- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
DOI 10.35630/2022/12/psy.ro.20
![]() terpan.mihai@yahoo.com, baciu91@yahoo.com, carmengavrilaa@gmail.com
terpan.mihai@yahoo.com, baciu91@yahoo.com, carmengavrilaa@gmail.com
Introduction: According to the studies, a quarter of people who drink alcohol suffer at least one depressive episode in their lifetime. It has also been found that one-third of people who suffer from depression, abusively consume psychoactive substances, such as alcohol, as a form of self-healing.
Aim: In this retrospective study, we propose to statistically quantify the relationship between alcohol-related mental and behavioural illnesses and depression spectrum disorders.
Method: The retrospective study was conducted on a group of hospitalized patients, between January 1st and June 30th, 2018, at "Elisabeta Doamna" Psychiatric Hospital, in Galati, Romania. For diagnosis we used the ICD-10 (The ICD-10 Classification of Mental and Behavioral Disorders. (Clinical description, diagnostic guidelines and psychometric tests, such as HAM-D (Hamilton Depression Rating Scale)), AUDIT (Alcohol Use Disorders Identification Test). Patients were selected among those who had a combination of mental and behavioural disorders due to alcohol and depressive spectrum disorders.
Results: Between January 1st and June 30th, 2018, a quarter of total 6316 hospitalized patients, or 24.79% (1566 patients) were diagnosed with alcohol-related disorders, and 5.4% (341 cases) had a dual diagnosis, with alcohol-related disorders associated with depressive elements. During this 6-month period, of all cases of alcohol-related disorders, it was found that approximately 22% had a dual diagnosis, respectively, the combination of alcohol-related disorders with depressive spectrum disorders or depressive elements.
Conclusions: Unfortunately, it is estimated that depression will become a secondary cause of disability worldwide after cardiovascular disease. According to the WHO (World Health Organization), this disease affects more than 320 million people worldwide, and its combination with alcohol abuse is alarming.
Therefore, patients with dual diagnosis require a multidisciplinary therapeutic approach to reduce or even neutralize the adverse consequences that may occur in the psycho-social, medical, family, economic, or behavioural context.
Keywords: psychiatry, depression, alcohol, dual diagnosis
Psychiatric medical practice reveals illnesses such as alcoholism and depression as two of the most common disorders that affect mental health. In this regard, the combination of these two diagnoses has a significant impact on life and necessitates treatment for the patient. Alcohol consumption can lead to an increase in depressive symptoms, a more frequent and severe depressive episode, and a greater predisposition towards suicidal ideation (Ciubara et al., 2018; Donohue & Pincus, 2007). Antidepressant medication is far less effective if, in parallel, there is also alcohol dependence.
According to National Survey on Drug Use and Health, for 2014, 7.9 million persons in the United States have both a mental disorder and a substance use problem.
The co-occurrence of alcohol consumption disorders with other mental disorders is well known (Kessler et al., 1997). When an individual begins to use alcohol to cope with psychiatric distress, the onset of the other disorder may be significantly influenced. The "dual diagnosis" patient can be difficult to treat since he/she/they may not react well to normal addiction therapy and may have higher rates of relapse, dropout, and readmission. However, if a concomitant psychiatric disorder is discovered, identifying the relative beginning of the two disorders may have therapeutic value because primary disorders tend to have greater long-term clinical significance.
There is a profound connection between depressive disorders and alcohol consumption, and this guide us towards the following dilemma: regular alcohol consumption may predispose people to depression, or depressed people are more prone to alcohol? Both versions are valid.
The goal in conducting this retrospective study is to statistically quantify the connection between alcoholism-related mental and behavioural disorders and the depressive spectrum disorders.
From the standpoint of public health, depressive disorders are very relevant since they are widespread, have good treatments available, and may seriously impair psychosocial function (Paduraru et al., 2019). These ailments have a significant negative impact on patients and their families, and they are one of the main causes of occupational absenteeism (Donohue & Pincus, 2007; Stern et al., 2008; Valcea et al., 2016).
At the "Elisabeta Doamna" Psychiatric Hospital in Galati, Romania, between January 1 and June 30, 2018, a group of hospitalized patients was the subject of this retrospective study. For diagnosis we used the ICD-10 (World Health Organization, 1993) and psychometric tests, such as HAM-D (Hamilton Depression Rating Scale), AUDIT (Alcohol Use Disorders Identification Test).
Patients were selected who match the combination between mental and behavioural disorders due to alcohol and depressive elements or depressive spectrum disorders.
For the statistical interpretation of the data, we used the following programs: Microsoft Excel 2010, Epi Info 7 (a free and open-source collection of interoperable software tools for the global community of public health practitioners and researchers), JASP Statistics (an open-source statistical program), and SOFA Statistics (an open-source statistics, analysis, and reporting software).
Of all
6316 patients hospitalized between January 1st and June 30th, 2018, a
quarter of them, 24.79% (1566 patients), were diagnosed with
alcohol-related disorders.
There were
341 cases of "dual diagnosis" among the 1566 cases
diagnosed with alcohol consumption, accounting for 5.4% of the total
number of studied cases and 21.78% of alcohol-related disorder
diagnoses.
These 341 cases include alcohol-related disorders and depressive spectrum disorders (Fig. 1, Fig. 1.1). Of these 1566 cases with an alcohol-related diagnosis, 85.76% (1343 patients) have the primary diagnosis of hospitalization, and 14.24% (223 patients) have the secondary diagnosis of being admitted for alcohol-related disorders.
| Total number of patients | Diagnosis
related to alcohol consumption |
Dual Diagnosis (number & percentage of total cases) | Dual Diagnosis (number & percentage of dg with alcohol) | Dual Diagnosis female urban (number & percentage from alcohol diagnosis) | Dual Diagnosis male urban (number & percentage from alcohol diagnosis) | Dual Diagnosis female rural (number & percentage from alcohol diagnosis) | Dual Diagnosis male rural (number & percentage from alcohol diagnosis) |
| 6316 | 1566 | 341 | 341 | 77 | 194 | 13 | 57 |
| 100% | 24.79% | 5.4% | 21.78% | 4.92% | 12.39% | 0.83% | 3.64% |
Figure 1.
Distribution of diagnoses (alcohol
related,
depressive spectrum, dual diagnosis)
Source: Authors' own
conception
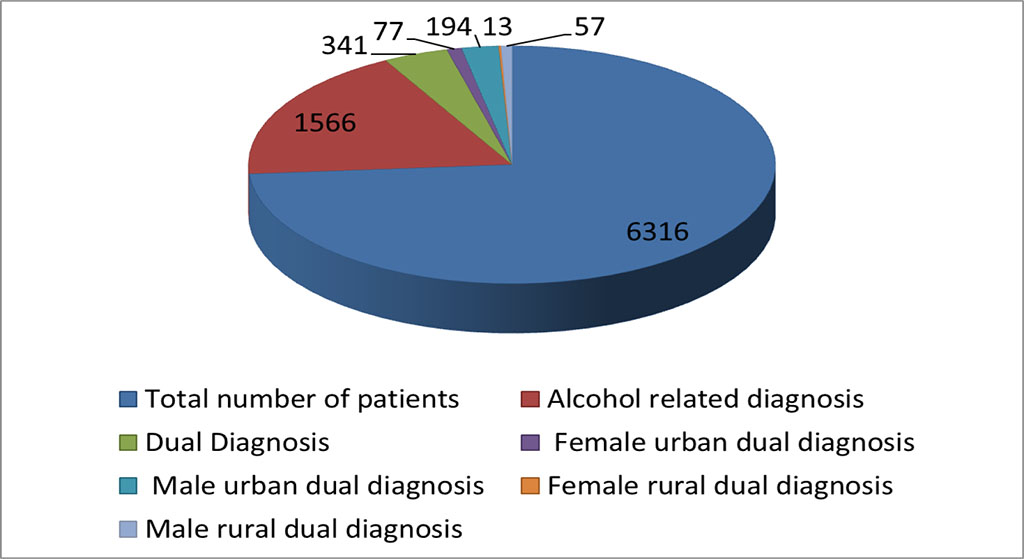
Figure 1.1. Graphical Distribution of diagnoses (alcohol related, depressive
spectrum, dual diagnosis
Source: Authors' own
conception
During this 6-month period, of all cases of alcohol-related disorders, it was found that approximately 22% (341 patients) of them presented "dual diagnosis", namely, the association of alcohol-related disorders with depressive spectrum disorders or depressive elements.
| Gender and residence | F10.0 | F10.1 | F10.2 | F10.3 | F10.4 | F10.5 | F10.8 |
| Female | 28 | 9 | 4 | 19 | 2 | 0 | 27 |
| Male | 46 | 36 | 66 | 69 | 3 | 1 | 30 |
| Urban area | 63 | 39 | 47 | 62 | 3 | 1 | 2 |
| Rural area | 11 | 6 | 23 | 26 | 2 | 0 | 5 |
Figure 2. Distribution of alcohol
related disorders, by gender and residence
Source: Authors' own conception
According to ICD-10, mental and behavioural disorders due to the use of psychoactive substances have the following codes: F10 to F19.
Figure 2 Figure 2.1 Figure 2.2
F10.0 = acute intoxication
F10.1 = harmful use
F10.2 = addiction syndrome
F10.3 = withdrawal state
F10.4 = withdrawal state with delirium
F10.5 = psychotic disorder
F10.8 = other mental and behavioral disorders (Kaplan et al., 1994)
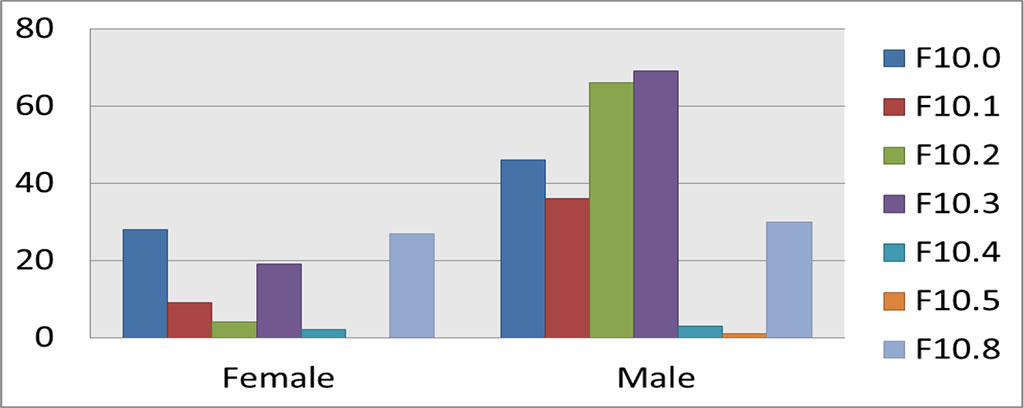
Figure 2.1 Graphical distribution of alcohol related
disorders, by gender
Source: Authors' own conception
F10.0, female, acute intoxication↑↑↑
F10.3, male, withdrawal state↑↑↑
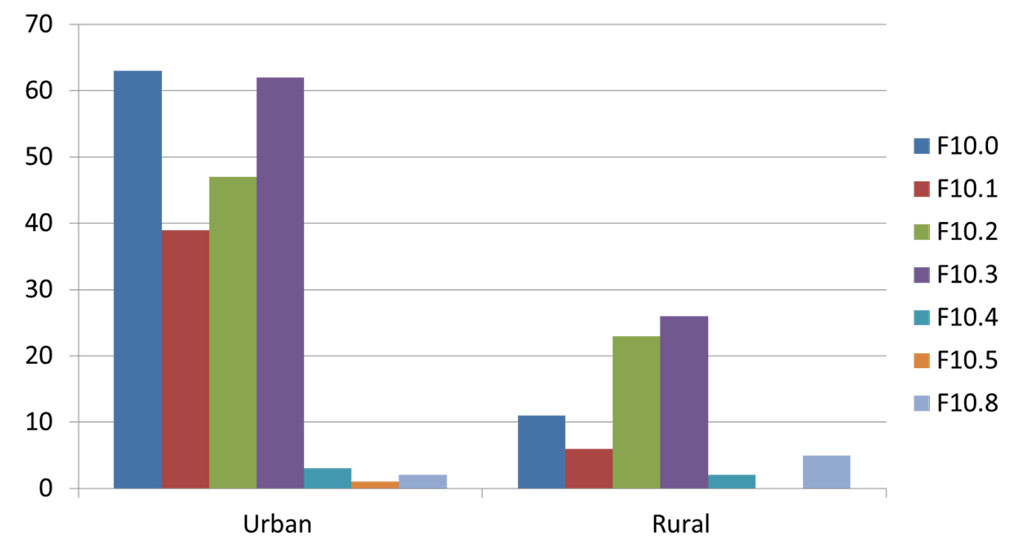
Figure 2.2 Graphical distribution of alcohol related disorders, by residence
Source: Authors' own conception
F10.0, urban, acute intoxication↑↑↑
F10.8, rural, withdrawal state↑↑↑
| Residence and gender | Depresive elements | F32 | F32.1 | F32.2 | F34 | F34.8 | F38 | F41 | F41.2 | F43 | F43.2 |
| Urban | 147 | 6 | 3 | 2 | 1 | 4 | 70 | 5 | 13 | 4 | 18 |
| Rural | 26 | 2 | 0 | 0 | 2 | 4 | 25 | 0 | 8 | 0 | 3 |
| Female | 67 | 0 | 2 | 2 | 0 | 2 | 9 | 0 | 4 | 0 | 6 |
| Male | 106 | 8 | 1 | 0 | 3 | 6 | 86 | 5 | 17 | 4 | 15 |
Figure 3. Distribution
of depressive spectrum disorders, depressive, anxiety or stress
elements, by residence and gender.
Source: Authors' own
conception
According to ICD-10, mood (affective) disorders have the following codes, F30–F39, and neurotic, stress-related, and somatoform disorders have the following codes, F40–F48.
F32 = depressive episode
F32.1 = moderate depressive episode
F32.2 = major depressive episode without psychotic symptoms
F34 = persistent mood disorders
F34.8 = other persistent mood disorders
F38 = other mood disorders [affective]
F41 = other anxiety disorders
F41.2 = mixed anxiety and depressive disorders
F43 = response to severe stress and adjustment disorders
F43.2= adjustment disorders
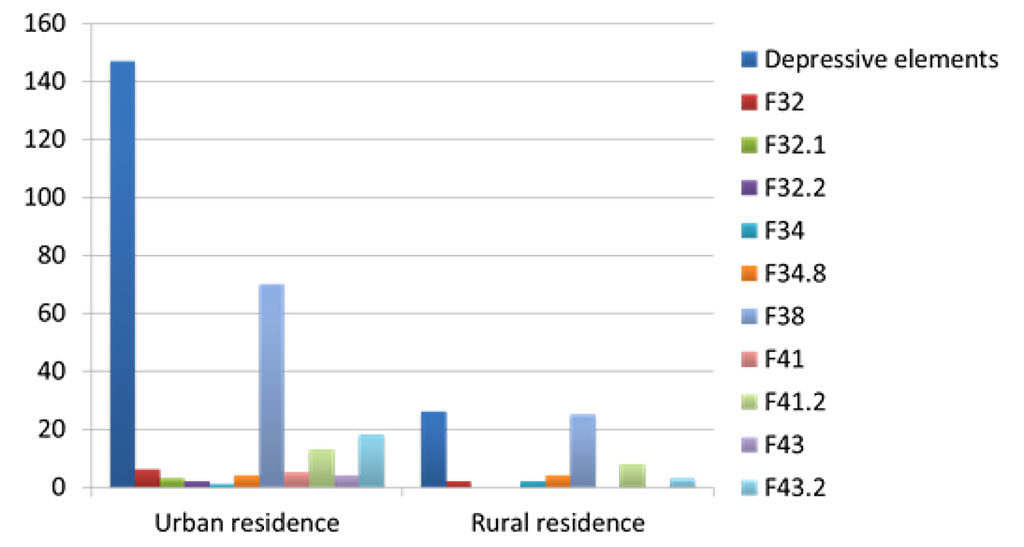
Figure 3.1 Graphical distribution of depressive spectrum disorders, anxiety,
stress or depressive elements, by residence
Source: Authors' own
conception
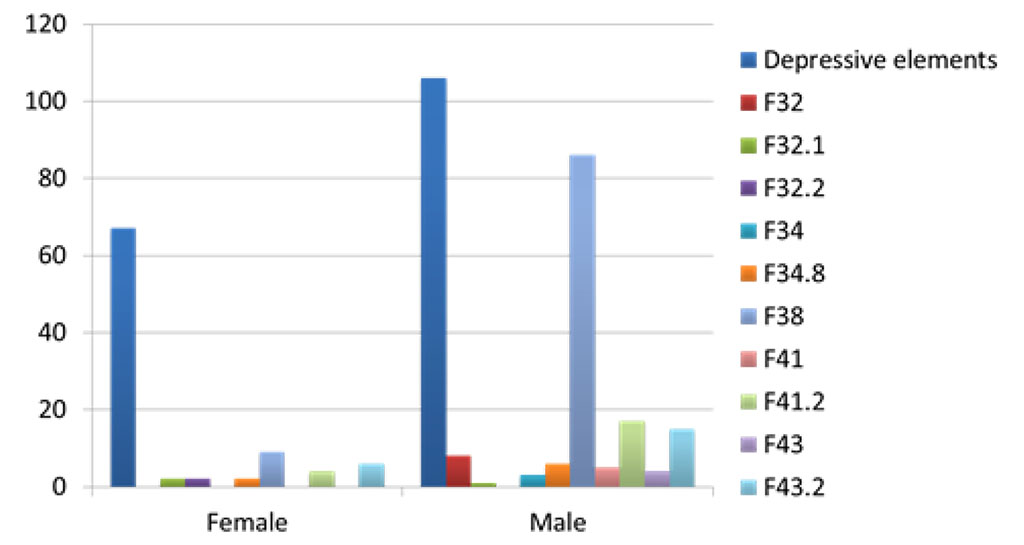
Figure 3.2 Graphical distribution of depressive spectrum disorders, anxiety,
stress, or depressive elements, by gender
Source: Authors' own conception
Alcoholism is associated with a high rate of depression (Kuria et al., 2012; Ciobotea et al., 2016). Unfortunately, depression is expected to be the second leading cause of disability worldwide by 2020, behind cardiovascular illness (Rădulescu et al., 2020).
According to the World Health Organization (n.d.), this condition affects more than 320 million individuals globally, and its link to alcohol misuse is concerning. There is depression recovery after alcohol detoxification and rehabilitation, and the majority of instances do not require depression treatment.
Furthermore, depressed people have a considerably increased need for alcohol after detoxification and rehabilitation. It is critical to screen for and diagnose depression in order to determine treatment needs throughout detoxification and recovery.
Therefore, patients with dual diagnosis require a multidisciplinary therapeutic approach to reduce or even neutralize the adverse consequences that may occur in the psycho-social, medical, family, economic, or behavioural context.