- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Aim: To justify the choice of a method for fixing unstable proximal tibial fractures (PTF), to conduct computer simulation of stresses on various metal fixators.
Materials and Methods: at the initial stage, a solid 3D model of the lower leg has been created using Solid Works, on the background of anatomical models and CT scans. The model contained the following elements: tibia and fibula, interosseous membrane, ligaments of the proximal and distal tibia syndesmosis, and a modeled proximal tibial fracture. We have subsequently studied 4 models of bone fragments’ fixation with LCP plates and an intramedullary blocking metal rod. Further calculations were performed using the finite element method.
Results: computer simulations of stresses on various metal fixators applied to fix a PTF convincingly proved that blocked intramedullary osteosynthesis (BIOS) and LCP plates placed bilaterally are feasible for this category of patients.
Conclusions: Deformities and loads observed in the metal fixator, bone tissue and ligamentous apparatus run within normal limits. They are statistically significantly (p ≤ 0.05) lower in models of bone fragments’ fixation with IM nailing and bilaterally placed LCP plates. This evidences the adequate stability of bone fragments’ and these methods of osteosynthesis as a whole, compared to the stains in the same elements of modelled fixation using only one plate – medially or laterally.
The results of the study may serve as the background for the development of an algorithm for surgical treatment and rehabilitation of patients with PTF.
Keywords: computer modeling, proximal tibial fractures, tension, metal clamps
Proximal tibial fractures (PTF) are severe lower limbs’ injuries. The share of PTF in all skeleton fractures makes from 2% to 5%. [5]. For a modern orthopedic surgeon, PTF treatment is a challenge due to its complex cinematics and peculiarities of knee joint’s structure (the absence of a significant muscle mass, close placement of major vessels and nerves) [6, 8]. Its topicality is predetermined by high frequency of poor functional outcomes. Not rarely, deforming osteoarthritis, contractures, knee instabilities occur in a distant period after the trauma, namely in 5.8% to 28%, of cases. At that, recognized invalidity reaches 5.9-9.1% [1, 7]. Due to these factors, it is medically and socially essential task for the modern traumatology: to find the most efficient way to treat this disorder.
There are various methods for surgical treatment for PTF. Locking intramedullary osteosynthesis (intramedullary nailing) is a generally-accepted “golden standard” for extra-articular fractures, surface plates and screws [6]. However, having analyzed literature sources dedicated to PTF we have discovered, that there is lack of a common opinion regards the use of a certain metal fixator for this category of patients. For instance, IM nailing can serve for the surgical treatment of PTF (41-А2, 41-А3, 42 according to AO) [6]. However, there are descriptions of the cases of a successful IM nailing after simple intraarticular fractures (41-С1 і 41-С2) [9, 10]. Discussed is the expediency of the use of one or two superficial plates for the osteosynthesis in this category of patients [5, 12]. Simultaneously, there are attempts to substantiate the fitness of metal implantable devices on the backgrounds of the knowledge about human systems’ biomechanics. At that, most frequently calculations accept approximate schemes reflecting key aspects of “bone-implant” system’s behavior using software realization of numeric methods line the method of finite elements. On the grounds of the calculations’ results, we make conclusions on the work of an implants and its influence on the bone to refuse from developing vividly hopeless constructions. They enable us to correct and change shapes of an implant’s components to improve its functionality. The need in numeric animal tests disappears; the time and costs required to develop an implantable device drop significantly; an accurate forecasting of remote results becomes possible on the background of the deforming strains distribution [3, 11].
Therefore, we consider it scientifically and practically interesting to carry out a computer-aided modelling of strains in different metal fixators upon conditions of proximal tibial fractures – hence, objective of the research.
The biomechanical study took place at the Laboratory of Biomechanics of the SI “ITO NAMS of Ukraine” headed by Lazariev I.A. At the initial stage, a solid 3D model of a shin has been created using anatomic model data and CT scans with means of Solid Works. It contained the following elements: tibia, fibula, interosseous membrane, ligaments of a proximal and distal syndesmosis, and a reproducible proximal tibial fracture according to a scheme (Fig.1). Afterwards, they created 4 models of bone fragments’ fixation using LCO plates and an intramedullary metal rod (Fig.2).
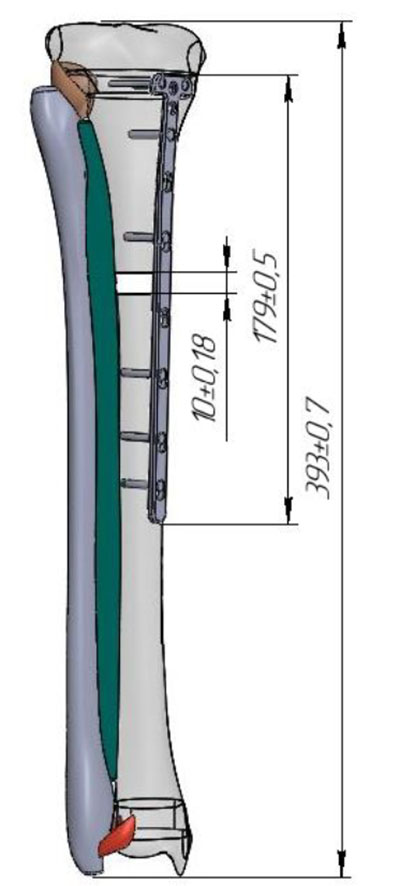
Fig.1. The solid 3D model of a shin
The next stage indicated boundary values of the model’s fixation and load with a body weight, corresponding to an average statistical body weight of 75 kg (750N). The created model included 381.787 nods and 206.583 elements. Next calculations applied the finite elements method (FEM). To calculate the strain-deformed conditions (SDC) using the FEM method, we have chosen Ansys software complex by ANSYS Inc. [3, 11].
The calculations considered physical characteristics of bone tissue, obtained from literature sources [2]. We calculated SDC by FEM method for all 4 proposed models:
Model 1 – an LCP plate on the medial surface of a tibia;
Model 2 – an LCP plate on the lateral surface of a tibia;
Model 3 – two LCP plated – on medial and lateral surfaces of a tibia;
Model 4 – an intramedullary locking nail.
For statistic studies, we used Statistica - 6.0 software package [4].
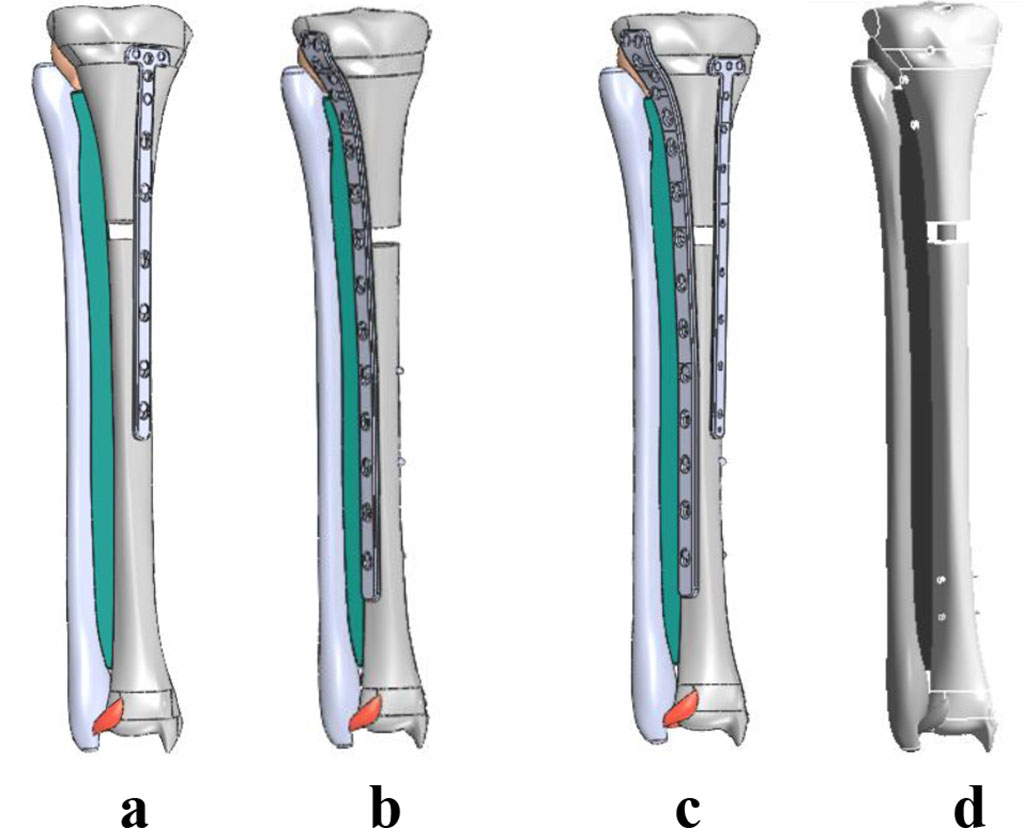
Fig.2. Models of bone fragment’s fixation methods using LCP plates: unilaterally, on a tibia bone’s medial surface - model 1 (a), unilaterally, on a tibia’s lateral surface – model 2 (b); bilaterally – model 3 (c), and the model with an IM nail – model 4 (d).
The aggregate values of the models' SDC appear on the Table 1 and Fig. 3.
Analysis of the obtained SDC values for loading with a body weight, as arranged in the Table 1 and Fig.3, demonstrate that strain distribution is more uniform for an intramedullary locking nail (model 4), where the strain in the metal fixator, bone tissue, and ligament apparatus run within normal values and is statistically significantly (р ≤ 0.05) lower than the strains in the elements of the models 1 and 2. At that, deformity values of the model are insignificant and statistically significantly (р ≤ 0.05) lower, compared to the deformity values of the models 1 and 2. This evidences adequate stability of fragments and the method of osteosynthesis as a whole. The shift of the model in the case of IM nailing is stipulated by structural specificity of the “nail-bone” system and promotes reparative osteogenesis.
Table 1. Strain-deformed condition values of the models
| Bone fragments’ fixation variant | The model’s element | Deformation
of the model, mm |
Displacement of the model, mm | ||||
| tibia, MPa | metal fixator, MPa | fibula, MPa | interosseous membrane, MPa | ligaments, MPa | |||
| Model 1 | 26.90 (15.12) | 1095.2 | 11.95 (7.21) | 12.89 | 0.03 | 0.05 | 2.53 |
| Model 2 | 49.18 (12.53) | 880.56 | 29.31 | 14.73 | 0.05 | 0.06 | 2.66 |
| Model 3 | 29.99 (7.28)* | 382.0* | 11.4 (4.09) * | 5.94* | 0.03 | 0.02* | 1.41* |
| Model 4 | 60.09 (6.02)* | 250.4* | 11.54 (4.32) * | 4.76* | 0.44 | 0.03* | 2.47 |
Note. 1. Values in brackets – according to the strain scale, except for its concentration (basic values); 2. *– the values demonstrate significant statistical difference (р≤0.05) compared to the same for the model 1.
The situation was similar for the bilateral use of LCO plates (model 3), however SDC values for the bone and metal structure were insignificantly higher. Strain in the metal fixator, bone tissue, and ligament apparatus remain within normal values and are statistically significantly (р≤0.05) lower compared to the same of the models 1 and 2. The values of general displacements (Total Deformation) and the models’ deformations are also insignificant, statistically reliably (р≤0.05) than the deformities in models’ 1 and 2 elements. This evidences adequate stability of fragments and the method of osteosynthesis in general.
The use of an LCO plate unilaterally – on medial or lateral surface of a tibial (model 1 and 2) don’t ensure stable fragments’ fixation. The strains in the bone and ligament apparatus significantly exceed the margin of strength. This may lead to breakage of fixators and slower bone consolidation. The values of total displacements (Total Deformation) for the models 1 and 2 equal 2.53 and 2.657 mm. For this type of osteosyntheis, it could be a significant factor for the development of reparative osteogenesis disorders.
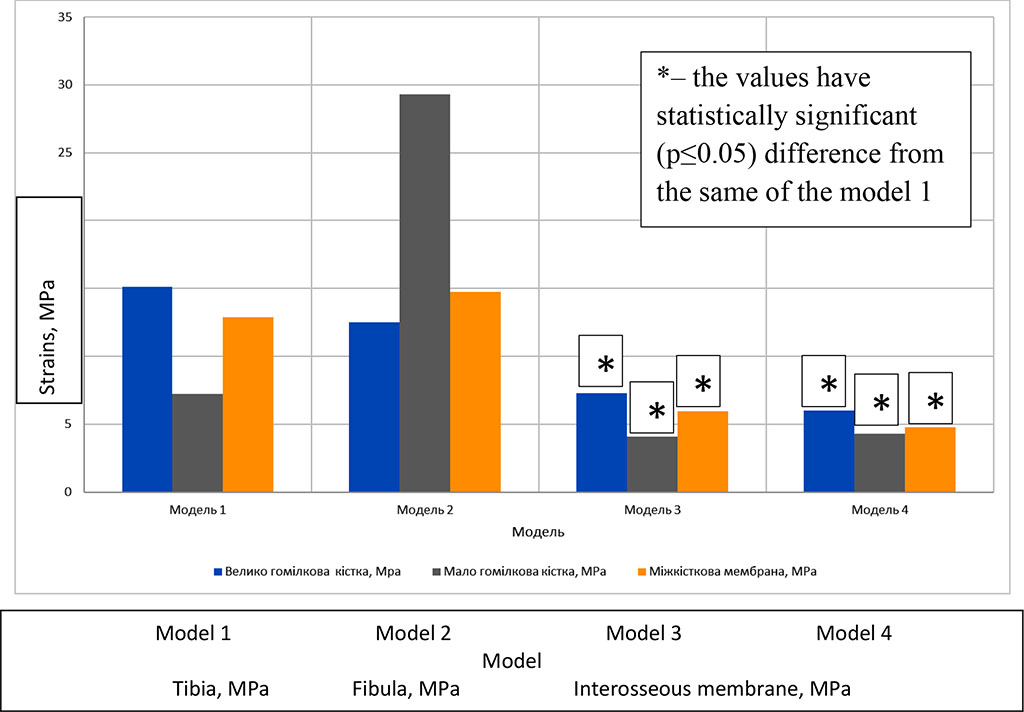
Fig. 3. Comparative characteristics of SDC values for every model
Thus, computer-aided modelling of strains in different metal fixator used to fix a PTF has convincingly proved the expediency of IM nailing and LCP plates, if used bilaterally for this group of patients.
The computer-aided simulation of the strains in different metal fixators (LCO plates used unilaterally medially or laterally, bilaterally, and IM nailing) for PTF fixation evidences, that:
The results could serve as a background to an algorithm for surgical treatment of PTF patients.
Within the task from the scientific and research program of The Institute of Traumatology and Orthopedics of Ukraine: “To elaborate a tactics for surgical treatment of a ship post-traumatic osteomyelitis depending on the extent of expression of trophic disorders”0117U003012, years 2018-2020.
The authors have no conflict of interest to declare.