- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 6. DOI 10.35630/2024/14/6.604
Aims: Studying the results of the reconstruction of pediatric multi-facial fracture.
Case Description: In our study we present a 13-year-old boy with facial oedema, oral pain and bleeding due to falling from height. Upon examination, the patient had a left parasymphysial mandibular fracture and maxillary fracture Le fort I.
Conclusions: A combined closed reduction with intermaxillary fixation and maxillary-frontal suspension and open reduction using interosseous wiring had restored the preoperative anatomical, functional and cosmetic aspects of the patient, which was found to be a reliable, cost-effective method for surgical management of pediatric facial trauma.
Keywords: Pediatric facial trauma, Fracture mandible, Le fort classification, closed reduction, interosseous wiring.
Children are more subjected to sustain cranio-facial trauma than adults due to a higher cranial-facial volume (8:1 in newborns Vs. 2.5:1 in adults). Injuries occur predominantly in boys due to motor vehicle collisions, falls, violence, and sports-related trauma. Falls usually predominate in children younger than six years and sports injuries are more prevalent during adolescence. Cranio-facial trauma is a major cause of disability and death among children [1]. Delayed evaluation and management result in > 30% of deaths among seriously injured children [2]. The most common fracture sites are mandibular, nasal and orbital [3], which are generally non-displaced due to the flexibility of the facial skeleton and the presence of unerupted milky teeth [4]. Maxillofacial soft tissue injuries often occur in palate [5]. Unerupted canine may promote for mandibular symphysis/parasymphysial fractures [6]. The goal of treatment is restoration of preinjury function, occlusion, facial symmetry, and minimizing disruption of normal growth and development [7].
A 13-year-old boy was referred to our emergency clinic due to falling from high (F.F.H.).
General examination: No fractures, wounds or bleeding other than the craniofacial region. Normal vital signs. Neurological examination; the patient was alert, conscious, crying, in-pain. Head and neck examination; no airway obstruction, no foreign bodies in the respiratory tract. No features of cervical spine fracture. Glasgow Coma Scale (GCS) was 15/15.
Facial examination: Mild facial oedema, multiple facial abrasions and contusions. Oral malocclusion, lost maxillary central, left lateral incisors and canine, tender mobile maxilla; Le fort I fracture (Table 1), soft palatal tear (Figure 1) and a complex displaced left parasymphysial mandibular facture with lost left mandibular lateral incisor (Table 2).
Table 1: Le Fort classification [8].
| Grade | Extent of fracture line |
| Le Fort I | The anterolateral margin of nasal fossa. |
| Le Fort II | The inferior orbital rim. |
| Le Fort III | The zygomatic arch. |

Figure 1: The maxillary Le Fort I and the left parasymphysial mandibular fractures.
Table 2: Classification of mandibular fracture [9].
| (I) According to the fracture site. | Fracture-site |
| 1. Symphysial. | In the incisor area, from the alveolar process to the lower border of the mandible. |
| 2. Parasymphysial. | Between the incisor and mental foramen. |
| 3. Body. | Between mental foramen and 2nd molar. |
| 4. Angle. | Distal to 2nd molar to the posterior border of the ramus. |
| 5.
Ramus. |
From the posterior border of the ramus to the lower border of the mandible. |
| 6.
Condyle. |
From the sigmoid notch along the upper part to the posterior border of the ramus. |
| 7. Coronoid process. | In coronoid process. |
| 8. Dentoalveolar. | Fracture of the alveolar process and supporting root structure; doesn’t involve the basal bone of the mandible. |
| (II) According to the Fracture pattern. | Pattern |
| 1. Closed (simple) | Fracture has no communication with the external environment. |
| 2. Open (compound). | Fracture has communication with the external environment. |
| 3. Complex (Complicated). | Simple or compound fracture associated with soft tissue injury. |
| 4. Comminuted. | Multiple bony segments are shattered/crushed. |
| 5.
Multiple. |
Two or more fractures within the same bone, without communication with each other. |
| 6.
Pathological. |
Fracture occurring from pre-existing disease which had weakened the bone. |
| 7. Greenstick. | Incomplete fracture involves only one bony cortex. |
| 8. Atrophic. | A spontaneous fracture within an atrophied mandible (edentulous mandible with <20 mm heigh). |
| 9. Indirect. | Occurs at a site distant from the area of impact e.g., “Guardsman fracture” having bilateral condylar neck fractures’ secondary to a direct trauma to the chin causing symphyseal fracture. |
| 10. Impacted. | Bone segments are telescoped over each other. |
| (III) According to the fracture biomechanics. | Stability |
| 1.Favorable (stable). | The fracture line and the vector of the muscle pull keep the fracture appropriately reduced. |
| 2.Unfavourable (unstable). | The fracture line and the vector of the muscle pull cause displacement. |
| (IV) According to the presence or absence of teeth on both sides of the fracture | Dentation |
| 1.ClassI. |
Teeth on both sides of the fracture. |
| 2.Class II. | Teeth on only one side of the fracture. |
| 3.Class III. | Edentulous or without teeth on both sides of the fracture. |
Cranio-facial Multidetector Computerized Tomography (MDCT) confirmed our diagnosis, excluded other fractures, intracranial lesions, cerebral oedema and hemorrhage [Figure 2,3]. The patient was given one gm I.V. CefotaximeTM. The decision was made for closed reduction (except for the mandibular fracture) under general anathesia with nasal intubation.
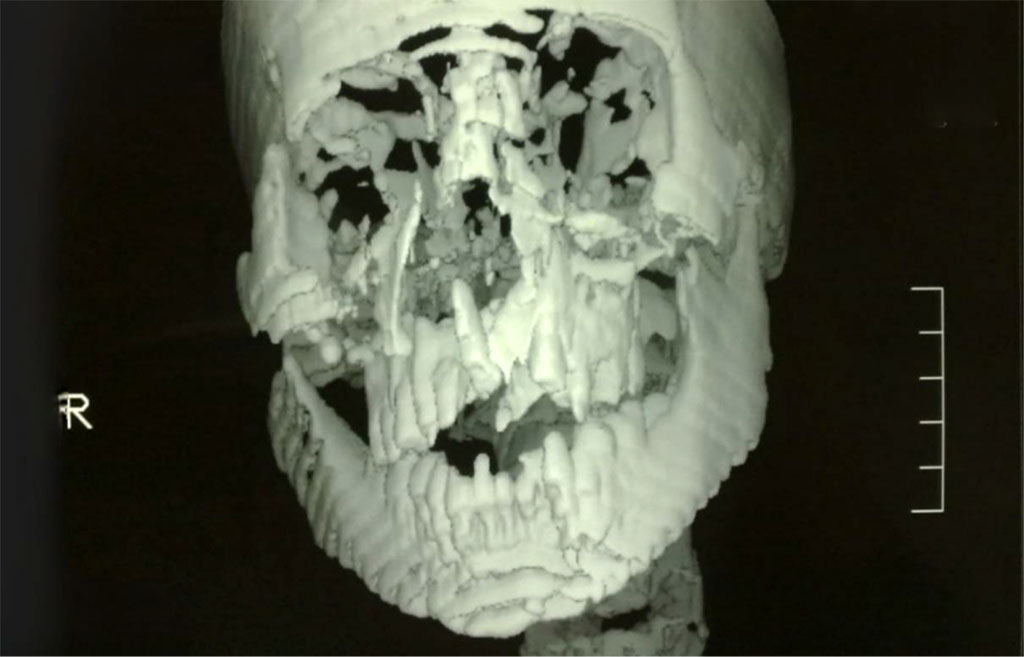
Figure 2: MDCT showing the maxillary Le Fort I and the left parasymphysial mandibular fractures.
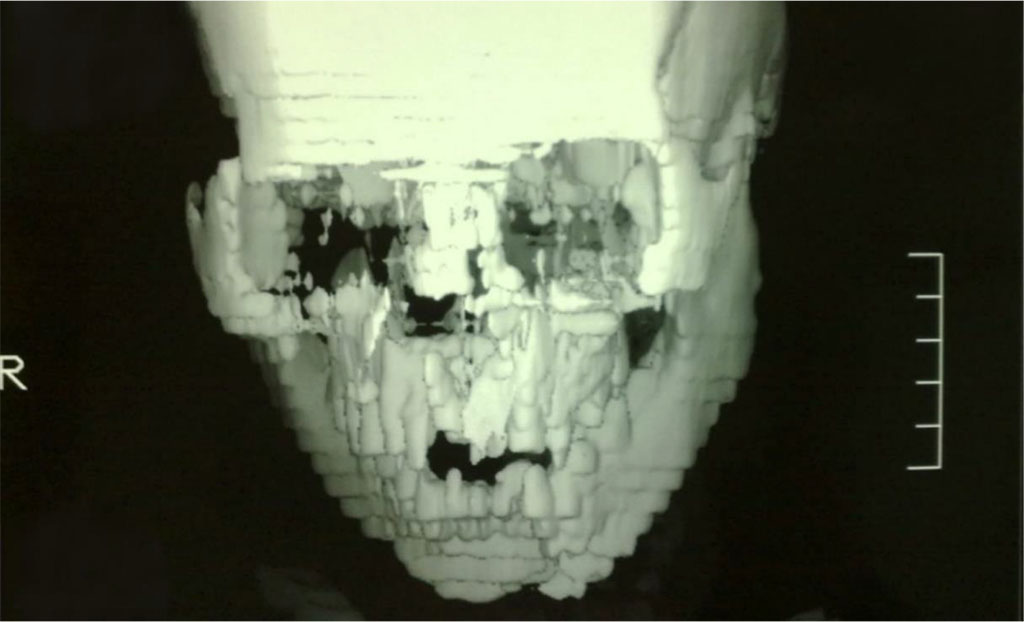
Figure 3: MDCT showing the maxillary Le Fort I and the left parasymphysial mandibular fractures.

Figure 4: The trans-maxillary wire (The white arrow).
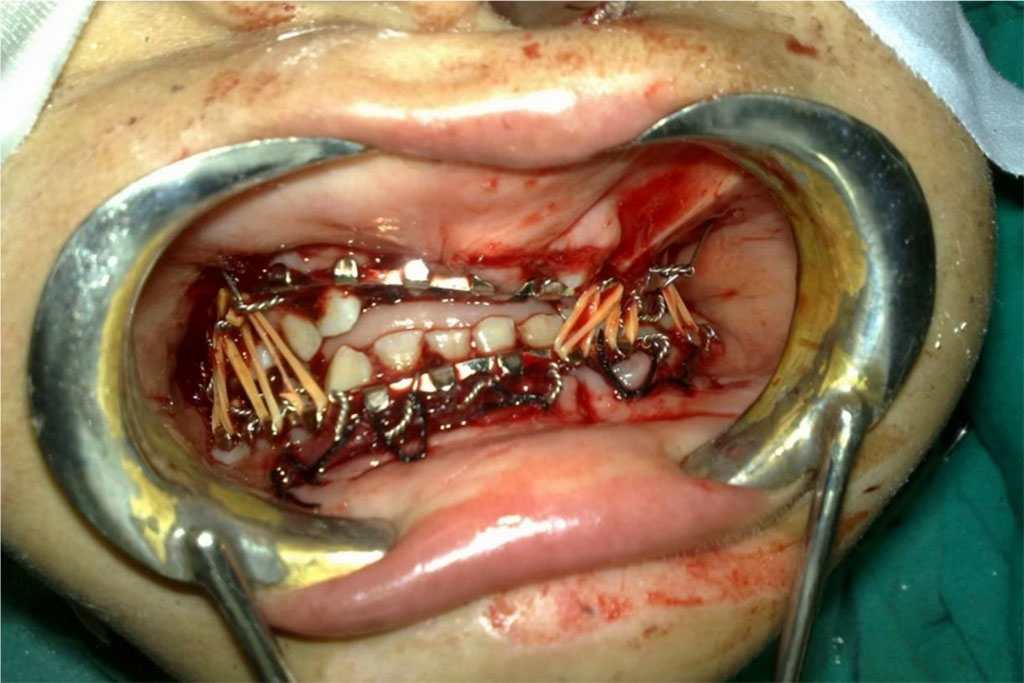
Figure 5: Manduiblo-maxillary fixation and closing the oral cavity using elastic materials stretched in between the hooks mandibular and maxillary arch bars.
Operative-time was 45 minutes.
Postoperatively: the patient started oral feeding after three hours; fluids then semisolids. No fever. Pain was controlled by PerfalganTM infusion. Plain skull x-rays (Town and lateral views) revealed proper reduction, optimal mandibular occlusion without any complications e.g., malunion or non-union [Figure 6,7]. The patient was discharged on the fifth day.
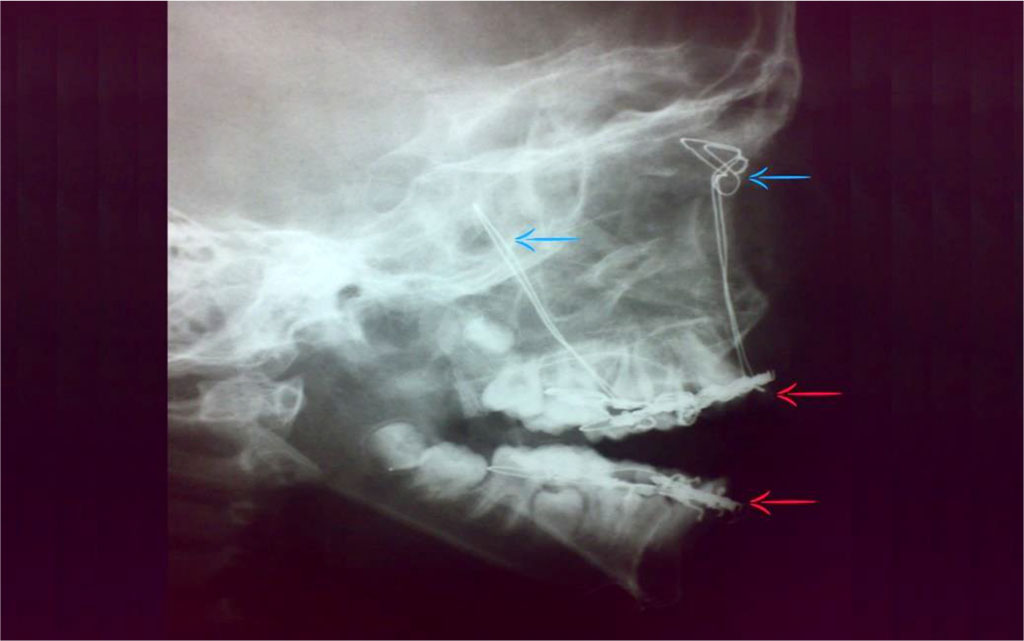
Figure 6: Postoperative plain skull x-ray (lateral view); Frontal suspension (blue arrows) and Manduiblo-maxillary fixation (red arrows).

Figure 7: Postoperative plain skull x-ray (Town view); Frontal suspension (blue arrows), Manduiblo-maxillary fixation (white arrows) and interosseus wire (red arrow).
During sort-term follow-up; the patient showed no complains or complications. The sutures were removed after ten days. The frontal suspension, trans-maxillary wire and arch bars were removed after one month, while the interosseous wire was not removed [Figure 7]. The patient was referred to a pediatric orthodontist for further follow-up.
We successfully restored functional, anatomical and cosmetic aspects in our patient: no complications were reported. Combined closed reduction and interosseous wire for open reduction and internal fixation (ORIF) in the absence of other facilities; biodegradable plates (pediatric) and titanium miniplates (for adults) was an optimal and cost-effective choice for pediatric facial fractures. Our conclusion was consistent with the study by Pereira I. et al [10]. There is always a search for other safe, cost-effective alternatives for ORIF where optimal results are combined with minimal drawbacks. Further investigations are needed.
Authors have no conflict of interest to declare.
This publication was prepared without any external source of funding.
Sameh Salem, Mekhaeel Mekhaeel, Andrey Protasov – conceptualization. Sameh Salem, Mekhaeel Mekhaeel, Andrey Protasov, Nada Taha, Mohamed Arafa, Salma Noureldin - writing original draft and review. Sameh Salem, Mekhaeel Mekhaeel, Andrey Protasov – editing. project administration; Salem Sameh, Mekhaeel Mekhaeel, Andrey Protasov, Nada Taha, Mohamed Arafa, Salma Noureldin. Sameh Salem, Mekhaeel Mekhaeel, Andrey Protasov – visualization, Sameh Salem, Mekhaeel Mekhaeel, Andrey Protasov – supervision.