- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 4. DOI 10.35630/2024/14/4.416
Purpose of the Study: To evaluate the effectiveness of photodynamic therapy in the treatment of post-acne scars.
Materials and Methods: We have presented a clinical case of the correction of post-acne with photodynamic therapy after a preliminary course of systemic retinoids. A 23-year-old patient with a 10-year history of acne lesions was diagnosed with severe acne complicated with atrophic scars and dyschromia.
Results: The use of photodynamic therapy with an external gel, a photosensitizer based on chlorin E6, proved to be highly effective in correcting the post-acne complications. The use of a personalized approach when determining the exposure of the gel on the skin established its highest concentration after 10 minutes and the optimal duration of irradiation within 10 minutes. As a result of treatment, there was a restoration of skin color and a decrease in the depth of atrophic scars.
Conclusions: This case is of interest to dermatologists/aesthetic physicians, since an effective method of using photodynamic therapy with a topical photosensitizer gel in the correction of post-acne scars was proposed.
Keywords: acne, post-acne, atrophic scars, dyschromia, photodynamic therapy
Acne is the most common dermatosis seen by a dermatovenerologist, which is a chronic, recurrent disease of the sebaceous glands and hair follicles, manifested by open or closed comedones, inflammatory lesions in the form of pustules and papules. In 85% of patients, acne occurs between the ages of 12 and 24 years, in 8% in the age group from 25-34 years and in 3% in the age group from 35 to 44 years [1]. To determine the severity of dermatosis, the dermatological acne index (DAI) is used, which calculates the number of comedones, papules, pustules and nodules on the facial skin. In mild cases, inflammatory elements are detected from 1 to 5, moderate - from 6 to 10, severe - from 11 to 15 [2].
Complications of post-acne include: dyschromia, scarring (both atrophic and hypertrophic) and stagnant erythema [3].
Goodman-Baron scale is used to assess acne scars (by J. Goodman, J. A. Baron, 2006) which is a quantitative and qualitative indicator and is determined on the skin of the face before and after treatment, expressed in points [4]. A score of 1 point is given for a patchy lesion with erythematous hyper- or depigmented flat scars, without changing the skin texture; 2 points - with a lower level of damage, when atrophic or hypertrophic scars are not significantly expressed, and not visible from a distance of 50 cm or more, and are corrected with camouflage cosmetics; 3 points - for clearly visible atrophic or hypertrophic scar changes from a distance of 50 cm or more, poorly masked by foundation and the shadow of closely spaced hair, 4 points - for atrophic scars that do not smooth out with skin tension and pronounced hypertrophic changes [4].
The GAIS scale is used to assess the clinical effectiveness of treatment (Global Aesthetic Improvement scale). The results of the procedure are assessed with points from -1 to 3, individually by the doctor and the patient. In this case, -1 point means deterioration compared to the initial state; 0 points – no effect from the procedure (the condition is the same as before the treatment); 1 point—insignificant improvement requiring additional correction; 2 points - pronounced effect, but further correction is still possible; 3 points – optimal cosmetic result, with which the patient is completely satisfied [5].
Photodynamic therapy is a technique that includes the use of an external photosensitizer gel and laser radiation. The wavelength of laser radiation corresponds to the peak absorption of the photosensitizer in the skin. Thanks to the use of a local (external) photosensitizer that does not have a phototoxic or irritating effect on the skin, and radiation sources for its activation, based on ultra-bright LEDs, new opportunities have emerged for the use of photodynamic therapy in dermatovenerology and cosmetology. Cytotoxicity, which occurs during a photochemical reaction, causes necrosis or apoptosis of the pathogenic cell. Apoptosis occurs as a result of oxidative destruction of mitochondria, and necrosis occurs as a result of destruction of the cell membrane. The body's response after damage is aimed at removing cellular debris, damaged tissue and regenerating surrounding structures. Photodynamic therapy helps restore the collagen framework and skin pigmentation, as well as improve microcirculation. The main advantages of this method are the activation of the growth of young, healthy cellular structures, collagen and elastin, the painlessness and non-invasiveness of the procedure, the absence of a rehabilitation period and side effects [6, 7, 8].
We present a clinical case report of successful acne treatment. Patient I., 23 years old, in September 2022 consulted a dermatologist with complaints of rashes on the skin of the face and neck.
The rashes first appeared at the age of 13. The patient used self-medicated with topical remedies, without significant effect. In 2023, he consulted a dermatologist, where he was diagnosed with severe acne, with complications in the form of atrophic scars and dyschromia (L .70).
The pathological process is localized on the skin of the face in the forehead, cheeks, chin, front and side surfaces of the neck. The prevalence of the rash is disseminated. The inflammatory reaction is acute. Primary morphological elements are represented by pustules and papules, bright red in color with a bluish tint, hemispherical in shape, present over a background of erythema. Manifestations of post-acne on a G scale by J. Goodman, J. A. Baron were rated 4 points. [4].
The following treatment was carried out: isotretinoin 40 mg per day, according to a scheme with gradual withdrawal of the drug over 11 months, clindamycin orally 150 mg 4 times a day for 14 days [1,9]. For external treatment, clindamycin gel was used once a day for 2 months in combination with moisturizing creams to reduce skin dryness (as a side effect of systemic retinoids).
After treatment of acne on the facial skin in the forehead, cheeks, chin, and neck, post-acne changes remained in the form of atrophic scars and dyschromia. To correct these complications, the patient underwent a course of photodynamic therapy. An external gel was used as a photosensitizer, the active substance of which is N - dimethylglucamine chlorine E6, obtained by extracting chlorophyll A from the marine microalgae spirulina and its subsequent chemical transformation using an original technology [6]. To activate the photodynamic reaction, red laser radiation in the range of 660±2 nm was used [10]. For the purpose of a personalized approach, the concentration of the photosensitizer gel was determined for the patient at various exposures (Table No. 1, Fig. 1 - a, b, c, d, e).
Table 1. Determination of the concentration of a photosensitizer gel in scar tissue at various exposures
| No. | Gel exposure (in minutes) | Gel concentration indicators (in units) |
| 1 | 5 | 0.199 |
| 2 | 10 | 0.659 |
| 3 | 15 | 0.754 |
| 4 | 20 | 0.707 |
| 5 | 25 | 0.539 |
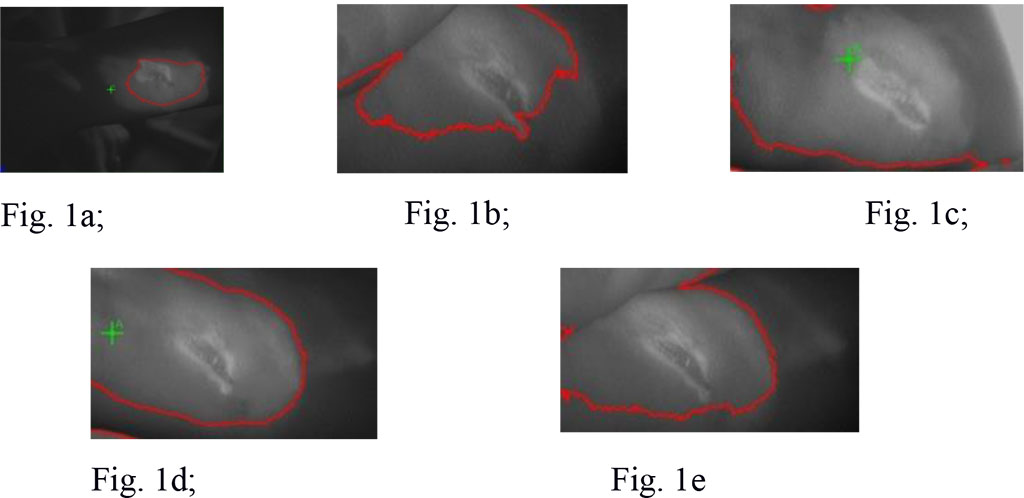
Figure 1. Gel concentration in scar tissue at
various exposures
Figure 1a. Gel
concentration after
5 minutes
Figure 1b. Gel
concentration after
10 minutes
Figure 1c. Gel
concentration after
15 minutes
Figure 1d. Gel concentration after 20 minutes
Figure 1e. Gel concentration after 25 minutes
Thus, the highest concentration of the gel and the highest expected effect of the photodynamic reaction were determined in an interval of 10-20 minutes, which indicates the validity of applying the gel for 10 minutes and its subsequent activation by laser radiation for 10 minutes.
The facial skin was previously cleansed with an aqueous solution of chlorhexidine. The gel was applied to dry skin under occlusion and left for 10 minutes, then washed off with water and gel/foam, and the pores were thoroughly cleaned of the photosensitizer. Next, the entire treated surface was irradiated using a laser device with a power density of 100 mW/ cm, a light dose of 120–140 J/ cm² for 10 minutes. The wavelength of laser radiation corresponded to 660 nm, the area of the light beam was 400–800 cm². Photodynamic therapy sessions were carried out once a week, with a total course of 10 procedures [11,12,13].
After a course of photodynamic therapy, the patient experienced smoothing of scars, leveling of skin relief and color, as well as an increase in skin turgor and elasticity, and a decrease in dryness. Manifestations of post-acne on a G scale. J. Goodman, J. A. Baron were rated at 2 points. The clinical effectiveness of treatment on the GAIS scale was 3 points (Fig. 2 - a, b, c). The obtained result was maintained over a 12month observation period.
Treatment with systemic retinoids (isotretinoin) in combination with a topical gel (clindamycin) resulted in clinical resolution of acne. However, in severe forms, scarring changes, dyschromia, increased dryness, decreased elasticity and turgor of the skin remain after treatment. The use of photodynamic therapy with an external gel, a photosensitizer based on chlorin E6, proved to be highly effective in correcting these post-acne complications. The use of a personalized approach when determining the exposure of the gel on the skin established its highest concentration after 10 minutes and the optimal duration of irradiation within 10 minutes. This case is of interest to dermatologists and cosmetologists, since it illustrates the feasibility of photodynamic therapy as a new method for correcting post-acne skin changes.