- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 4. DOI 10.35630/2024/14/4.405
Introduction: Intramuscular myxoma is a rare benign soft tissue tumor which usually affects large muscle groups in patients aged between forty and sixty years. It is composed of hypocellular myxoid tissue. Incidence of intramuscular myxoma varies from 0.1 to 0.3 per 100,000 individuals.
The aim of this study: to present the process of diagnosis and treatment of a patient with the rare soft tissue tumor.
Case description: A 41-year-old female came to the Orthopedic Clinic with a 2-year history of a lump on the lateral side of her right thigh. Noticeable growth of the lesion and pain complaints started after skiing injury 7 months before the examination. The magnetic resonance imaging test demonstrated encapsulated intramuscular mass which measured 6 x 2 x 2 cm located in Vastus lateralis muscle. Due to an increasing pain and a significant size of the lesion, the patient was qualified for an excisional biopsy. After an excision, the lesion was found on histopathology to be an intramuscular myxoma. The patient did not complain of any neurological deficits, walking disorders. The follow-up imaging examination 3 months after surgery show no recurrence and the further observation was planned.
Myxomas were initially documented by Virchow in the year 1871 [15]. They are classified among benign tumors occurring within muscles, bones, urogenital tract, skin, subcutaneous and aponeurotic tissues. The most frequent - intramuscular myxomas, affect larger muscle groups. Predominantly found in cardiac muscles, they constitute about half of all benign lesions in this area [1, 2]. Another common sites are thigh muscles, while less common locations include arm, upper limb girdle, trunk, buttocks [14, 20, 21]. Their annual incidence is approximately one in a million, with a higher prevalence among individuals aged forty to sixty, particularly women, as in the presented case description [3, 14].
Myxomas consist of spindled and stellate-shaped cells with a significant presence of mucoid substance between them (Figure 1) [23].
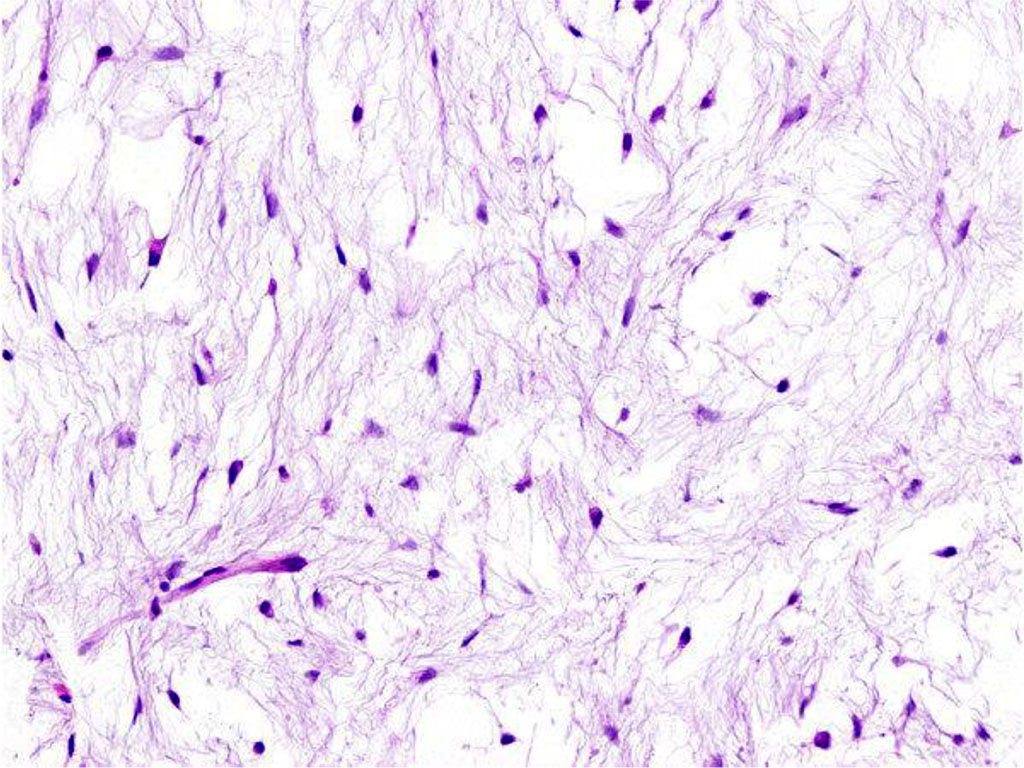
Figure 1. Histologic finding of intramuscular myxoma. The tumour is composed of spindle and stellate-shaped cells in an abundant myxoid stroma.
They develop from primitive mesenchymal cells that lose their ability to produce collagen but instead produce excessive hyaluronic acid and immature collagen fibers [4, 10]. Myxomas share similarities with other pseudosarcomatous lesions, often mimicking soft tissue sarcomas due to their cellular abnormalities, and increased mitotic activity, which can lead to misdiagnosis despite their benign nature. Treatment primarily involves complete surgical removal of the lesion.
The aim of this study was to present the process of diagnosis and treatment of a patient with the rare soft tissue tumor. Incidence of intramuscular myxoma varies from 0.1 to 0.3 per 100,000 individuals.
A 41-year-old female came to the Orthopedic Clinic with a 2-year history of a lump on the lateral side of right thigh. Noticeable growth of the lesion and pain complaints started after skiing injury 7 months before the examination. There was no history of soft tissue neoplasms in either the patient or her family. During the physical examination, there was an area of swelling in the right thigh, which was tender upon palpation. The swelling was about several centimeters in size, with a solid texture, and could be moved vertically. The skin above it appeared normal. No similar swellings were found elsewhere, and her overall health was good.
The patient came with laboratory tests and ultrasound results which were performed some time earlier. Laboratory investigation, including a complete blood count, prothrombin time C-reactive protein test showed no abnormalities. Ultrasound examination revealed a well-defined, oval-shaped area of reduced echo intensity within the muscle tissue. Further, more detailed imaging was planned. Magnetic resonance imaging (MRI) confirmed the presence of the tumor. The tumor measured about 6 cm in length, 2 cm in width, and 2 cm in sagittal diameter. It appeared hyperintense on T2-weighted images (Figure 2A, Figure 3A) and hypointense (resembling fluid) on T1-weighted images (Figure 2B, Figure 3B).

Figure 2. (A) Coronal MRI section showing high signal intensity on T2-weighted imaging in oval-shaped lesion in the Vastus lateralis. (B) Coronal MRI section showing low signal intensity on T1-weighted imaging in oval-shaped lesion in the Vastus lateralis.
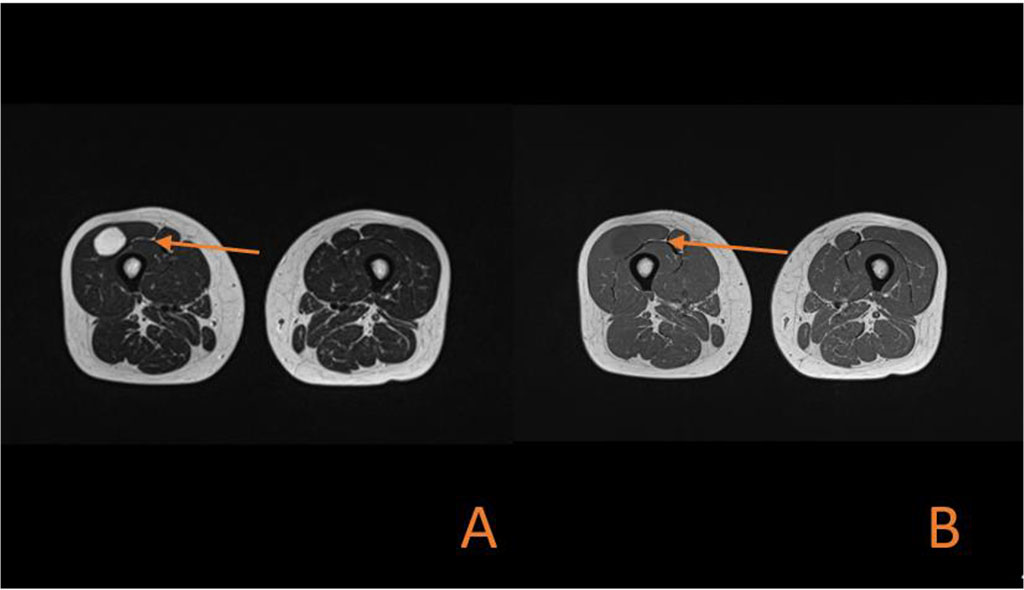
Figure 3. (A) Axial MRI section showing high signal intensity on T2-weighted imaging in oval-shaped lesion in the Vastus lateralis. (B) Axial MRI section showing low signal intensity on T1-weighted imaging in oval-shaped lesion in the Vastus lateralis.
An observation of the lesion and a pre-operative core biopsy were not taken into consideration because of growing pain reported by the patient and significant size of the lesion. The patient was qualified for an excisional biopsy. During surgery under spinal anaesthesia encapsulated tumor was completely excised. A tissue sample was collected and sent for histopathological evaluation. The patient had no complications after the surgery - any neurological deficits, walking disorders. The patient was discharged from hospital after 2 days. The histopathological examination of the surgical specimen confirmed the diagnosis of an intramuscular myxoma. The follow-up imaging examination 3 months after surgery show no recurrence and the further observation was projected.
The aetiology of intramuscular myxoma is identified incompletely [5]. There is evidence suggesting its association with mutations in the GNAS (guanine nucleotide binding protein, alpha stimulating) gene [5, 6].
Mazabraud syndrome should be considered if intramuscular myxoma is suspected . This is a rare condition characterized by the presence of fibrous dysplasia and intramuscular myxomas [7, 16, 17, 18].
Obtaining a definitive diagnosis of intramuscular myxoma through non-invasive diagnostic methods is challenging, as the tumor manifests with nonspecific clinical symptoms and can be easily misinterpreted as other tumors in imaging studies such as X-ray, ultrasound, computed tomography (CT scan) and MRI. X-ray examinations may reveal a normal appearance or demonstrate a nonspecific intramuscular mass rarely containing calcifications [8, 9]. Ultrasound examinations typically depict an intramuscular myxoma as a well-defined, hypoechoic or heteroechoic mass [10, 11]. CT scans usually reveal a well-defined, homogeneous, low-density lesion [10, 12, 13 ]. MRI images present an IM as a hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted images [13]. MRI imaging seems the most accurate imaging as a method of planning resection of tumour.
Macroscopically, the neoplasm typically exhibits an elliptical shape and presents a distinct profile. Nonetheless, the fibrous capsule may be deficient and penetrate the adjacent muscles[20, 22] . Recurrences following incomplete excision have been documented [13, 19]. Therefore, excising the tumor along with the surrounding muscle is advised if the macroscopic margin is ambiguous. The follow-up imaging examinations are recommended even though intramuscular myxomas lack malignant potential and do not display metastatic tendencies [8].
Intramuscular myxoma should be differentiated early from malignancies, especially sarcomas and metastasis. The magnetic resonance imaging is used to plan resection of the lesion. A definitive diagnosis is only made post-surgery through histopathological analysis of intraoperative biopsy.