- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
The authors analyzed the case histories of 3 954 patients aged 15–86 years with varying degrees of neurological deficit who had received treatment from 2010 to 2020 in the city neurology department. All patients underwent general clinical and neurological examinations, electrocardiography, clinical laboratory and biochemical tests and, of course, the classical Wasserman test. In addition, ophthalmological, immunological, neurophysiological, neuropsychological and radiological studies were performed. We present a clinical example of early meningovascular neurosyphilis against the backdrop of right hemispheric cerebrovascular accident (CVA). Difficult diagnosing due to the bias of data on CVA, the peculiarities of the disease course and the cumulative neuroimaging data allow the authors to assume a clear dependence of meningovascular syphilis of the nervous system on constitutional variations and/or anomalies of the arteries of the circle of Willis. Constitutional variations and/or anomalies in the development of human cerebral arteries are considered as an additional risk factor for CVA syndrome during infectious processes of the brain with other things being equal.
Keywords: cerebrovascular accident, syphilis, cerebrovascular neurosyphilis, cerebral arteries, cerebral stroke, anomalies of the cerebral arteries, differential diagnosis
According to WHO, in 2020, 7 million new cases of syphilis infection were registered worldwide [1]. An even more urgent problem of modern medicine is vascular lesions of the central nervous system. Every year, 15 million people worldwide suffer a stroke. Of these, 5 million die, and another 5 million remain permanently disabled, which puts a strain on the family and society [2,3].
Currently we can also observe some new characteristics of neurosyphilis. The most common form of neurosyphilis is asymptomatic neurosyphilis and meningoencephalitis, although meningovascular syphilis was the most common form in some cohort studies [3–6]. The prevalence of pre-antibiotic era symptoms, such as tabes dorsalis, paralytic dementia, and gummous neurosyphilis, dropped sharply as the widespread use of antibiotics for other diseases could indirectly treat neurosyphilis, while timely diagnosis and treatment shortened the course of the disease. Neurosyphilis, which is considered an excellent mimic of neuro-ophthalmic, auditory-vestibular and mental disorders, is often combined with other diseases. In this regard, it is always important to keep in mind the cerebrovascular form of neurosyphilis, which is likely in different age groups [7-12]. Taking into account the presence of infectious, vascular and autoimmune mechanisms in the formation of early neurosyphilis, fast and adequate verification of the process is essential.
The objective of the study was to identify the clinical features of neurosyphilis against the backdrop of abnormal development of cerebral arteries on the basis of screening examination data and a description of a clinical example.
To study the relationship of clinically significant variations of human cerebral arteries with the features of clinical manifestations of modern early neurosyphilis, we analyzed the case histories of 3 954 patients aged 15–86 years with varying degrees of neurological deficit who had received treatment from November 2010 to November 2020 in the city neurology department. All patients underwent general clinical and neurological examinations, electrocardiography, clinical laboratory and biochemical tests and, of course, the classical Wasserman test. If clinically indicated – ophthalmological, immunological, neurophysiological (EEG, EMG, TCDG), neuropsychological and radiological examinations, general analysis of cerebrospinal fluid, the Wassermann test and immunofluorescence test with various dilutions of cerebrospinal fluid, as well as magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the cerebral arteries of the circle of Willis.
The screening identified one verified case of early cerebrovascular neurosyphilis.
Patient M., 53 years old, unemployed. He underwent examination and treatment in the neurological department of the City Hospital No. 4 in Tambov. He was admitted with complaints of weakness in the left limbs. He had been sick for about 2 months, when gradually began to feel weakness of the left limbs. He went to seek medical help, "because the arm and leg grew completely numb". He was treated in the neurological department of the district hospital at the place of residence with a diagnosis of "Ischemic stroke in the system of the right middle cerebral artery in presence of chronic alcohol intoxication" without a clear effect. Anamnesis: infrequent colds, long-term abuse of alcohol and its surrogates, as well as smoking. He categorically denied any other diseases. MRI of the brain: In the right hemisphere of the brain: massive cerebrovascular disorders associated with dyscirculation. Median structures were not displaced. The ventricles were dilated to 1-2 degree. 4th ventricle was in the midline. The pituitary gland was not enlarged. MRA: Posterior trifurcation of the right internal carotid artery, hypoplasia of both posterior communicating arteries. See the Figure 1.
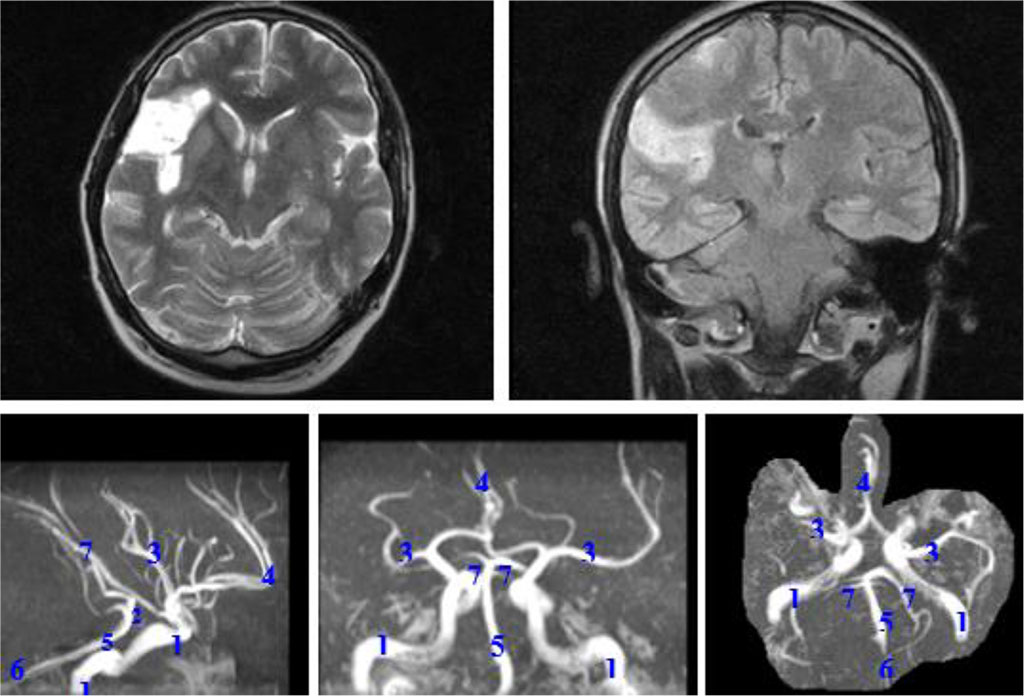
Figure 1. MRI: postischemic changes in the right hemisphere. Magnetic resonance angiography: posterior trifurcation of the right internal carotid artery, hypoplasia of both posterior communicating arteries. 1 - internal carotid arteries; 2 - posterior communicating arteries; 3 - middle cerebral arteries; 4 - anterior cerebral artery; 5 - basilar artery; 6 - vertebral arteries; 7 - posterior cerebral arteries.
Objective data on admission: BP = 130/80 mm Hg; Heart rate = 74 bpm, rhythmic. Examination by a therapist revealed chronic gastritis and chronic cholecystitis. Neurological data: clear consciousness, but reduced cognitive functions; no meningosigns; positive Argyll Robertson’s sign, moderate paresis of the left facial muscles, tongue deviation to the left; left-sided hemihypesthesia, plegia of the arm, leg paresis (up to point 1-2), tendon reflexes: S > D, pathological hand and foot signs on the left; pelvic functions in order. ECG: sinus rhythm – 60 per minute, slowed intra-atrial conduction, moderate changes in the myocardium. UA and CBC – no pathology. Cholesterol – 4.1 mmol/l, β-lipoproteins – 4.4 g/l, urea – 4.6 mmol/l, creatinine – 70 µmol/l, ALT – 23 U/l, AST – 16 U/l, CPK – 108 U/l, bilirubin – 7.6 μmol/l. Peripheral blood glucose – 4.7 mmol/l. Prothrombin – 97%, fibrinogen – 4.1 g/l. WR – (4+) strong-positive. Dermatovenereologist: latent early seropositive syphilis. Immunofluorescence test (CSF) – (4+) strong-positive. CFT (CSF) with trepanema antigen – (4+), CFT with cardiolipin antigen – (4+) in all three dilutions. CSF culture for flora and sensitivity to antibiotics: double culture, no growth. Dermatovenereologist (repeated) – early meningovascular syphilis of the nervous system.
Improvement after treatment (Penicillin Sodium Salt, Carnitine Chloride, Mildronate, Glycine, Cerebrolysate): cognitive functions with positive dynamics, doubtful Argyll Robertson’s sign, left-sided hemiparesis of the arm (up to 2 points) and of the leg (up to 3 points).
Discharged with a diagnosis of early meningovascular neurosyphilis, early recovery period after CVA syndrome in the right hemisphere. Catamnesis not available.
Thus, the singularity of the case, the difficulty of diagnosing due to the bias of data on CVA syndrome, the rate of the disease course, and the cumulative data of neuroimaging make us assume a clear connection between the occurrence of meningovascular syphilis of the nervous system and developmental variations of the circle of Willis. These circumstances suggest to consider constitutionally determined variations and/or developmental anomalies of the arteries of the circle of Willis as an additional risk factor for CVA syndrome in infectious processes of the brain, all other things being equal.