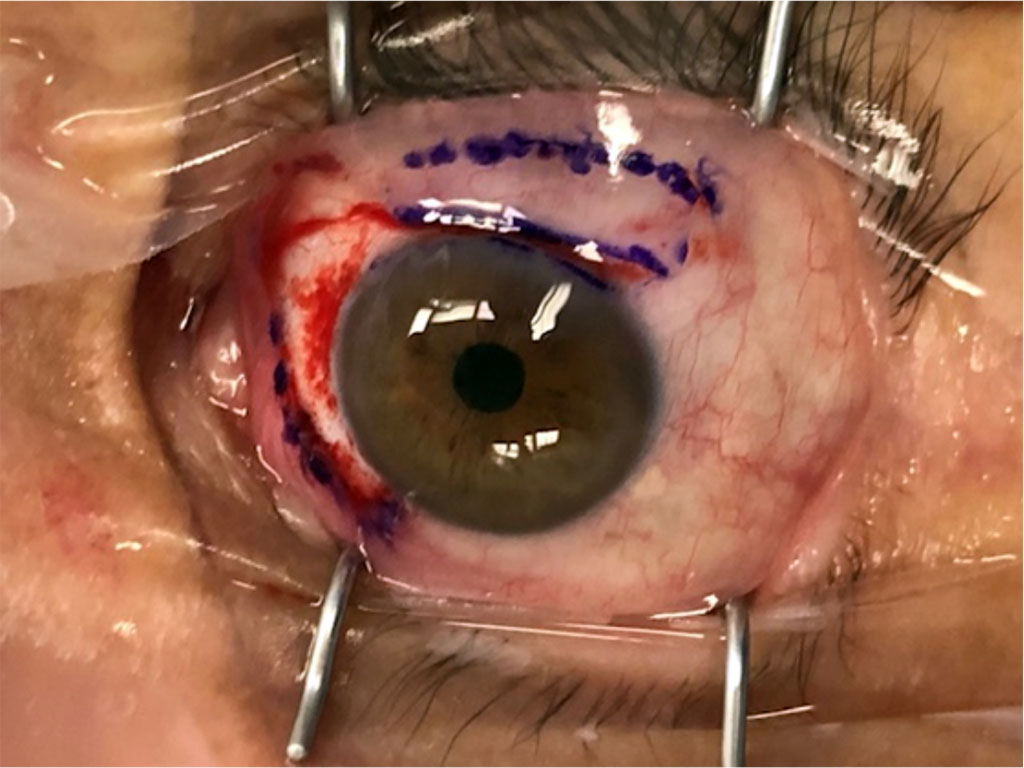
Figure 2. Scleral wound post pterygium removal and superior conjunctival flap planning.
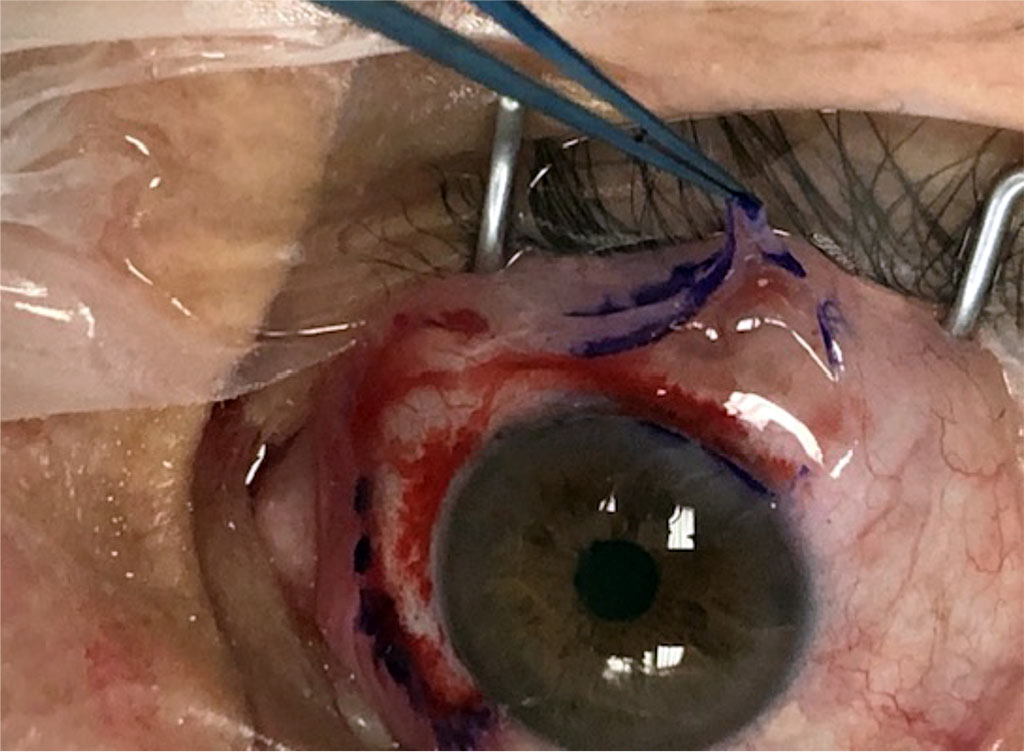
Figure 3. Formation and transposition of superior conjunctival flap.
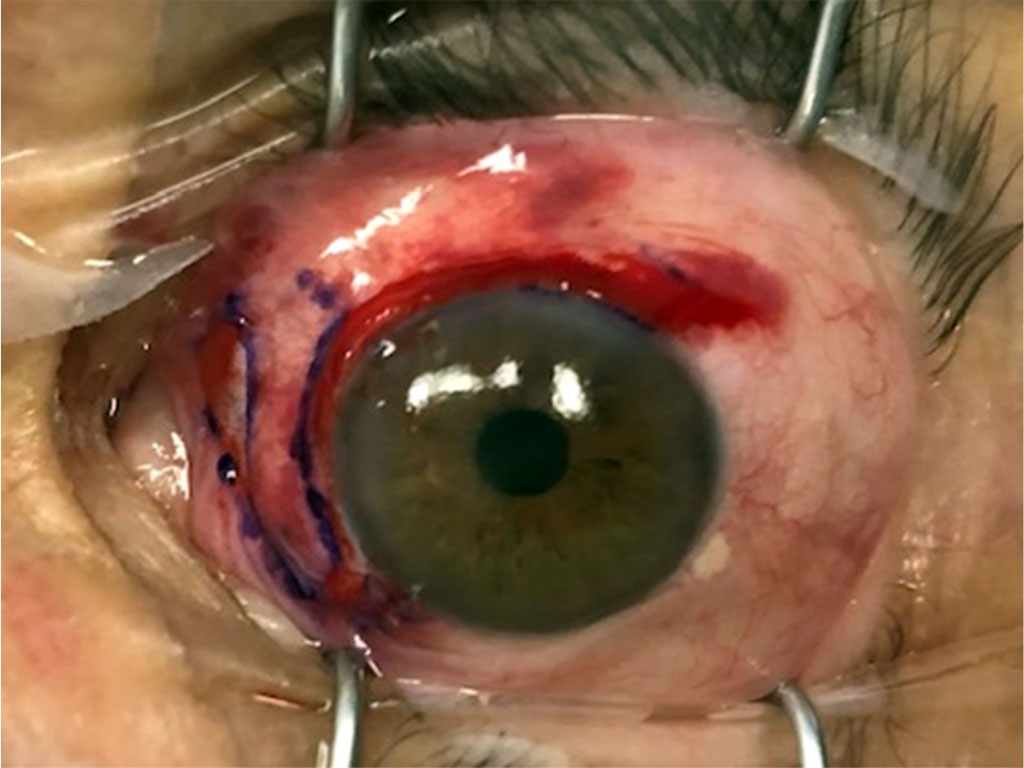
Figure 4A. Fixation of conjunctival flap to limbus and nasal sclera with Fibrin glue.
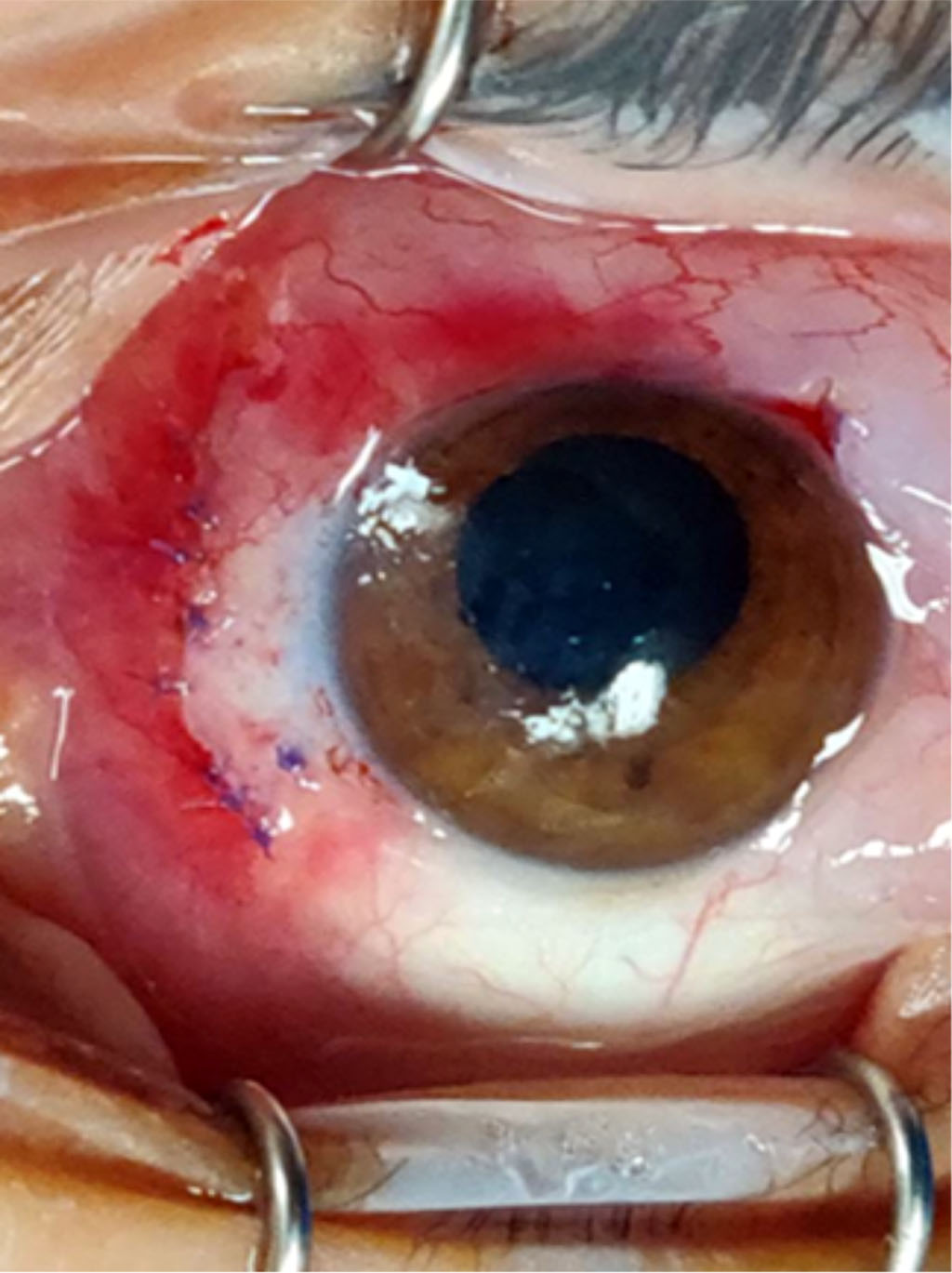
Fig. 4B Fixation of conjunctival flap to nasal sclera with Vicryl sutures.
Both techniques had complete closure of wounds in the supra limbal area.
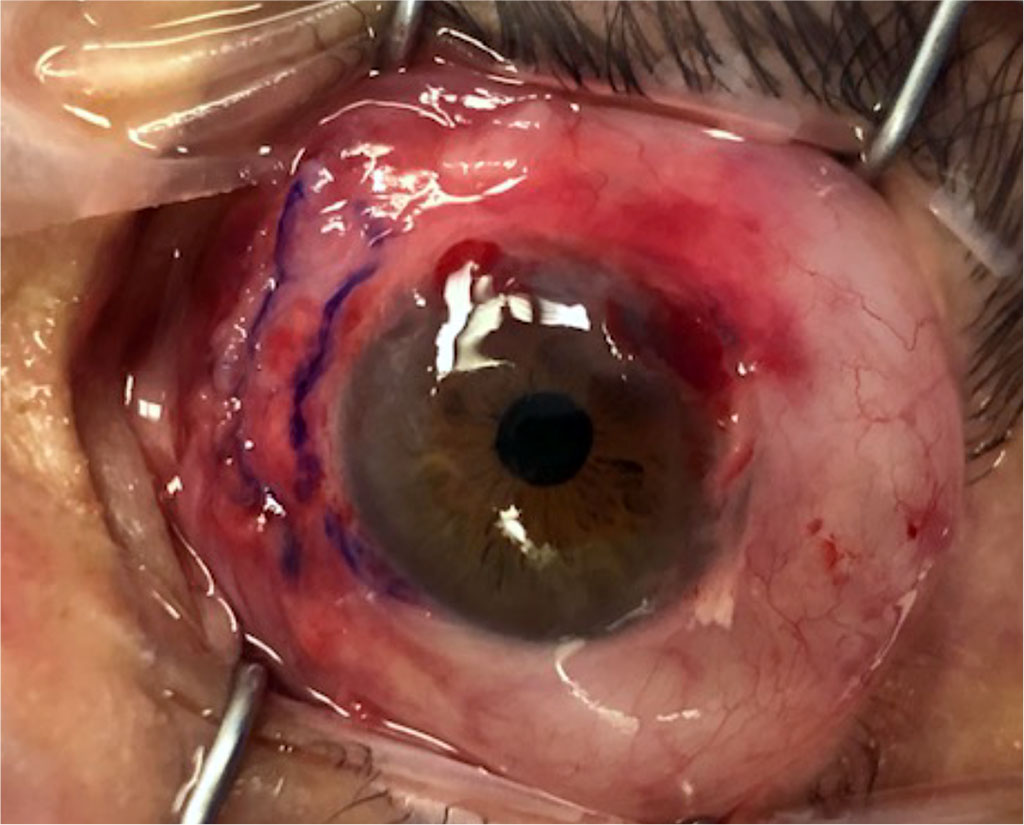
Fig 5 Additional fibrin glue application on corneal surface for Fibrin contact lens formation.
Postoperative pain levels were assessed using a standardized pain scale at specific time points: 24 hours and 7 days after surgery. The pain scale employed a numerical rating system ranging from 0 (no pain) to 10 (worst imaginable pain). Pain assessments were conducted by an independent investigator who was blinded to the surgical technique used.
The questionnaire consists of questions administered on the first day after surgery and one week after surgery. On the first day, Question 1 assesses the peak pain level on a scale of 1 to 10. Question 2 evaluates the level of pain during periods of minimal discomfort, also on a scale of 1 to 10. Question 3 captures the average pain level. At the one-week mark, Question 1 assesses the level of pain during discomfort, and Question 2 evaluates pain during periods of minimal discomfort using the 1 to 10 scale. Question 3 captures the average pain level. This questionnaire enables a comparison of pain levels between the two surgical techniques. Question 4 duration of pain in days from 1 to 7.
We performed a comprehensive statistical analysis to investigate the differences between Fibrin covered surgical corneal wound and not covered surgical corneal wound in pterygium surgery. Firstly, an independent t-test was conducted to examine the potential age difference. Additionally, we compared the gender distribution between the two groups using a chi-square test. For each question in the survey, we assessed the normality assumption using the Shapiro-Wilk test. To evaluate variance discrepancies, Levene's test was employed. Lastly, the Mann-Whitney U test was performed to ascertain significant differences between the two groups at each question. These statistical analyses provided robust evidence for assessing the gender distribution, age comparison, normality assumption, variance discrepancy, and differences between the groups.
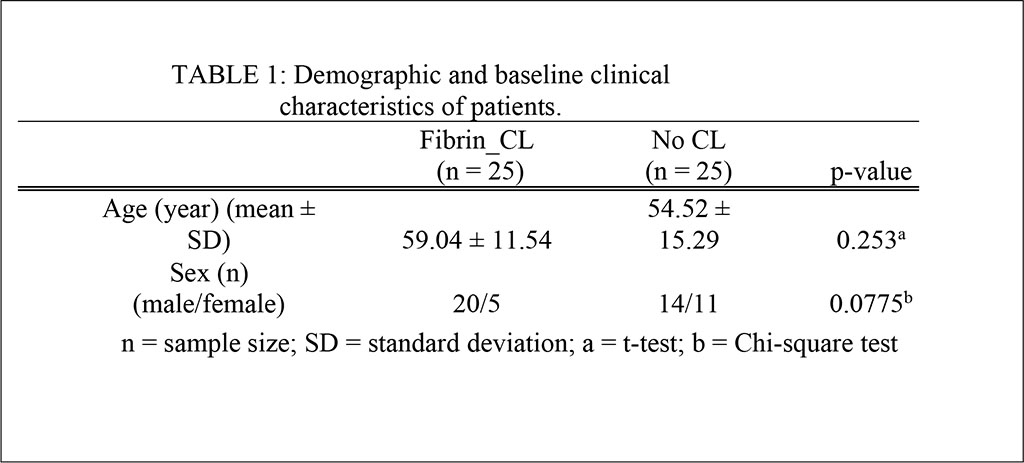
This study comprised 50 consecutive patients who underwent primary pterygium surgery. There were 5 women and 20 men in the fibrin CL group, and 11 women and 14 men in the No CL group. The mean age of the fibrin CL group was 59.04 ± 11.54 years; that of the No CL group was 54.52 ± 15.29 years. There was no statistically significant difference in mean age, sex and size between the 2 groups (p ^ 0.05; Table 1).
At 24 hours post-surgery, the mean maximal pain level was found to be 6.32 in the Fibrin CL group and 6.48 in the Corneal erosion group (No CL Group) (p = 0.496). The mean minimal pain level after 24 hours was 1.40 in the Fibrin CL group and 2.48 in the No CL group (p = 0.36). Similarly, the mean pain level after 24 hours was 3.88 in the Fibrin CL group and 4.40 in the No CL group (p = 0.301).
Upon assessing pain levels after one week, it was observed that the mean maximal pain level was 3.88 in the Fibrin CL group and 5.36 in the No CL group (p = 0.07). The mean minimal pain level after one week was 0.76 in the Fibrin CL group and 0.80 in the No CL group (p = 0.362). The mean pain level after one week was 2.12 in the Fibrin CL group and 3.20 in the No CL group (p = 0.0304), which is significant. Furthermore, the mean duration of overall days of pain within one week was 3.04 in the Fibrin CL group and 4.36 in the No CL group (p = 0.0287), also statistically significant.
These results indicate that while there were slight variations in pain levels between the two techniques 24 post-surgery, the differences were not statistically significant. However, in the pain level 1 week post of was significantly less in the Fibrin CL group as well as the duration of the overall days of pain – both these were statistically significant.
Table 2: Difference between the two treatments on a random shuffled data
| Type | Mean | Median | SD | P-value | |
| 24h-1: max pain | Fibrin_CL | 6.32 | 7 | 3.34 | 0.496 |
| No CL | 6.48 | 6 | 2.87 | ||
| 24h-2: min pain | Fibrin_CL | 1.40 | 1 | 1.52 | 0.36 |
| No CL | 2.48 | 0 | 3.42 | ||
| 24h-3: mean pain | Fibrin_CL | 3.88 | 5 | 2.30 | 0.301 |
| No CL | 4.40 | 4 | 3.00 | ||
| 1w-1: max pain | Fibrin_CL | 3.88 | 5 | 3.05 | 0.07 |
| No CL | 5.36 | 6 | 3.50 | ||
| 1w-2: min pain | Fibrin_CL | 0.76 | 0 | 1.20 | 0.362 |
| No CL | 0.80 | 0 | 1.50 | ||
| 1w-3: mean pain | Fibrin_CL | 2.12 | 2 | 1.83 | 0.0304 |
| No CL | 3.20 | 3 | 2.10 | ||
| 1w-4: pain time | Fibrin_CL | 3.04 | 3 | 2.35 | 0.0287 |
| No CL | 4.36 | 4 | 2.38 |
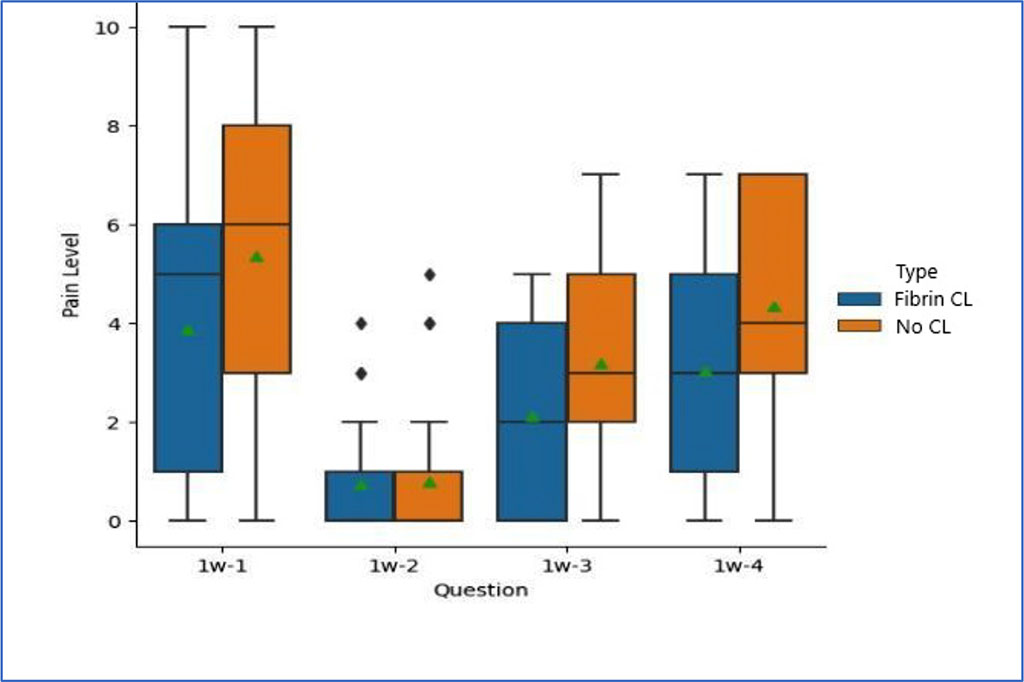
Figure 6. Comparison of pain levels during 1 week: 1 maximal pain, 2 minimal pain, 3 mean pain, 4 pain time.
Fibrin glue serves as a biological tissue adhesive that mimics the concluding phases of the coagulation cascade. This occurs by activating a solution containing human fibrinogen with thrombin, which are the two components of fibrin glue. Ever since the introduction of fibrin glue in ophthalmology, its major use has been in pterygium surgery (1).
The primary long-term goal of pterygium surgery is the excision of the pterygium with a focus on preventing its recurrence (5). A diverse array of surgical techniques are currently employed for this objective, ranging from the conventional bare sclera procedure to advanced methodologies, including amniotic membrane transplantation, resection with autologous stem cell transplantation, and lamellar keratoplasty (6).
Post-operative recovery is often accompanied by significant pain, especially during the first post-operative week, and is a great source of patient discomfort (7). A component of post operative pain is due to the corneal erosion caused during surgery, before full wound epithelialization is achieved. Similar pain due to corneal erosion has been shown to respond well to tight bandaging, such as with a bandage contact lens (8).
In our solution this bandage serves a dual purpose by not only stabilizing the conjunctival flap and shielding the conjunctival wound but also by extending its coverage to encompass areas of corneal erosion. This comprehensive approach addresses the unique challenges associated with corneal erosion, providing an additional layer of protection and support during the critical healing phase. The use of fibrin glue in this manner represents a significant advancement in pterygium surgery, offering a comprehensive solution for flap stability and corneal care, potentially improving surgical outcomes and patient comfort.
We examined a technique of bandaging the resulting corneal erosion following pterygium removal with conjunctival flap which makes use of application of fibrin glue to the corneal erosion. This technique forms a temporary barrier between the exposed de-epithelialized cornea and the environment that dissolves as the epithelial layer heals by adjusting the thickness of the fibrin glue contact lens by varying the number of drops of glue applied. In closure using fibrin glue, addition of this stage necessitates minimal additional time and cost to the surgery.
In this pilot study, patients presenting for pterygium surgery were randomized to conjunctival wound closure with either sutures and without corneal wound closure or to conjunctival wound closure with fibrin glue and fibrin bandaging of corneal erosion. We believe that the main source of patient pain is the resulting corneal erosion and not the healing conjunctival wound. When closing the conjunctival wound the fibrin glue often leaks onto the cornea therefore forming a defacto partial fibrin bandage contact lens. In order to circumvent this problem and to isolate the corneal pain difference, we chose to compare suture closing of conjunctival wound vs fibrin glue with a bandage contact lens. In addition, the use of absorbable sutures on the conjunctival flap do not contribute additional pain just possible minor discomfort. In our study we evaluated a pain which shouldn’t be affected by suture discomfort. Patient in both treatment groups were similar in age and sex. In patients treated with fibrin bandaging, the mean pain level after one week was 2.12 and 3.20 in the No CL group (p = 0.0304). Furthermore, the mean duration of overall days of pain within one week was 3.04 in the Fibrin CL group and 4.36 in the No CL group (p = 0.0287).
In conclusion, the outcomes of this study propose that employing fibrin glue as a bandage for corneal surgical wounds in pterygium surgery is associated with diminished pain levels and a shorter overall duration of pain when compared to the use of closure only conjunctival wound and leaving the corneal wound uncovered. Importantly, no surgical complications, such as wound dehiscence or infection, were identified in either group. While these findings are promising, it is imperative to acknowledge the need for further investigations with larger sample sizes and extended follow-up periods to validate and comprehensively explore the factors contributing to the observed differences. In future studies we need to explore fibrin contact lens closure vs treatment contact lens in the suture group and expand the questionnaire to include extra parameters including discomfort. This will contribute to a more robust understanding of the potential benefits and implications of utilizing fibrin glue in conjunctival wound closure during pterygium surgery.
This study adhered to the principles outlined in the Declaration of Helsinki and received ethical approval from the institutional review board of the medical center. Patient confidentiality was strictly maintained, and all data were anonymized and securely stored.
None.
No conflicting relationship exists for any author.