- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 6. DOI 10.35630/2024/14/6.608
Recently, there has been an increase in publications devoted to sentinel lymph node biopsy (SLNB) in oral cancer. It has been established that cervical lymph node involvement, even in small primary tumors, is an unfavorable prognostic sign and is associated with a more than twofold decrease in overall survival. This creates a need to develop new methods for detecting hidden regional metastases, which, in turn, can improve long-term treatment outcomes.
Our study included 16 patients with primary tongue cancer cT1-2N0M0 subject to selective or modified radical neck dissection, as well as radical tongue resection. Patients under 18 years of age, with previous neck surgery or radiation therapy, and with iodine allergy were excluded. Sentinel lymph node (SN) mapping was performed using the SPY-PHI Stryker navigation system, which simultaneously displays color video and fluorescence images. Tracers such as ICG (5 mg/mL) and methylene blue (10 mg/mL) were injected around the tumor, followed by a standard neck incision and measurement of fluorescence signal to identify SNs, which were then removed for histologic examination.
All patients were able to reconstruct the tongue with local tissues and there were no technique-related complications. Sentinel lymph nodes (SLNs) were successfully identified in all cases, with four patients having histologically confirmed occult metastases. Nodal classification changed in three patients from cN0 to pN1 and one to pN2, and additional blue-staining lymph nodes were found in 11 patients, all of whom remained N0. The ICG sentinel lymph node method has been used in medicine since 1957 to assess organ function and angiography. ICG quickly binds to plasma proteins and is removed by the liver, making it a safe, radiation-free indicator that is less expensive than X-ray methods.
The SNB procedure with ICG NIF imaging is simple and fast, but tissue swelling may occur during the first 24 hours. However, detection of nodes through the skin is difficult in patients with normal or high body weight, since the lymphatic vessels are located deeper and are blocked by surrounding tissue. A sentinel lymph node indicates damage to a specific lymphatic channel or collector.
Keywords: sentinel lymph node, biopsy, metastases, lymphadenectomy
In the last decade, there have been more and more publications in the domestic literature on the performance of sentinel lymph node biopsy (SLNB) in oral cancer. It is known that the involvement of cervical lymph nodes, even with a small primary tumor, is prognostically unfavorable and is associated with a decrease in overall survival by more than two times. This encourages researchers to search for new methods for detecting hidden regional metastases, which will ultimately improve the long-term treatment results [1-6].
It should be noted that today there is no absolutely accurate diagnostic test that could assess the status of cervical lymph nodes in clinically undetectable nodes (N0) [7,11]. In this case, either patient observation or preventive cervical lymphadenectomy (CLA) can be performed. This operation is justified from an oncological standpoint, but is certainly not safe for the patient [8,9,12,13].
Researchers indicate that, according to the results of prophylactic cervical lymphadenectomy, in 30-50% of patients, no lymph nodes metastases are detected during routine examination [9,13,15,16,17]. Consequently, these patients could avoid extensive surgery, often associated with serious complications (nerve paresis, coarse scars on the neck, myofascial pain, limited movement in the shoulder joint, etc.) [18,19].
And although selective cervical dissection for N0 is generally accepted and more gentle than radical CLA, it can undoubtedly be unjustified.
The presence of hidden lymph nodes metastases was detected in less than 1/3 cases of operated patients, which means that the remaining 2/3 underwent unnecessary surgery [19,20].
It is also known that the thickness of the tumor directly correlates with the risk of metastatic lesions of the lymph nodes (Fig.1.).
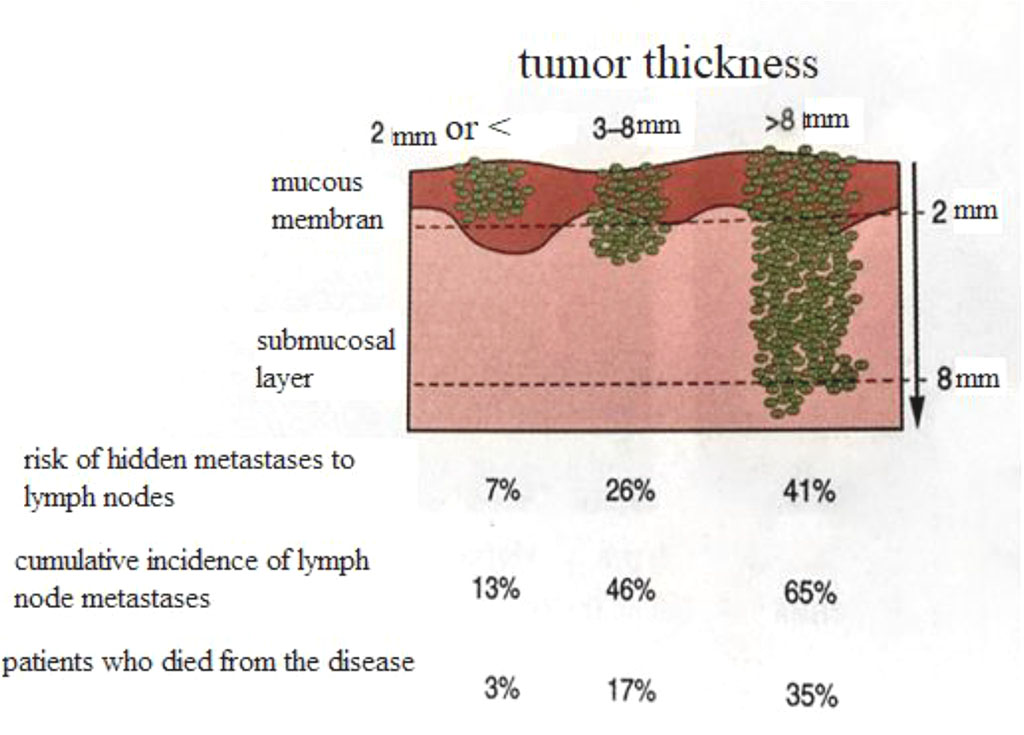
Fig. 1. Scheme of correlation of tumor thickness with its metastatic potential.
The lymphatic vessels were named by Thomas Bartolini (1616–1680) from Denmark [9]. Virchow formulated the theory in the 19th century that the lymph nodes filter particulate matter from the lymph. To determine the barrier function of the lymph nodes, several investigators injected particulate matter or tumor cells into the afferent lymphatic vessels in animal experiments. The tumor emboli were immediately trapped in the subcapsular sinuses and did not spread to the next lymph nodes for some time [12]. The anatomy of the cervical lymphatic system was described in detail in 1932 by Rouvier [13].
The term sentinel lymph node in oral cancer was first introduced by Ernest Gould in 1959, during an urgent biopsy of a lymph node found at the confluence of the anterior and posterior jugular veins [21,22, 23].
The history of SLNB has been around for over 40 years and this study is standard for breast cancer and melanoma [18,20].
The main idea of SLNB is that lymph spread from the tumor does not occur randomly, but through the first, so-called "sentinel lymph node", and then spreads to subsequent regional lymph nodes.
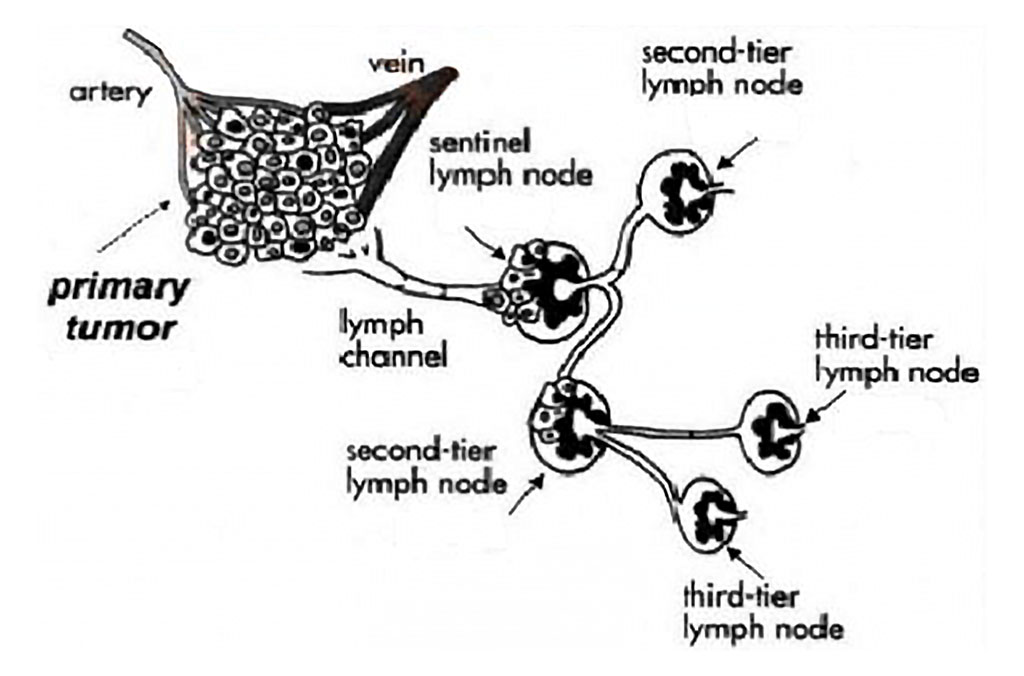
Fig. 2. Scheme of tumor cell dissemination through the sentinel node.
To assess this process, the lymphoscintigraphy technique was actively studied in our country in the 1970s and 1980s [6,7]. However, it did not have any practical significance at that time. This direction was looked at in a new way at the beginning of the 21st century, when they began to use intraoperative detection of nodes with a γ-probe or dye mapping. It should be noted that access to radioactive isotopes is very limited in many surgical clinics, and there is also a potential risk of radioactive indicators for the operating team.
Near infrared fluorescence imaging (NIF) is a newer SNB method first introduced by Kitai et al. in 2005 [16]. Subsequent reports of its successful use in gastric, gynecological, lung, esophageal, and skin cancers have been reported in the literature [18,19,20].
Several pilot studies of SNB with NIF mapping in oral mucosal cancer have been published, demonstrating the efficacy and safety of this method.
However, all investigators note that further refinement of the technique and recruitment of a larger number of patients are required. The validity of NIF imaging using indocyanine green (ICG) for evaluation of cervical lymph nodes in oral mucosal cancer (with N0) needs to be established. Scientists from Karolinska University came to the conclusion that SLN and adjacent “healthy” nodes differ in the qualitative and quantitative composition of T-lymphocytes. SLN contain a significantly higher number of B-cells with an immunosuppressive phenotype (IL-10).
High expression of PD-L1 by dendritic cells of the affected node is associated with a worse prognosis. High concentrations of dendritic cells and cytotoxic lymphocytes in SLN were regarded as potential biomarkers of an aggressive clinical course of the tumor [24, 25].
The level of CD8⁺ T-lymphocytes in the affected node was also assessed, compared with healthy ones. Krzysztof Piersiala, Vilma Lagebro (2023) concluded that SLNs contain cells that are effective trigger-detectors that recognize the tumor and provide an antitumor response (primarily due to dendritic cells (DC1) and CD8⁺ T-cell. And a high level of PD-L1 expression by dendritic cells is a factor in poor tumor prognosis [25,26,27].
This study included 16 patients with cT1-2N0M0 primary tongue cancer scheduled for selective neck dissection (levels I-III) or modified radical cervical dissection, and radical tongue resection (removal of the primary tumor). Exclusion criteria were age <18 years, history of previous cervical surgery or radiotherapy, and iodine allergy. Clinical staging was based on physical examination and imaging studies (CT or MRI with contrast). Written informed consent was obtained from all patients before SNB.
SN mapping was performed using the SPY-PHI Stryker surgical navigation system. The system consists of two wavelength-separated light sources: a “white” light source generating 400-650 nm light and a “near infrared” light source generating 760 nm light. Color video and NIR fluorescence images are simultaneously captured and displayed in real time using specialized optics and software that separate the color video and NIF images. The imaging head is attached to a flexible, dual-hinge arm, allowing the imaging head to be positioned virtually anywhere in the surgical field.
ICG was dissolved at a concentration of 5 mg/ml, and methylene blue was prepared at a concentration of 10 mg/ml. One milliliter of ICG was injected around the tumor from four points. A standard neck incision (in the fluorescence zone) was made 15-20 minutes after the tracers were injected. After retracting the sternocleidomastoid muscle posteriorly, the fluorescent signal in the surgical field was measured using the navigation system. At this time, intense fluorescence foci appeared on the screen. Particular attention was paid to the lymphatic vessels and lymph nodes stained greenish. The first lymph nodes to appear with NIF foci with or without visible dye were defined as SN and were removed for further confirmation under a microscope (Fig. 4). All nodes were sent for histological and immunohistochemical examination.

Fig. 3. Indocyanine green was injected at a concentration of 5 mg/1 ml around the tumor in 4 directions (from one injection) a-before, b-after.

Fig. 4 After retracting the sternocleidomastoid muscle posteriorly, the fluorescent glow of the node is visible under the influence of an infrared light source.
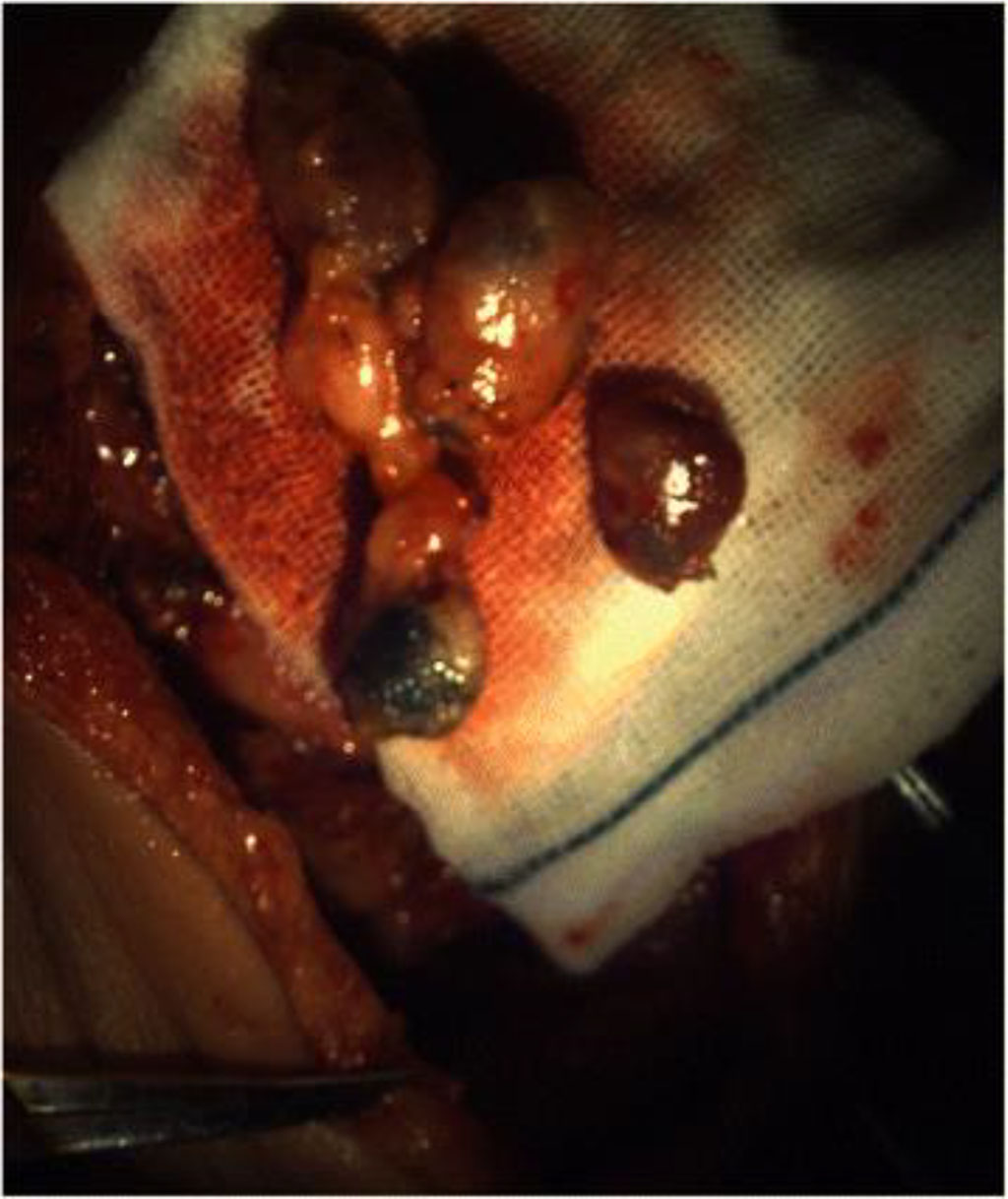
Fig. 5 Remote signal nodes, painted with dye, also glow under the influence of a light source.
This study included 16 patients with squamous cell carcinoma of the tongue, operated in 2023-2024 in Moscow City Hospital #62, with a clinical stage T1-2N0M0. The average age of the patients was 60.5 years (range 43-77 years). The primary tumor was cT1 in 13 patients, cT2 in 3 patients. The localization of the primary tumor included the lateral surface of the tongue (n = 13), dorsum of the tongue -1, tip of the tongue -2. All patients were able to restore the tongue with local tissues. There were no technique-related complications. SNB increased the overall operative time by an average of approximately 30 minutes.
The most frequently affected level was II 14 (88%), level I (2) 12.0%. All SLNs were successfully identified in all 16 cases, without false negative results. Histological examination after cervical lymph node dissection revealed occult lymph node metastases in four patients.
The node classification was changed in 3 patients from cN0 to pN1 and in one patient to pN2. Additional blue-stained lymph nodes were found in 11 patients after SNs removal. All of these lymph nodes were N0. No complications related to ICG injection were observed in this series.
The method of determining the signal lymph node using ICG has been widely used in various fields of medicine since 1957 [16]. The method is widely used to assess liver/kidney function, retinal angiography, and cardiac output. The advantage of ICG is that immediately after administration, it quickly binds to plasma proteins and is retained in the vascular space. ICG is removed exclusively by the liver at a rate of 18-24% per minute with a half-life of 150-180 s [21].
Compared with the γ-probe, this method has several advantages. SNB using NIF imaging with ICG is a convenient one-step procedure. ICG is a radiation-free, safe indicator, and no special radiation protection is required. The cost of a full dose of ICG is much lower than that of a radiological indicator, and the fluorescence imaging device is also cheaper than a γ-probe. The injection technique is simple and repeatable. Detection and search for nodes is carried out quite quickly (about 15 minutes). However, it should be noted that in the first 24 hours after the introduction of ICG into the tongue tissue, quite pronounced edema is possible, which passes against the background of infusion therapy, antibiotics, and anti-edema therapy.
Another feature of detection is the fact that through the skin - "directly" the node can be detected only in asthenic patients. When stimulated by near infrared light, the fluorescent signal of ICG is clearly and distinctly determined after the abduction of the sternocleidomastoid muscle.
At the initial stage, our attempts to measure the fluorescent signal transcutaneously were ineffective in 4 cases. We believe that the physical explanation for this fact is that the thickness of NIF penetration from ICG through soft tissues is 0.5–1 cm [17], while the ervical lymphatic vessels coming from the oral cavity to the SLN are located in deep layers of adipose tissue and are blocked either by the mandible or the sternocleidomastoid muscle, which makes it impossible for the scanning camera to capture the NIF signal transcutaneously. The concept of a sentinel lymph node is a lymph node located near the tumor, and in some cases at a distance from it, indicating the lesion of a certain lymphatic bed or collector.
Patient G., 55, came to the appointment due to the presence of a 1.0 cm formation on the back of the tongue. Morphological verification of the formation was performed on an outpatient basis: No. 20043030/24: Squamous cell keratinizing carcinoma with a lesion of the tongue.
On examination: on the back of the tongue along the midline, in the center - an exophytic formation with an ulcer in the center - up to 1 cm;
Hospitalized in the Department of Head and Neck Pathology for surgical treatment.
05/15/2024, tongue resection was performed with identification and biopsy of the sentinel lymph node.
At the same time, the distribution of the drug was not typical. As can be seen from the photo, at first the distribution was directed in both directions. But after 20 minutes, the node in the submandibular zone on the right began to be determined most intensively.

Fig.6 Intraoperative photo of the spread of the drug along the lymphatic pathways.
The sentinel node was identified in the submandibular region on the right, near the horn of the hyoid bone. During the planned histological examination, no metastases was found in it.
According to the results of pathohistological examination O24005516-1 Squamous cell keratinizing cancer of the tongue. pT2 pN0(0/3) R0.
The surgical outcomes were discussed at the oncological council and it was decided to leave the patient under dynamic observation.
Currently, the patient is observed without relapses and metastases
In patients with early stages of oral mucosal cancer (T1, T2) in the absence of clinical data for lymph node involvement, it is advisable to use the SLN determination method.
Near infrared imaging using indocyanine green is an effective method for determining SLN in patients with N0.
The authors declare no conflict of interest.