- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Gonarthrosis is one of the topical orthopedic problems. One out of three all orthopedic patients are affected by knee osteoarthritis. Multiple studies demonstrate that this condition occurs most frequently in working-age population. Having studied the results of surgical treatment in 324 gonarthrosis patients, we have elaborated a differentiated approach to knee arthroplasties. A unicondylar arthroplasty is expedient for young patients; if flexion contracture of a knee exceeds 15°, we recommend a PLC non-preserving prosthesis; if a lesion of a tibial process exceeds 10 mm, we used a prosthesis with a tibial extensor; for total instability of knee, we used hinge-type constrained modifications of prostheses.
Keywords: gonarthrosis, endoprosthesis, tibial extensor, knee joint
Deforming arthritis is one of most topical and complex orthopedic problems. One third of all orthopedic patients suffer from the deforming arthritis. Multiple studies have shown, that these conditions occur most frequently in active age people, namely 40-60 years old [1, 2]. In Ukraine, osteoarthritis affects almost 500 people per 100 thousand of population [1, 4]. Most often, the pathology occurs in “loaded” joints (hips and knees). According to its incidence, arthritis of a knee (gonarthrosis) leads the group of degenerative and dystrophic joint diseases [3, 4, 5]. By the severity of its progression, it is in second place after coxarthrosis. One out of five people in the world suffer from gonarthrosis. Its occurrence in women is twice higher than in men. Statistically, 7-22% of the world population has gonarthrosis. Gonarthrosis (deforming arthritis, osteoarthritis, degenerative arthritis, or hypertrophic arthritis) is a poly-etiological degenerative-dystrophic disease, typical of damage to articular cartilage, subchondral, and metaphyseal bone, synovial membrane, ligaments, capsule, muscles, accompanied with bone-cartilage proliferations. It is expressed with pain and restricted range of motions of the affected joint. Gonarthrosis progression leads to the development or exacerbation of knee deformity in 32-65% of patients. This is a frequent cause of such patients’ disability. In early stages of the disease, various therapies are expedient, as conservative, as surgical [6, 9, 10]. In later stages, as pain and restriction of motions grow, knee arthroplasty is becoming more and more expedient for gonarthrosis treatment.
Objective: to develop a differentiated approach to knee arthroplasty, depending on the severity of damage to the joint in patients with III-IV stages deforming gonarthrosis according to Kellgren-Lawrence classification [7].
Within 2010-2017, we carried out 324 knee arthroplasty surgeries in gonarthrosis patients. Age of the patients was 62±14 years old; 82.5% of them were women, and 17.5% - men. In 6 cases, there was a total knee arthroplasty to both knee joints.
Clinically, the patients claimed for constant pain in knee area, going worse under the physical loading. The majority of patients suffered from flexion knee contracture 0-0-90±15. In 204 cases, we observed a varus knee deformity, while in 21 cases – a valgus one. In all the cases, there were significant radiological changes. Joint gaps were sharply narrowed and almost disappeared between the femoral and patellar surfaces. In addition, there was tibial medial process destruction, edge bone excrescences along the periphery of femoral, tibial, and patellar bones.
Choosing for a type of endoprosthesis in gonarthrosis patients, we have considered the following factors:
Depending on these factors, the patients underwent following surgical interventions: a unicondylar arthroplasty, a PCL-preserving and non-preserving total arthroplasty, a total knee arthroplasty with a tibial extensor, and an arthroplasty with a constrained hinge-type endoprosthesis (Table 1).
Table 1. Patients according to the type of surgery
| Type of the surgical operation | Men | Women | Total |
| Unicondylar knee arthroplasty | 6 | 11 | 17 |
| Total knee arthroplasty (СR) | 32 | 151 | 183 |
| Total knee arthroplasty (СR) with a tibial extensor | 0 | 3 | 3 |
| Total knee arthroplasty (LPS) | 17 | 96 | 113 |
| Total knee arthroplasty (LPS) with a tibial extensor | 1 | 3 | 4 |
| Total knee arthroplasty with a constrained hinge-type endoprosthesis | 1 | 3 | 4 |
| Total | 50 | 253 | 324 |
In gonarthrosis cases of the 2nd -3rd stage complicated with an aseptic necrosis of a femoral medial process in patients under 60 years old, a unicondylar knee arthroplasty was performed.
For those, whose flexion contracture of the knee did not exceed 10 degrees, we carried out a total knee arthroplasty, PCL preserved.
If the knee flexion contracture exceeded 10 degrees, we implanted a total endoprosthesis without preservation of PCL, using the extramedular technique and cement fixation of the prosthetic components.
In cases of any tibial process defect (varus or valgus knee deformity), we applied a tibial extensor. To replace the defects, we used bone autograft or augment, depending on the lesion’s size.
Upon conditions of a complete lateral knee stabilizers’ incompetence, we replaced the knee joint with a constrained hinge-type endoprosthesis.
Principal tasks of total knee arthroplasty were to recover an extremity’s biomechanical axis and to implant the components correctly. During the early post-surgical period, we used an adequate pharmaceutical pain management, prevention of infectious complications with broad-spectrum antibiotics for 5-7 days; introduced low-molecular heparins during the first week after the intervention. The active-passive motions of the joint started in 1-2 days after the operation; we recommended walking with crutches, loading the operated limb with 25% of the body weight 3-4 times a day; in two months, the patients were allowed to load the operated limb completely.
The patients involved to this study have given their informed consent.
The observation over the operated patients lasted from 1 to 9 years after the surgery. To evaluate the outcomes, we have elaborated a score-based system for the assessment of the functional conditions of a knee (Table 2) based on the defining of workability criteria, extended with an Lequesne Algofunctional Index [9] (Table 3). Evaluating outcomes, we have considered 7 signs (criteria), giving 3, 2 or 1 score to each. This system covers following criteria: the patient’s personal assessment of his/her knee, pain, range of motions, weight bearing capacity, flexion contracture, lameness, knee deformity in a frontal plane.
Table 2. The system to assess the gonarthrosis patients’ outcomes
| Criteria | Scores | ||
| 3 | 2 | 1 | |
| Subjective evaluation of the conditions of the joint by a patient | Good | Satisfactory (reported insignificant distortion of the limb’s functions) | Poor (significant distortion of the functions of the limb) |
Pain |
No pain | Moderate pain during physical loading | Constant pain |
| Range of motions | Over 90° | Over 80° | Less than 80° |
| Flexion contracture | No flexion contracture | Under 10° | Over 10° |
| Weight bearing capacity | Preserved | Distorted moderately | Distorted significantly |
| Lameness | No lameness | Moderate lameness | Expressed lameness |
| Varus (valgus) deformity of the knee | 0–50 |
60–100 |
Over 100 |
We construed the total amount of 18-14 scores as a good result, 13-10 as a satisfactory, and 9-6 as a poor one. The cases of early or remote suppuration demanding the repeated surgery, including the removal of the prosthesis we registered as poor results.
The total knee arthroplasty without PCL preservation has demonstrated good results in 84% and satisfactory ones in 16% among 113 patients. After the knee arthroplasty with PCL preservation, there were 54% of good and 46% of satisfactory results among 183 gonarthrosis patients. In our opinion, it could be explained by underassessment of a knee flexion contracture at the stage of choosing the endoprosthesis system (Table 3).
Table 3. Lequesne Algofunctional Index for gonarthrosis
| Criteria | Scores | |
| 1 | 2 | |
| Pain or discomfort | ||
| Pain in the night | ||
| Only in a specific position Even at rest | 1 2 | |
| Morning stiffness or pain after sleeping | ||
| Less than 15 minutes Over 15 minutes | 1 2 | |
| Pain occurs while walking | ||
| Only after walking to a specific distance Appear at once and later becomes stronger | 1 2 | |
| 2. Maximum painless walking distance | ||
| Over 1 km with a rest About 1 km From 500 to 900 m From 300 to 500 m From 100 to 300 m Less than 100 m With a single cane or crutch With two canes or crutches | 1 2 3 4 5 6 +1 +2 | |
| 3. Restrictions of regular daily activities | ||
| Can you climb one flight of stairs? Can you get down one flight of stairs? Can you put something on a wardrobe’s lowest shelf, staying on your knees? Can you walk an uneven road? Do you experience a shooting pain or sudden feeling that you lose the ill extremity’s support? sometimes frequently | 0–2
0–2 0–2 0–2 1 2 |
|
If the sum total of the scores was within 21 – 17, Lequesne Algofunctional Index (LAI) from 1 to 5, we took this as a good result; scores from 17 to 10 and LAI from 6 to 8 meant satisfactory, and less than 9 scores and LAI 9 and more – a poor one (Table 4).
Table 4. The knee arthroplasty with (CR) and without (LPS) the posterior crucial ligament preservation
| Results (scores) | Prosthesis of a knee joint | Total (persons) | |
| LPS, pers. (%) | CR, pers.(%) | ||
| Good
(21-17) LAI (1-5) |
95 (84%) | 98 (54%) | 193 |
| Satisfactory
(17-10) LAI (6-8) |
18 (16%) | 80 (46%) | 98 |
| Poor
( ≥ 9 ) LAI ( ≥ 9) |
0 | 5 | 5 |
| Total | 113 | 183 | 296 |
Having applied a tibial extensor, we have observed good outcomes in 84% of patients after LPS and in 54% - after CR surgery. This could be explained by wider options LPS system provides to correct varus deformities and flexion contractures (Table 5).
Table 5. The use of tibial extensors while CR (PCL-preserving) and LPS (non PCL-preserving) total knee arthroplasty
| Results (scores) | Total knee endoprosthesis with a tibial extensor | Total (persons) | |
| LPS, pers. | CR, pers. | ||
| Good
(21-17) LAI (1-5) |
4 | 3 | 7 |
| Satisfactory
(17-10) LAI (6-8) |
0 | 0 | 0 |
| Poor
( ≥ 9 ) LAI ( ≥ 9) |
0 | 0 | 0 |
| Total | 4 | 3 | 7 |
Having applied a tibial extensor for total knee arthroplasty, we have observed good outcomes in 100% of patients. Results were good in all the patients after the total knee arthroplasty with a constrained hinge-type endoprosthesis
In general, good outcomes were observed in 65% (210 persons) of arthroplasty cases. The patients felt good: no pain, no laming, recovered regular range of motions, no joint deformity, correct limb axis, stable joint. X-ray revealed the correct placement of prosthetic components, no signs of instability. In 35% (114 persons), the results were satisfactory: the patients felt good, no pain, a moderate laming, restriction of the range of motion did not exceed 80o, no join deformity, stable joint. X-ray showed that position of the prosthetic components was correct, without any signs of instability.
We had no poor results.
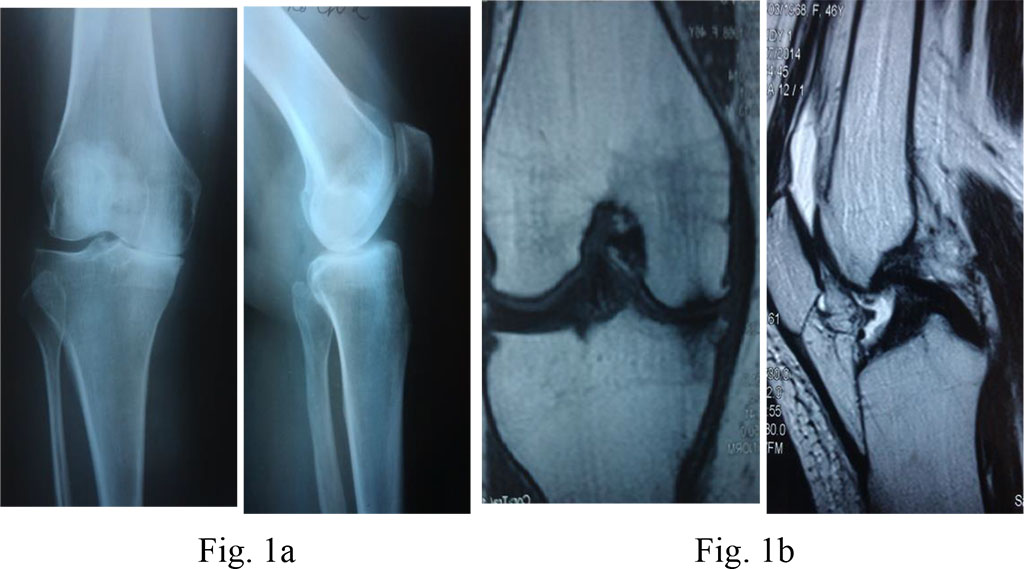
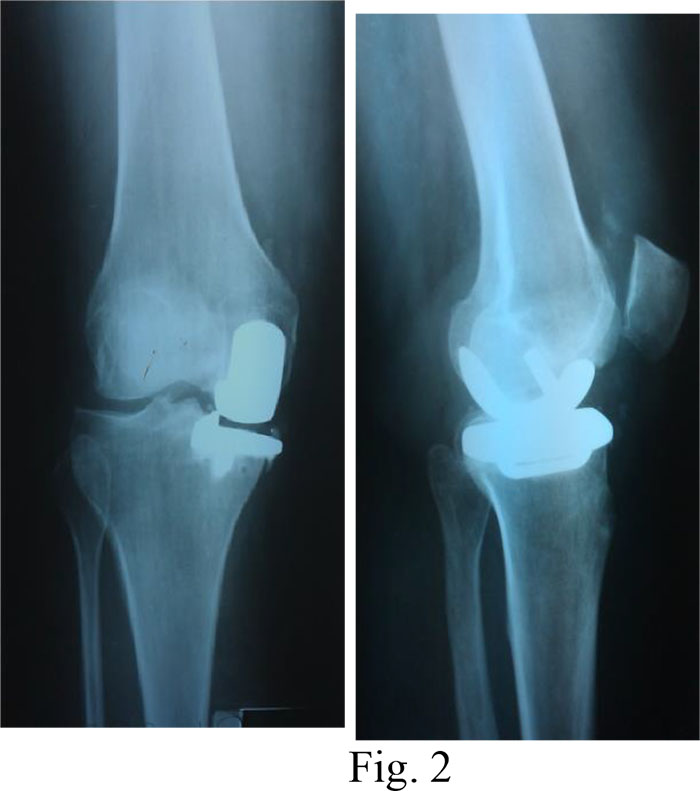
Diagnosis: III stage deforming arthritis of the left knee; varus deformity of the left knee; aseptic necrosis of the left femur’s medial process; pain syndrome.
Surgical treatment: a unicondylar arthroplasty of the left knee (Fig. 1a, b and 2)
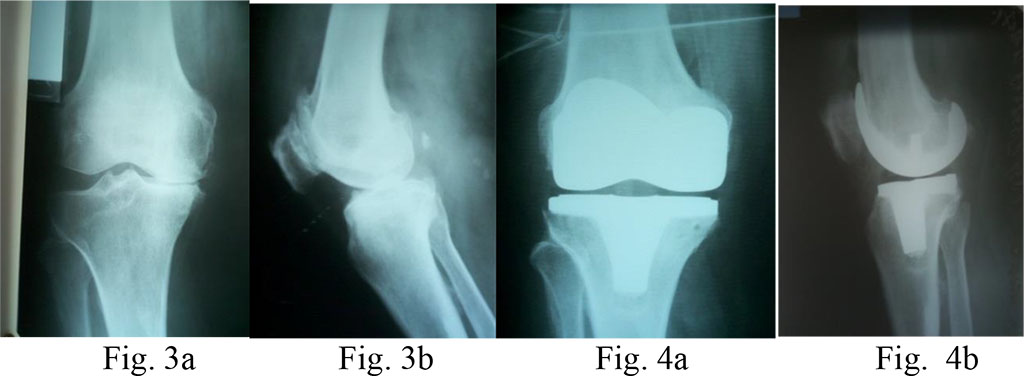
Diagnosis: knee osteoarthritis on the right, IV stage according to Kellgren&Lawrence (1957); varus deformity of the joint; expressed pain syndrome.
Surgical treatment: total arthroplasty of the right knee with PCL-preserving system (Fig. 3a, b and 4a, b)
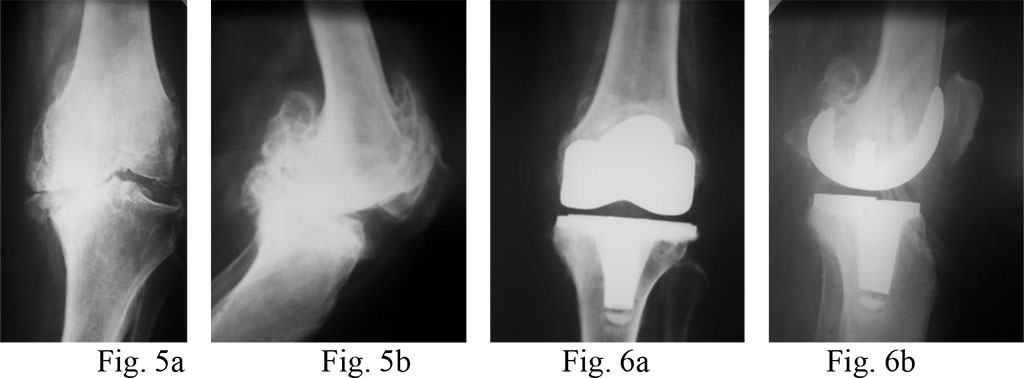
Diagnosis: knee osteoarthritis on the left, IV stage according to Kellgren&Lawrence; varus deformity of the joint, 15o flexion contracture of the left knee.
Surgical treatment: total arthroplasty of the left knee with an LPS prosthesis (without preservation of the PCL) (Fig. 5a, b and 6a, b)
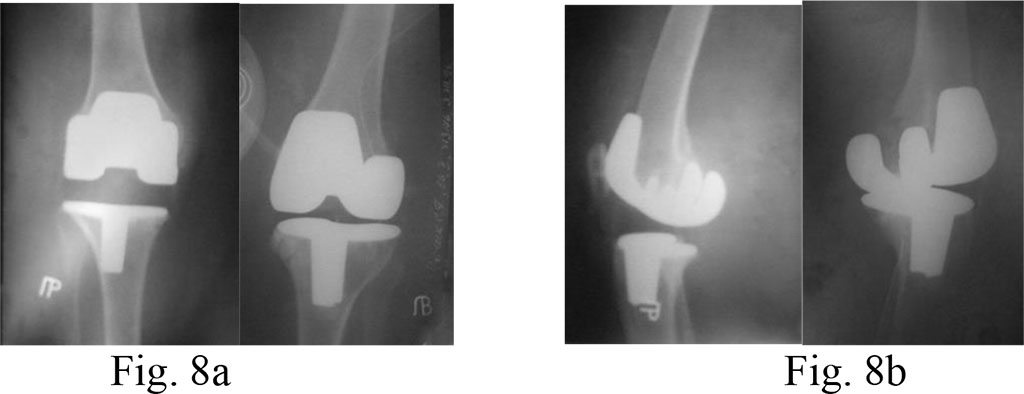
Diagnosis: bilateral deforming gonarthrosis stage 4; varus deformities of both knees.
Surgical treatment: bilateral total knee arthroplasty with PCL preservation.
On the right, we carried out tibial resection on the level of the lower edge of the defect and applied a large tibial insert (21 mm). On the left, resection of the tibial bone was on the level of the upper edge of the lesion, than filled with bone cement and a tibial insert of a minimal size (9 mm) (Fig. 7a, b and 8a, b)

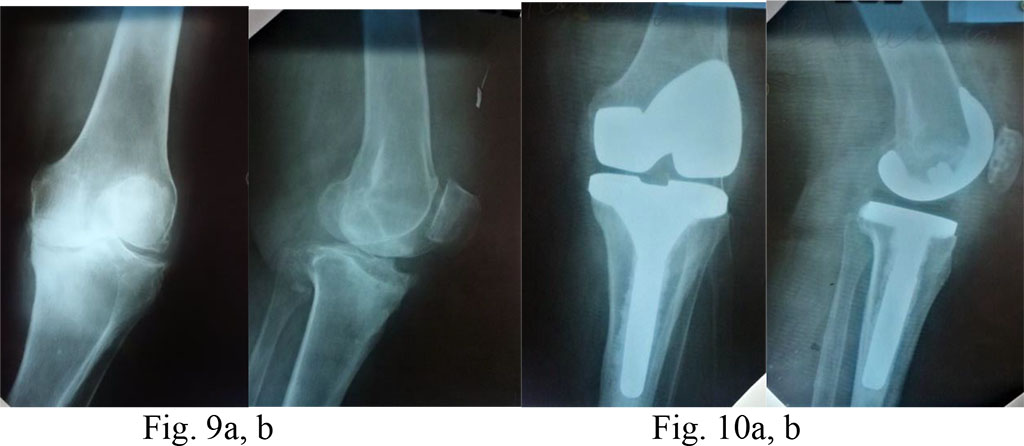
Diagnosis: knee osteoarthritis on the left, stage 4 according to Kellgren&Lawrence (1957); a posttraumatic lesion of the medial tibial process; varus deformity of the joint; expressed pain syndrome.
Surgical treatment: total arthroplasty of the right knee with an extended tibial component, CR method (PCL preserved) (Fig. 9a, b and 10a, b)
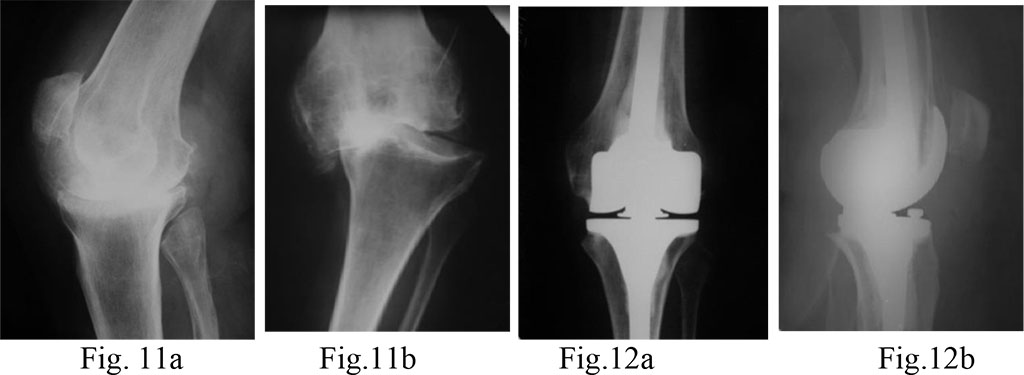
Diagnosis: a posttraumatic gonarthrosis stage 4 on the left; varus deformity of the left knee; the frontal instability; complete lateral knee stabilizers’ incompetence.
Surgical treatment: total knee arthroplasty on the left with a constrained hinge-type endoprosthesis (Fig. 11a, b and 12a, b)